Pelvic Fixation with Sacral-Alar-Iliac Screws in Neuromuscular Scoliosis
Jaysson T. Brooks
Paul D. Sponseller
The Galveston technique, the first widely used form of pelvic fixation, was developed by Allen and Ferguson in the 1980s. This technique involved using an L-shaped rod inserted at the posterior superior iliac spine between the inner and outer tables of the ilium, improving caudal fixation in long posterior spinal fusions. Since then, a variety of other pelvic fixation methods have been developed, including the unit rod, Jackson intrasacral rod, and the iliosacral screw (1, 2). Unfortunately, these options often required substantial soft-tissue dissection and were often complicated by prominence and back out. These issues led to the development of the sacral-alar-iliac (SAI) screw (3, 4, 5), which is commonly used for pelvic fixation in patients with neuromuscular scoliosis (NMS). The advantages of SAI pelvic fixation compared with other methods are that (a) the starting point is on the sacrum, avoiding the soft-tissue dissection needed for a posterior superior iliac spine starting point; (b) the starting point is 1.5 cm deeper beneath the skin surface; (c) the SAI screws extend well past the lumbosacral pivot point, resulting in a marked increase in construct stiffness; and (d) the more laterally directed screw trajectory leads to less back out. The following text will describe when and how to use pelvic fixation with SAI screws.
INDICATIONS
The primary goal of performing posterior spinal fusions on patients with NMS is to improve their sitting balance and posture. Unlike patients with idiopathic scoliosis, selective thoracic fusions and fusions short of the pelvis are rarely indicated in this patient population. All patients with NMS should be considered for pelvic fixation unless they have trunk control, an end Cobb vertebra above L3, and a horizontal L4 and pelvis in sitting or standing, with Gross Motor Function Classification System levels of I through III. Thus, patients with NMS who are able to sit independently with a balanced pelvis may not require fusion to the pelvis, particularly if it would limit their function. Severe sacropelvic dysplasia complicates but does not contraindicate the SAI technique.
PREOPERATIVE PLANNING
Preoperative planning involves the standard evaluation of history, physical examination, and radiographic data. In this particular patient population, there are four specific issues to consider. First, it is important to understand the degree of transverse plane asymmetry present within the pelvis as this may alter the previously planned trajectory for SAI screw insertion (6). An iliac wing that appears narrower on the radiograph will pose more of a challenge in insertion. It is also important to identify the presence and laterality of any baclofen pumps (Medtronic, Inc., Minneapolis, MN) because they will need to be protected during the approach to the spine. Second, it is important to consider whether preoperative halo traction or intraoperative traction is needed. Patients with Cobb angles of more than 110 degrees or severe proximal thoracic curves sometimes benefit from preoperative traction. Some degrees of pelvic obliquity can be corrected with distal traction, using the skin traction method if hip or knee contractures are not too severe. Third, while extension of the fusion down to the pelvis is planned, it is equally important to consider how far cephalad to extend the fusion. As a general rule, all vertebrae within the main coronal and sagittal curves and any proximal thoracic curve larger than 30 to 35 degrees should be included in the fusion. Fourth, it is important to plan whether correction of the patient’s deformity will occur from caudad to cephalad or cephalad to caudad. Unless the patient has a severe proximal thoracic curve, correction from caudad to cephalad is preferred.
SURGICAL PROCEDURE
Positioning
The patient is positioned prone on a modified Jackson table. Frequently, the patient’s legs are placed in a sling, which can be adjusted to control intraoperative lordosis after the posterior supporting structures are removed. A standard approach is made down to the spinous processes; the surgeon should make sure he/she is aware of the presence and laterality of any implanted baclofen pumps. When the exposure is complete, there should be adequate visualization of the S1 vertebral body, the sacral ala, and the S1 and S2 posterior foramina.
Placement of S1 Screws
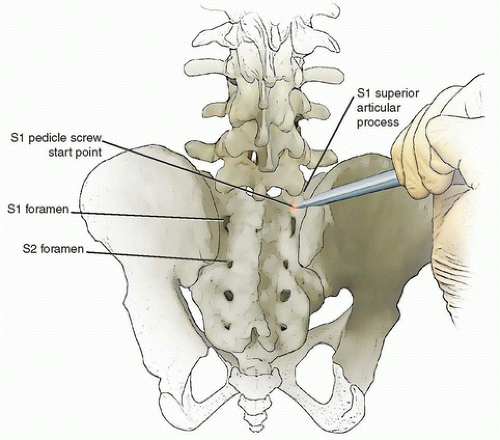
The S1 screws are usually placed before the SAI screws, and the starting point is at the base of S1 superior articular process (Fig. 46-1). The trajectory should be aimed medial approximately 25 degrees and toward the anterior aspect of the sacral promontory; this position achieves
a “tricortical” fixation, which increases the pullout strength. When placing the S1 screw, it is important to have a correct three-dimensional understanding of the anatomy based on the position of the pelvis. With the patient on a modified Jackson table and the legs in a padded sling, the anterior lip of the sacral promontory is tilted caudally. Imaging or navigation can help confirm this position if needed. Once the three-dimensional position of the pelvis is better understood, it will be clear that the correct trajectory of the S1 screw appears more parallel with the sacral plateau than with the vertical plane (Fig. 46-2). Once the S1 screw is correctly inserted, its position can be confirmed using a lateral image via fluoroscopy; however, with experience, doing so is rarely necessary.
a “tricortical” fixation, which increases the pullout strength. When placing the S1 screw, it is important to have a correct three-dimensional understanding of the anatomy based on the position of the pelvis. With the patient on a modified Jackson table and the legs in a padded sling, the anterior lip of the sacral promontory is tilted caudally. Imaging or navigation can help confirm this position if needed. Once the three-dimensional position of the pelvis is better understood, it will be clear that the correct trajectory of the S1 screw appears more parallel with the sacral plateau than with the vertical plane (Fig. 46-2). Once the S1 screw is correctly inserted, its position can be confirmed using a lateral image via fluoroscopy; however, with experience, doing so is rarely necessary.
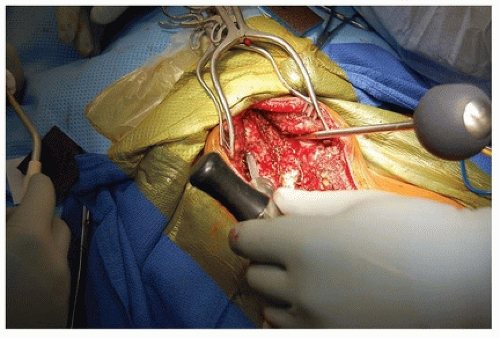
Placement of SAI Screws
The starting point for placement of SAI screws is the area between the S1 and S2 foramina, that is, slightly more medial and distal to the S1 foramen (Fig. 46-3). With a starting awl or burr, the SAI screw pathway is created using a trajectory angled 40 degrees lateral and 40 degrees caudal. In patients who do not have substantial intrapelvic asymmetry or hip dislocations, the surgeon can place a hand on the patient’s greater trochanter to help guide the correct trajectory as the awl is advanced toward the hand, or in thin patients, the outer table of the iliac crest can




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree