5 Pelvis Inspect for deformity, lower extremity malrotation, leg length discrepancy, increased/decreased lordosis, pelvic obliquity. Palpate anterior and posterior landmarks: Palpate the abdomen for masses or hernias. Neurovascular Examination: Table 5-1. Table 5-1. Table 5-2. • Pregnancy (hormones and pelvic stress increase mobility in SI joint) • Trauma/motor vehicle collision (foot on the brake during collision) • Conservative measures must be tried and must have failed. • Pain relief from fluoroscopically guided lidocaine/steroid injection must be documented. • Other causes such as herniated disk, spinal stenosis, degenerative disk disease, piriformis, or hip disorders must be ruled out. • If criteria are met, the patient will undergo an SI joint fusion, which involves the manual manipulation of the SI joint into anatomic position and then using screws across the joint to fuse the R and L ilea to the sacrum using a posterior approach. Obtain a postoperative radiograph of the AP pelvis and lateral hip and lumbar spine. • The patient does not need to be immobilized and will start PT at 3 weeks for rehabilitation. Follow up with the patient in 6 weeks for repeat radiographs. Osteitis pubis is the inflammation of the pubic symphysis. The etiology is unclear, although it was first described in patients who had undergone subrapubic surgery and later linked to athletes. Inflammation is caused by microtrauma to the adductors or lower rectus muscles, which increases shear forces across the pubis symphysis.
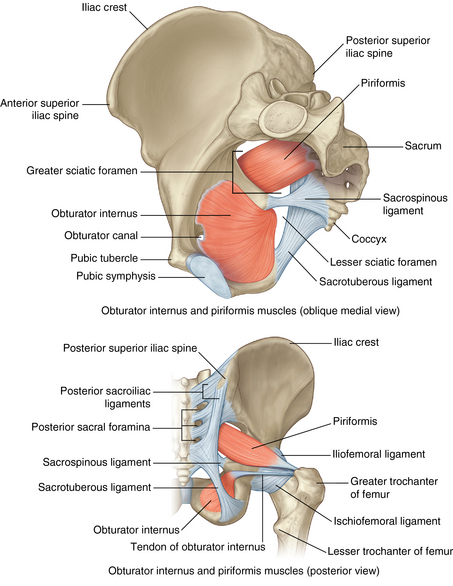
Anatomy
Physical examination
NERVE/VESSEL
LOCATION
Femoral artery
Inferior to inguinal ligament; halfway between the anterior superior iliac spine and the pubic tubercle
Cluneal nerve
Iliac crest between the posterior superior iliac spine and the iliac tubercle
Sciatic nerve
Midway between the greater trochanter and the ischial tuberosity
 Fabere test: Test for SI joint or hip pathology. With the patient lying supine, place the foot of the involved side on the opposite knee. Inguinal pain, in this position, suggests hip pathology. With one hand on the knee and the other hand on the ASIS, apply pressure; increased pain suggests SI joint pathology.
Fabere test: Test for SI joint or hip pathology. With the patient lying supine, place the foot of the involved side on the opposite knee. Inguinal pain, in this position, suggests hip pathology. With one hand on the knee and the other hand on the ASIS, apply pressure; increased pain suggests SI joint pathology.
 Trendelenburg sign: Ask the patient to stand and lift one leg (flex hip). The flexed side of the pelvis should elevate. If the pelvis falls, there is abductor or gluteus medius dysfunction.
Trendelenburg sign: Ask the patient to stand and lift one leg (flex hip). The flexed side of the pelvis should elevate. If the pelvis falls, there is abductor or gluteus medius dysfunction.
 FAIR test: Flexion Adduction Internal Rotation with patient in the lateral recumbent position with the affected side up reproduces gluteus pain, suggesting piriformis syndrome.
FAIR test: Flexion Adduction Internal Rotation with patient in the lateral recumbent position with the affected side up reproduces gluteus pain, suggesting piriformis syndrome.
Differential diagnosis: Table 5-2
Anterior pelvic pain
Pubic rami fracture, acetabular fracture, femur fracture, pubic symphysis disruption, iliopsoas tendonitis/bursitis, hip arthritis, femoral acetabular impingement (FAI), lumbar radiculopathy, nonorthopaedic causes (e.g., intra-abdominal, gynecologic, genitourinary)
Lateral pelvic pain
Greater trochanter bursitis, FAI
Posterior pelvic pain
Sacral fractures, sacroiliac joint arthritis/dislocation/fracture, piriformis syndrome, lumbar radiculopathy
Sacroiliac dysfunction
 Complaints of pain in the lower back exacerbated by prolonged sitting, twisting, or hyperextending the back
Complaints of pain in the lower back exacerbated by prolonged sitting, twisting, or hyperextending the back
 Difficulties getting in or out of a car, putting on shoes, or turning over in bed
Difficulties getting in or out of a car, putting on shoes, or turning over in bed
Physical examination
 Thrombotic thrombocytopenic purpura (TTP) is evident at the SI joint.
Thrombotic thrombocytopenic purpura (TTP) is evident at the SI joint.
 Perform a Gillet or “stork” test. (Ask the patient to stand with his or her back to the examiner while the examiner places his or her thumbs at the SI joint and has the patient flex each hip, individually. A positive test will cause the thumb ipsilateral to the flexed hip to either remain still or move cranially. If the thumb moves caudally, this indicates a negative test.)
Perform a Gillet or “stork” test. (Ask the patient to stand with his or her back to the examiner while the examiner places his or her thumbs at the SI joint and has the patient flex each hip, individually. A positive test will cause the thumb ipsilateral to the flexed hip to either remain still or move cranially. If the thumb moves caudally, this indicates a negative test.)
Imaging
 Order a radiograph of the pelvis (Fig. 5-2): anteroposterior (AP) and lateral to evaluate for sclerosis.
Order a radiograph of the pelvis (Fig. 5-2): anteroposterior (AP) and lateral to evaluate for sclerosis.
 Bone scans may indicate areas of stress; magnetic resonance imaging (MRI) may reveal synovitis or tumors.
Bone scans may indicate areas of stress; magnetic resonance imaging (MRI) may reveal synovitis or tumors.
 The gold standard is a lidocaine/steroid injection under fluoroscopy to the SI joint, which may be both diagnostic and therapeutic.
The gold standard is a lidocaine/steroid injection under fluoroscopy to the SI joint, which may be both diagnostic and therapeutic.
Initial treatment
 The junction of the sacrum with the right and left ilea forms the SI joint. It is designed for stabilization, twisting, and load transference to the lower body. It is a small joint and only allows for minimal movements. Pain is usually derived from hypermobility or instability of the joint. Treatment is geared toward stabilization of the joint and relieving pain and inflammation.
The junction of the sacrum with the right and left ilea forms the SI joint. It is designed for stabilization, twisting, and load transference to the lower body. It is a small joint and only allows for minimal movements. Pain is usually derived from hypermobility or instability of the joint. Treatment is geared toward stabilization of the joint and relieving pain and inflammation.
Treatment options
 Most patients will recover with conservative therapy that includes the following:
Most patients will recover with conservative therapy that includes the following:
Operative management
 Criteria for SI joint stabilization
Criteria for SI joint stabilization
Osteitis pubis
Physical examination
 A waddling gait is noticeable.
A waddling gait is noticeable.
 Tenderness to palpation presents over the pubic symphysis.
Tenderness to palpation presents over the pubic symphysis.
 Α “single leg hop” may reproduce pain.
Α “single leg hop” may reproduce pain.
 Compression of greater trochanters bilaterally causes pain at the pubic symphysis.
Compression of greater trochanters bilaterally causes pain at the pubic symphysis.
 Weakness at hip adductors or flexors is evident.
Weakness at hip adductors or flexors is evident.
 Evaluate for SI joint dysfunction, which can contribute to instability of the pubic symphysis.
Evaluate for SI joint dysfunction, which can contribute to instability of the pubic symphysis.
Pelvis