Pedicle Screw Insertion— Manual and Power Techniques
David B. Bumpass
Ronald A. Lehman Jr
Lawrence G. Lenke
INDICATIONS/CONTRAINDICATIONS
Pedicle screws are a versatile option for posterior instrumentation of the pediatric thoracic and lumbar spine. Screw-based constructs are useful for both fusion and growing spine deformity techniques. Over the past decade, numerous studies have demonstrated that pedicle screws are safe and effective for treating pediatric spine deformities and hold significant biomechanical advantages over hook or hybrid hook-screw constructs (1). Stable fixation can be obtained in most pedicles using screws, even those of small diameter. Contraindications are few but include pedicle erosion by significant dural ectasia in patients with neurofibromatosis or Marfan syndrome; in such cases, pedicle screws are still typically used above and below the areas of dural ectasia, with rods spanning the most affected levels. In addition, some surgeons may not be comfortable placing pedicle screws into tiny type D (slitlike) pedicles, and this relative contraindication should be respected to keep the overall use of pedicle screws as safe as possible during pediatric spinal surgery (2).
PREOPERATIVE PREPARATION
On physical examination, standing coronal and sagittal spinal balance should be noted. Shoulder balance, rib prominence, truncal shift, and pelvic obliquity also must be assessed. Having the patient lie prone on the examination table is useful to determine scoliosis flexibility; a push-prone maneuver can also be done to further examine flexibility. For kyphotic patients, having the patient lie supine or prone is very useful to visualize how much passive correction can be achieved. A thorough neurologic exam to detect motor and sensory deficits as well as signs of myelopathy must be performed prior to deformity correction. The skin of the back should also be inspected for acne or previous incisions.
The patient’s preoperative radiographs should be reviewed in detail prior to beginning surgery. Pedicle morphology should be assessed on a full-length anterior-posterior (AP) spine radiograph— there is significant variability in pedicle diameter between patients, and the surgeon should have an excellent understanding of the vertebral morphology prior to starting the surgery. In scoliotic patients, pedicle diameter is affected by whether the pedicle is located on the concavity or convexity
of a curve. Studying the preoperative supine coronal radiograph is very helpful, as the pedicles are always more visible due to having less curvature, rotation, and movement when the radiograph is taken without gravity. In addition, the severity of vertebral rotation can be ascertained from the AP radiograph. The lateral radiograph is useful to estimate desired pedicle screw length.
of a curve. Studying the preoperative supine coronal radiograph is very helpful, as the pedicles are always more visible due to having less curvature, rotation, and movement when the radiograph is taken without gravity. In addition, the severity of vertebral rotation can be ascertained from the AP radiograph. The lateral radiograph is useful to estimate desired pedicle screw length.
For pediatric patients with complex deformities, such as severe scoliosis, previous fusions, or a congenital osseous abnormality, a preoperative thoracolumbar computed tomography (CT) scan is typically obtained. While recognizing the need to minimize radiation in children, CT imaging is extremely useful for studying pedicle diameter and morphology, plotting screw length, and creating three-dimensional reconstructions of the spine to fully understand the orientation of each segment of the deformity.
Magnetic resonance imaging is obtained in patients with significant kyphosis, a sharp angular or rapidly progressing scoliosis, an atypical curve pattern such as a left-sided scoliosis, or a known history of Chiari malformation or spinal dysraphism. Knowing whether a patient is at higher risk for neurologic deficit is a critical step in preoperative planning regarding implant selection and correction strategy.
Pedicle screws can be placed using a freehand technique based on posterior spinal anatomic landmarks; alternatively, screw placement can be guided using intraoperative fluoroscopy or CT-based navigation. One advantage of the freehand technique is minimization of radiation exposure. For surgeons who do not place a high volume of pedicle screws or are accumulating experience, using fluoroscopy or navigation might be helpful to minimize complications, as studies have noted a high learning curve for the freehand technique (3). Surgeons should use the technique they feel is safest and most efficacious for the patient. However, understanding the local osseous and neural anatomy necessary for placing screws without any image guidance will help all surgeons during whatever technique they choose. The remainder of this chapter will present the freehand technique.
SURGICAL PROCEDURE
The patient is first positioned prone on an OSI table with a Jackson frame (Mizuho OSI, Union City, CA). Placement of the padded bolsters can influence sagittal spinal alignment, and thus, consideration is taken to make sure that the patient is ideally positioned prior to draping. Moving the distal bolsters under the pelvis, leaving the abdomen free, will increase lumbar lordosis. The back is shaved, and a wide surgical field is sterilized to allow for visualization of the pelvis, ribs, and scapulae throughout the surgery.
Exposure and Facetectomies
A subperiosteal exposure of the posterior thoracic/lumbar spine is performed. It is essential to remain subperiosteal to minimize bleeding, a critical consideration in pediatric patients. Maintaining tension on the soft tissues with multiple retractors as dissection progresses will help minimize bleeding as well. Furthermore, during exposure, the anesthesiologist should be asked to maintain mean arterial pressures between 60 and 70 mm Hg.
Once the skin incision is made, a pointed clamp or pedicle probe is used to mark a vertebra, and intraoperative posteroanterior (PA) and lateral radiographs are obtained. These radiographs serve to confirm that the proper spinal levels are being exposed and also allow the surgeon to visualize the patient’s spinal alignment on the operating table. Next, the transverse processes of the thoracic and lumbar spine are fully exposed. The interspinous ligament is left intact on the proximal two spinous processes to minimize risk of proximal junctional kyphosis. Facet joints are thoroughly cleaned of all capsular tissue using monopolar electrocautery. The thoracic joints should be cleaned in a medial-to-lateral direction so that the electrocautery does not inadvertently enter the spinal canal.
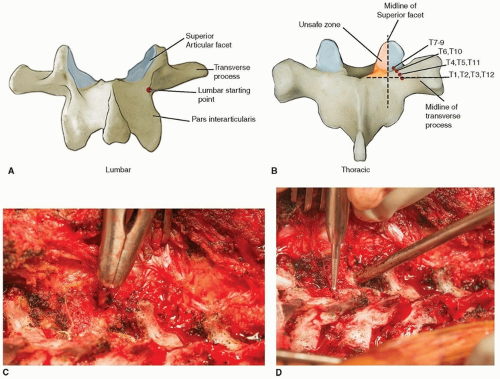
In the thoracic spine, a ½-inch straight osteotome is then used to remove the inferior 5 mm of the inferior articular facet by making two cuts (Fig. 44-1A). The superior facet cartilage is curetted away. It is essential to adequately expose the superior articular facet to visualize the critical landmarks for freehand thoracic pedicle screw placement. In the lumbar spine, a ½-inch osteotome is again used to remove the inferior articular facet by making an oblique cut in the plane of the joint (Fig. 44-1B). These facet preparations also improve the surface area for fusion.
Starting Point Identification
Steps 2 to 6 are completed for each pedicle before moving to the next. Once exposure and facetectomies are complete, the starting point for the first pedicle screw is identified. In the lumbar spine, the starting point is at the junction of the lateral border of the pars interarticularis and the inferior border of the transverse process, at the base of the superior articular process (Fig. 44-2A). To better identify this point, the superior articular facet can be removed using a rongeur; there is sometimes a mamillary process at this junction that should also be rongeured. Once the superior facet is removed, there is often a blush of blood from the cancellous pedicle tube, most often seen in type A (large cancellous channel) and type B (small cancellous channel) pedicles (2). An oval-tipped 4-mm bur is then used to puncture the corticocancellous bone overlying the pedicle.
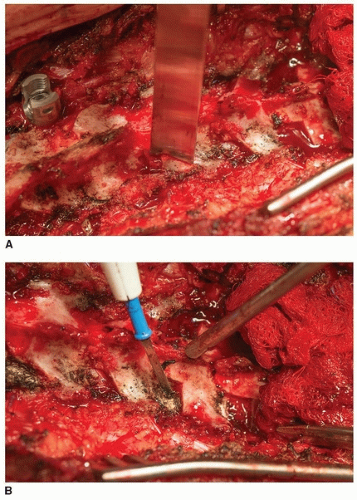
FIGURE 44-1 A. Thoracic inferior facetectomy being performed with ½-inch straight osteotome. B. Cartilage of superior facet removed using electrocautery.
In the thoracic spine, the starting points vary depending on cephalad-caudad vertebral level (4). Figure 44-2B demonstrates a mnemonic device for remembering the screw start points. Several general rules apply at all thoracic levels. First, no starting point should ever be medial to the midpoint of the superior facet in the medial-lateral direction. Second, no starting point should be distal to the midpoint of the transverse process in the superior-inferior direction. These two guidelines define a “safe zone” for starting thoracic pedicle screws. Typically, the starting points in the proximal and distal portions of the thoracic spine are slightly more lateral than in the midthoracic spine. Also, starting points at the concave apex of larger scoliotic curves tend to be slightly more lateral.
The dorsal transverse process of the thoracic vertebrae can be removed with a rongeur to obtain local autogenous bone graft. Some surgeons will also use a rongeur to remove the dorsal cortical bone at the inflection point of the transverse process as it meets the lamina in order to allow the screw head to rest more ventrally, minimizing implant prominence and facilitating pedicle cannulation. However, biomechanical studies have suggested that removing the dorsal lamina reduces screw pullout strength (5). The overall bone quality of the patient should be taken into consideration before rongeuring the dorsal lamina.
Pedicle Cannulation
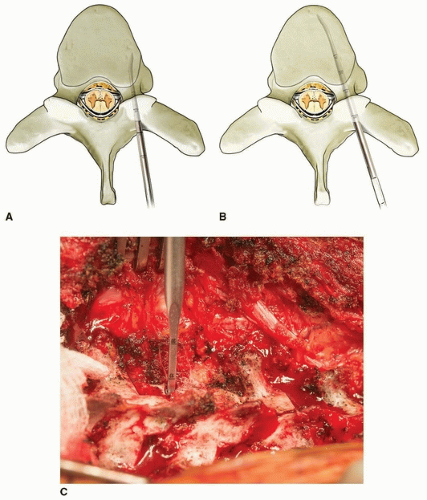
Once the starting point has been identified and burred, a pedicle probe is used to cannulate a cancellous track through the pedicle into the vertebral body. Either a straight or a slightly curved pedicle probe can be used (Fig. 44-3). For the curved probe, the point is first oriented laterally in order to avoid medial breach and possible neural tissue penetration (Fig. 44-4A). Care is taken to hold the probe with two hands at all times. The tip is placed into the burred starting hole and used to palpate the softer cancellous bone at the entry to the pedicle tube and then carefully advanced using small, controlled oscillations. In the thoracic spine, the probe is advanced to a depth of 20 to 25 mm, and in the lumbar spine, it is advanced to 30 mm. The probe is then withdrawn from the bone, the tip turned medially, and the probe reinserted to the previously achieved depth. This maneuver helps
to ensure that the tip of the probe is ventral to the spinal canal before it is medialized (Fig. 44-4B). The probe is now advanced to its final depth, and in doing so, the hand is gently moved laterally to cause the tip to progress medially toward the midline of the vertebral body. Once the desired depth is reached, the probe is oscillated a quarter turn in each direction to dilate the bottom of the track.
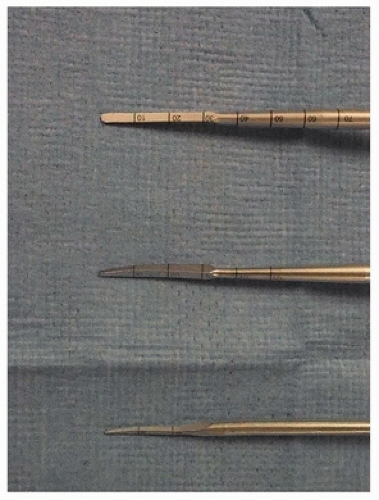
FIGURE 44-3 Pedicle probe options: 3-mm straight tip (top), 2-mm curved tip (middle), and 1-mm curved tip (bottom).
Preoperative planning and careful attention during surgery to vertebral anatomy are essential to determine the orientation and length of pedicle screws. A general rule is that the handle of the pedicle probe should align with a plane drawn between the transverse processes of the vertebra being cannulated to achieve a straight-ahead screw trajectory, which is more biomechanically favorable than is an anatomic trajectory (6). In other words, the tip of the pedicle probe should be advanced toward the contralateral transverse process, and this will guide cephalad-caudad screw orientation. Vertebral rotation must also be accounted for during freehand cannulation. The cadence of screw angulation in the axial plane should mirror the scoliosis curvature; cues can be taken from adjacent screws, adding or subtracting rotation appropriately as each subsequent screw is placed. Typically, the anterior cortex is not violated to avoid potential great vessel injury; however, on occasion, a bicortical track is cannulated. It is important to recognize the change in resistance against the probe tip when this occurs.
Any sudden advancement of the probe suggests possible breach, and the probe should not be advanced further until integrity of the track has been verified with a ball-tipped pedicle probe.
A sudden rush of venous blood from the pedicle track often indicates rupture of epidural veins by a medial breach. Bone wax is an effective method to achieve hemostasis of a bleeding pedicle track. Be cautious with use of injectable hemostatic agents, as these can enter the spinal canal via a medial breach causing spinal cord compression and loss of neuromonitoring data (7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree