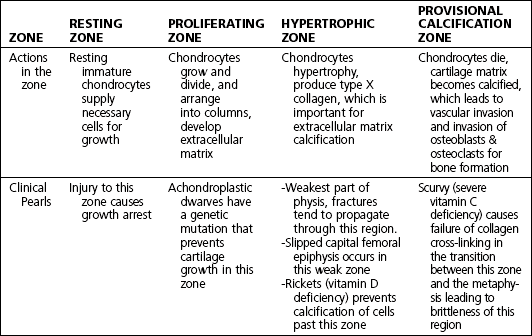
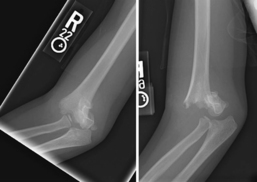
9 Pediatrics Table 9-1. (Modified from Palmer F: Keys to developmental assessment. In McMillan J, editor: Oski’s pediatrics, ed 3, Philadelphia, 2006, Lippincott Williams & Wilkins, p 789.) • Epiphysis—This region of bone is closest to a joint and lined with articular cartilage. • Ossification of the child’s epiphysis depends on age and location: Distal femoral, proximal tibial, and proximal humeral epiphysis are ossified at birth. • Ossification of the elbow epiphysis follows a sequence in pneumonic. Remember CRITOE and 1,3,5,7,9,11 for a rough age guideline for evaluating elbow radiographs: • C—capitellum: ossifies around 1 year • R—radial head: ossifies around 3 years • I—internal (medial) epicondyle: ossifies around 5 years • T—trochlea: ossifies around 7 years • O—olecranon: ossifies around 9 years • E—external (lateral) epicondyle: ossifies around 11 years • Metaphysis—the region of spongy bone that is the transition zone to the shaft of the long bone. • Endochondral ossification occurs when cartilage cells mature → hypertrophy → calcify → and are replaced by mature bone. • Endochondral ossification occurs at the physis, or growth plate, of each bone. • In long bones, the physis is located near a joint, lying in between the epiphysis and metaphysis. • Physis contains four continuous zones starting adjacent to the epiphysis to the metaphysis: resting zone (near epiphysis), proliferating zone, hypertrophic zone and provisional calcification zone (near metaphysis) (Table 9-2). • After adequate anesthesia is established, the displaced fracture is reduced with slight traction (excessive traction may be counterproductive due to tightening of thick periosteum in children), re-creation of the injury force by wrist dorsiflexion, and then volar pressure of the distal fragment. The reduction is held in place manually and confirmed with fluoroscopy. A sugar tong splint or long arm cast with a three-point mold is then applied to hold the reduction in place. • Displacement of the fracture in the splint/cast can occur, and hence serial radiographs are recommended within the first week after injury and subsequent weeks per discretion of the clinician. • Mild residual dorsal angulation (<30 degrees) in children after reduction can remodel with time. • The splint or cast should be held in place for at least 3 weeks. Radiographs should be obtained within 1 week after reduction to confirm that displacement has not occurred. Cast can be discontinued around 1 month when the fracture has healed and the patient is nontender at the injury site. • Inspect for the apex of the deformity, which serves as a clue for malrotation: An apex dorsal deformity suggests a pronation deformity of the distal fragment, whereas an apex volar deformity suggests a supination deformity of the distal fragment. • Using C-arm guidance, an appropriate start point is determined for insertion of elastic nail. A nail of 2 to 2.5 mm in diameter is usually used. In the radius, the entry point is 2 cm proximal to the distal physis along the radial border. A small incision is made and bluntly spread down to bone to prevent injury to the radial sensory nerve. The nail is inserted and passed down the shaft of the radius with the bone held reduced. In the ulna the entry point is 2 cm distal to the apophyseal plate (proximal, along the dorsoradial side). The nails are cut within 6 mm from the bone. A bivalved long arm cast is placed. • The patient’s arm is prepped and draped as proximally as possible. The fluoroscopy machine is then draped, and the patient’s arm is placed on the base of the fluoroscopy machine. • Gentle traction is applied to the arm, and varus/valgus angulation is corrected with fluoroscopic guidance. The elbow is then flexed to reduce the extended fracture. The reduction is held in place until pinned. • Two to three lateral 0.062-inch pins are placed from the lateral condyle engaging the medial diaphyseal cortex to hold the fracture in place. • The arm is splinted in a long arm posterior splint in approximately 70 degrees of elbow flexion. • Flexible intramedullary nailing (for patients < 108 lb) • The appropriate-sized nail is planned on the basis of radiographs and should be selected to be less than 40% of the narrowest portion of the femoral canal. The patient is placed supine on the fracture table, and closed reduction is obtained with gentle traction under C-arm guidance. The nails are manually contoured such that the apex of the bow is at the fracture site. A fluoroscope is used to identify the nail entry point on the lateral femur approximately 3 cm above the physis. A small stab incision is made along the lateral aspect of the distal femur, and a drill is used to open the femoral cortex. The nail is inserted to the level of the fracture. The opposite medial cortex is drilled at the same level and opened analogous to the lateral side, and a second nail is passed up to the level of the fracture. Each nail is then inserted in diverging directions past the fracture site sequentially while the fracture is held reduced. The nails are advanced until they just pass the proximal femoral physis. The nails are then cut (within 1 cm off the cortex of insertion site) and bent. Wounds are then closed. • Trochanteric entry with intramedullary nailing. • The patient is placed supine on a fracture table. C-arm images are obtained of the proximal femur before prepping to ensure adequate images are obtained. The fracture is reduced using traction on the fracture table. A small incision is made proximal to the greater trochanter, and a guidewire is used to determine the appropriate start point just lateral to the tip of the greater trochanter. The guidewire is drilled into the greater trochanter under C-arm guidance in the AP and lateral planes to verify accurate placement. An entry reamer is used to open the proximal femoral canal over the guidewire. A reaming guidewire is then placed down the intramedullary canal past the fracture site ending proximal to the physis. The appropriate length nail is then measured with the measuring guide. The femur is then reamed to the appropriate width. An intramedullary nail is then placed down the reaming guidewire with the fracture held reduced in place. The reaming guidewire is removed. Using C-arm guidance, proximal and distal nail interlocking screws are placed through stab incisions. Wounds are then irrigated and closed.
Introduction
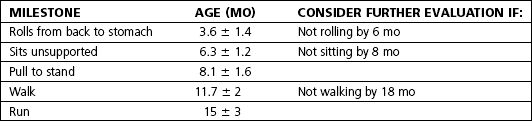
 Developmental milestones (Table 9-1)
Developmental milestones (Table 9-1)
Structure and function of bone
Skeletal growth
 Skeletal growth over the lifetime is not constant—the rate of growth is highest in the first 4 years and levels off until adolescence.
Skeletal growth over the lifetime is not constant—the rate of growth is highest in the first 4 years and levels off until adolescence.
 Growth proportion varies by anatomic region (i.e., proximal tibial physis contributes more to tibial length than distal tibial physis).
Growth proportion varies by anatomic region (i.e., proximal tibial physis contributes more to tibial length than distal tibial physis).
 Longitudinal growth of limbs occurs via endochondral ossification.
Longitudinal growth of limbs occurs via endochondral ossification.
 Fractures in children take special consideration due to growth considerations because fractures in the growth plate may cause growth disturbances and potential for limb length inequality and deformity from asymmetric growth.
Fractures in children take special consideration due to growth considerations because fractures in the growth plate may cause growth disturbances and potential for limb length inequality and deformity from asymmetric growth.
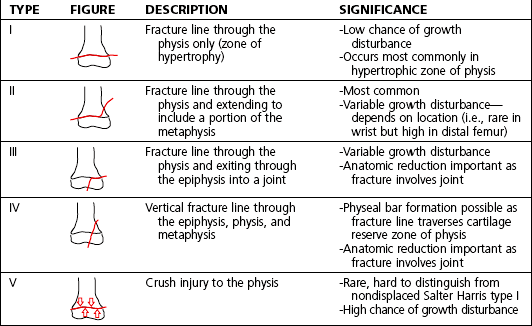
 The Salter-Harris classification is for growth plate injuries (Table 9-3).
The Salter-Harris classification is for growth plate injuries (Table 9-3).
Common pediatric injuries
History
 Background: Pediatric distal radius and ulna fractures are common injuries. Younger children generally sustain metaphyseal buckle fractures, whereas older children can sustain distal radius and ulna physeal fractures.
Background: Pediatric distal radius and ulna fractures are common injuries. Younger children generally sustain metaphyseal buckle fractures, whereas older children can sustain distal radius and ulna physeal fractures.
 Α fall onto an outstretched hand is the most common mechanism. Most fractures occur with a hyperextended wrist leading to dorsal displacement of the distal fracture fragment.
Α fall onto an outstretched hand is the most common mechanism. Most fractures occur with a hyperextended wrist leading to dorsal displacement of the distal fracture fragment.
 The patient may report pain and may have a wrist deformity or swelling.
The patient may report pain and may have a wrist deformity or swelling.
Physical examination
Initial treatment
 Low-energy trauma and nondisplaced: splint or casting in the outpatient setting
Low-energy trauma and nondisplaced: splint or casting in the outpatient setting
 Higher-energy trauma + displaced injury: closed reduction and splinting under conscious sedation in the emergency department
Higher-energy trauma + displaced injury: closed reduction and splinting under conscious sedation in the emergency department
Patient education
 Distal radius and ulna fractures are common injuries in children. The patient can expect to be immobilized in a splint or cast for approximately 3 to 4 weeks. General results of treatment are good if acceptable alignment of fracture is obtained.
Distal radius and ulna fractures are common injuries in children. The patient can expect to be immobilized in a splint or cast for approximately 3 to 4 weeks. General results of treatment are good if acceptable alignment of fracture is obtained.
 Physeal arrest is rare, although it can occur in up to 10% of physeal distal radius and ulna fractures.
Physeal arrest is rare, although it can occur in up to 10% of physeal distal radius and ulna fractures.
First treatment steps
 For nondisplaced fractures, apply a sugar tong splint without manipulation of the fracture. Provide the patient with an appropriately fitting sling.
For nondisplaced fractures, apply a sugar tong splint without manipulation of the fracture. Provide the patient with an appropriately fitting sling.
 Displaced fractures: Apply a temporary volar splint in a position of comfort. Arrange for the patient to be seen in an acute care setting that will allow for reduction and sedation.
Displaced fractures: Apply a temporary volar splint in a position of comfort. Arrange for the patient to be seen in an acute care setting that will allow for reduction and sedation.
Treatment options
 Closed manipulation and reduction of dorsally displaced distal radius and ulna fracture
Closed manipulation and reduction of dorsally displaced distal radius and ulna fracture
Pediatric forearm fractures
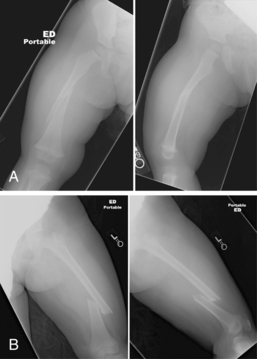
 Background: Pediatric forearm fractures include fractures of the diaphysis of the radius and/or ulna. Forearm bony anatomy is unforgiving of significant displacement or malrotation with regard to subsequent range of motion and function.
Background: Pediatric forearm fractures include fractures of the diaphysis of the radius and/or ulna. Forearm bony anatomy is unforgiving of significant displacement or malrotation with regard to subsequent range of motion and function.
 Common mechanisms include a fall onto an outstretched hand or direct blow to the forearm.
Common mechanisms include a fall onto an outstretched hand or direct blow to the forearm.
 Severe pain or neurovascular problems should prompt suspicion for compartment syndrome of the forearm.
Severe pain or neurovascular problems should prompt suspicion for compartment syndrome of the forearm.
 The patient may report forearm pain, swelling, or deformity.
The patient may report forearm pain, swelling, or deformity.
Physical examination
 Inspect for edema and rotational deformity (a key component to the injury).
Inspect for edema and rotational deformity (a key component to the injury).
 Palpate for significant tenderness at the fracture site.
Palpate for significant tenderness at the fracture site.
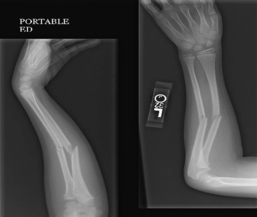
Imaging: Figure 9-2
 Anteroposterior (AP) and lateral radiographs of forearm (full length)
Anteroposterior (AP) and lateral radiographs of forearm (full length)
 Wrist and elbow radiographs to rule out associated injuries (injuries to the wrist, distal radioulnar joint, radial head dislocation)
Wrist and elbow radiographs to rule out associated injuries (injuries to the wrist, distal radioulnar joint, radial head dislocation)
 Evaluate images for the apex of the deformity and clues to malrotation including the relationship between the bicipital tuberosity and radial styloid (which should be facing opposite to each other in the normal forearm)
Evaluate images for the apex of the deformity and clues to malrotation including the relationship between the bicipital tuberosity and radial styloid (which should be facing opposite to each other in the normal forearm)
Initial treatment
 Forearm fractures are common injuries in children. These injuries must be reduced in near anatomic alignment, or limited range of motion and deformity may develop. Most preadolescents can be treated with casting. Children approaching maturity may be considered for operative open reduction and internal fixation.
Forearm fractures are common injuries in children. These injuries must be reduced in near anatomic alignment, or limited range of motion and deformity may develop. Most preadolescents can be treated with casting. Children approaching maturity may be considered for operative open reduction and internal fixation.
Treatment options
 Nonoperative management with closed manipulation under sedation/anesthesia is the mainstay of treatment.
Nonoperative management with closed manipulation under sedation/anesthesia is the mainstay of treatment.
 The deformity should be reduced, paying particular attention to the fact that forearm injuries often require reduction of a rotational deformity.
The deformity should be reduced, paying particular attention to the fact that forearm injuries often require reduction of a rotational deformity.
 A long arm cast or sugar tong splint with the elbow at 90 degrees with a flat ulna and interosseous mold can be used to hold the reduction.
A long arm cast or sugar tong splint with the elbow at 90 degrees with a flat ulna and interosseous mold can be used to hold the reduction.
 The patient should be followed up weekly for repeat radiographs, and cast immobilization should be continued for 6 weeks.
The patient should be followed up weekly for repeat radiographs, and cast immobilization should be continued for 6 weeks.
Surgical procedures
 Intramedullary nailing of forearm fracture
Intramedullary nailing of forearm fracture
 Open reduction and internal fixation of forearm fracture
Open reduction and internal fixation of forearm fracture
Radial head subluxation (nursemaid’s elbow)
 Background: Nursemaid’s elbow is radial head subluxation with an annular ligament tear and interposition of annular ligament between the radial head and capitellum.
Background: Nursemaid’s elbow is radial head subluxation with an annular ligament tear and interposition of annular ligament between the radial head and capitellum.
 This is a common injury in young children, where a longitudinal traction force is placed on the child’s extended and pronated forearm (i.e., child being helped up onto a sidewalk).
This is a common injury in young children, where a longitudinal traction force is placed on the child’s extended and pronated forearm (i.e., child being helped up onto a sidewalk).
 Children affected are usually younger than 5 years old.
Children affected are usually younger than 5 years old.
 Initially the condition is painful, but it eventually subsides, although the child will guard the extremity with activities.
Initially the condition is painful, but it eventually subsides, although the child will guard the extremity with activities.
 The patient or parents may report that the arm is not being used.
The patient or parents may report that the arm is not being used.
Physical examination
Treatment options
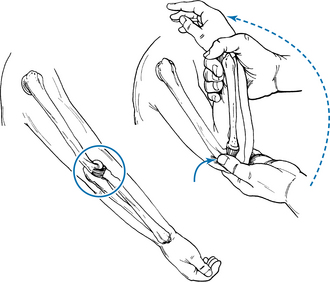
Closed reduction of radial head subluxation (figure 9-3)
 Under adequate anesthesia, child’s forearm is supinated and maximally flexed with the clinician’s thumb placed over the radial head.
Under adequate anesthesia, child’s forearm is supinated and maximally flexed with the clinician’s thumb placed over the radial head.
 A palpable click is often felt on reduction.
A palpable click is often felt on reduction.
 There is no need to immobilize after reduction if this is a first-time reduction. If this is a repeat injury, consider cast immobilization.
There is no need to immobilize after reduction if this is a first-time reduction. If this is a repeat injury, consider cast immobilization.
Pediatric supracondylar humerus fractures
Classification system
 Flexion- and extension-type injuries depending on whether the arm was flexed or extended at the time of injury; majority of injuries are of the extension type
Flexion- and extension-type injuries depending on whether the arm was flexed or extended at the time of injury; majority of injuries are of the extension type
 Gartland classification (extension-type injuries)—type I: nondisplaced, type II: angulated with an intact posterior cortex, type III: displaced with no intact cortex
Gartland classification (extension-type injuries)—type I: nondisplaced, type II: angulated with an intact posterior cortex, type III: displaced with no intact cortex
Initial treatment
 Supracondylar humerus fractures are the most common elbow injuries in young children, with a 10% to 15% neurovascular injury rate in displaced fractures. These injuries should be evaluated and treated urgently in an emergency department where a pediatric orthopaedist is available. The standard of care is to pin displaced fractures.
Supracondylar humerus fractures are the most common elbow injuries in young children, with a 10% to 15% neurovascular injury rate in displaced fractures. These injuries should be evaluated and treated urgently in an emergency department where a pediatric orthopaedist is available. The standard of care is to pin displaced fractures.
Treatment options
 Type I injuries: Immobilize initially in a posterior long arm splint and then transition to a long arm cast with the elbow at 90 degrees. Avoid hyperflexion.
Type I injuries: Immobilize initially in a posterior long arm splint and then transition to a long arm cast with the elbow at 90 degrees. Avoid hyperflexion.
 Type II injuries without significant angulation, intact medial cortex, and in which the anterior humeral line intersects the capitellum: Immobilize initially in a splint and then transition to a cast as indicated earlier.
Type II injuries without significant angulation, intact medial cortex, and in which the anterior humeral line intersects the capitellum: Immobilize initially in a splint and then transition to a cast as indicated earlier.
Surgical procedures
 Closed reduction and percutaneous pinning of displaced supracondylar humerus fracture
Closed reduction and percutaneous pinning of displaced supracondylar humerus fracture
Estimated postoperative course
 Postoperative days 7 to 10—Repeat radiographs of elbow in splint.
Postoperative days 7 to 10—Repeat radiographs of elbow in splint.
 Postoperative week 3—Repeat radiographs of elbow, splint, and pin removal if radiographs demonstrate acceptable alignment. Start range of motion at 3 weeks with activity restriction, with gradual progression based on healing.
Postoperative week 3—Repeat radiographs of elbow, splint, and pin removal if radiographs demonstrate acceptable alignment. Start range of motion at 3 weeks with activity restriction, with gradual progression based on healing.
 Postoperative month 3—Repeat radiographs and clinical evaluation of range of motion.
Postoperative month 3—Repeat radiographs and clinical evaluation of range of motion.
Pediatric femur fractures
History
 Background: Femur fractures in children can be related to both low-energy and high-energy mechanisms, including torsional-type injuries and motor vehicle accidents. Child abuse is not an uncommon mechanism of fracture in younger children (30% in children younger than 4 years old).
Background: Femur fractures in children can be related to both low-energy and high-energy mechanisms, including torsional-type injuries and motor vehicle accidents. Child abuse is not an uncommon mechanism of fracture in younger children (30% in children younger than 4 years old).
 Patient characteristics (age and patient size); fracture characteristics (spiral, transverse, comminuted); and mechanism of injury are all important in determining appropriate treatment.
Patient characteristics (age and patient size); fracture characteristics (spiral, transverse, comminuted); and mechanism of injury are all important in determining appropriate treatment.
 Patients present with pain and deformity and an impaired ability to bear weight on the affected lower extremity.
Patients present with pain and deformity and an impaired ability to bear weight on the affected lower extremity.
Initial treatment
 The appropriate treatment of pediatric femur fractures includes many variables. Most low-energy mechanism injuries can be treated in a closed fashion in young children. Internal fixation options in older children include intramedullary stabilization options. Common complications can include leg length inequality, malrotation, and angular malunion.
The appropriate treatment of pediatric femur fractures includes many variables. Most low-energy mechanism injuries can be treated in a closed fashion in young children. Internal fixation options in older children include intramedullary stabilization options. Common complications can include leg length inequality, malrotation, and angular malunion.
Treatment options
 0 to 6 months: Apply a Pavlik harness and immobilize the patient for 2 to 3 weeks. Rapid healing with exuberant callous formation is expected.
0 to 6 months: Apply a Pavlik harness and immobilize the patient for 2 to 3 weeks. Rapid healing with exuberant callous formation is expected.
 6 months to 5 years: Apply a spica cast under anesthesia (CPT Code 29325). Reduce the fracture with fluoroscopic guidance and then apply a spica cast positioning the injured extremity in approximately 45 degrees hip flexion and 45- to 60-degree knee flexion. Repeat radiographs within 2 weeks, and continue spica cast for approximately 6 weeks until healing.
6 months to 5 years: Apply a spica cast under anesthesia (CPT Code 29325). Reduce the fracture with fluoroscopic guidance and then apply a spica cast positioning the injured extremity in approximately 45 degrees hip flexion and 45- to 60-degree knee flexion. Repeat radiographs within 2 weeks, and continue spica cast for approximately 6 weeks until healing.
Surgical procedures
Estimated postoperative course
 Postoperative day 0: Ensure hemodynamic stability and monitor in the hospital. Patients generally may start partial weight bearing unless there is concern for fracture stability postoperatively.
Postoperative day 0: Ensure hemodynamic stability and monitor in the hospital. Patients generally may start partial weight bearing unless there is concern for fracture stability postoperatively.
 Postoperative days 10 to 14: Check the wound and take radiographs.
Postoperative days 10 to 14: Check the wound and take radiographs.
 Postoperative weeks 6 to 8: Repeat radiographs and clinical evaluation, and progress activities gradually if healing.
Postoperative weeks 6 to 8: Repeat radiographs and clinical evaluation, and progress activities gradually if healing.
 Postoperative months 3 to 6: Gradual progression to normal activities follows.
Postoperative months 3 to 6: Gradual progression to normal activities follows.
Pediatric tibia/fibula fractures
History
 The mechanism of injury commonly includes motor vehicle accidents, falls, and sports.
The mechanism of injury commonly includes motor vehicle accidents, falls, and sports.
 Pain is the most reliable clinical history.
Pain is the most reliable clinical history.
 In young children, inability to walk may be the clue, especially in nondisplaced toddler spiral fractures of the tibia.
In young children, inability to walk may be the clue, especially in nondisplaced toddler spiral fractures of the tibia.
 Incidence peaks at 3 to 4 years (mostly spiral fractures) and 15 to 16 years (mostly transverse fractures).
Incidence peaks at 3 to 4 years (mostly spiral fractures) and 15 to 16 years (mostly transverse fractures).
 Direct and indirect forces can contribute to tibia fractures in which direct injuries cause transverse or segmental fractures while indirect forces can cause oblique fractures.
Direct and indirect forces can contribute to tibia fractures in which direct injuries cause transverse or segmental fractures while indirect forces can cause oblique fractures.
Physical examination
Classification system
 Fractures of the proximal tibial metaphysis (common in children 3 to 6 years; most fractures are nondisplaced or greenstick with tendency to develop posttraumatic valgus)
Fractures of the proximal tibial metaphysis (common in children 3 to 6 years; most fractures are nondisplaced or greenstick with tendency to develop posttraumatic valgus)
 Fractures of the tibial and fibular shafts (complete both bone fractures are associated with higher energy mechanisms and direct blows)
Fractures of the tibial and fibular shafts (complete both bone fractures are associated with higher energy mechanisms and direct blows)
 Isolated fractures of the tibial shaft or fibular shaft (tibial shaft—torsional injuries without significant displacement or shortening due to intact fibula; fibular shaft—direct-impact injuries)
Isolated fractures of the tibial shaft or fibular shaft (tibial shaft—torsional injuries without significant displacement or shortening due to intact fibula; fibular shaft—direct-impact injuries)
 Fractures of the distal tibial metaphysis (rare injuries that generally heal without significant malalignment)
Fractures of the distal tibial metaphysis (rare injuries that generally heal without significant malalignment)
Initial treatment
 Tibia/fibula fractures represent a wide spectrum of injury severity and are common fractures in children. In general most low-energy mechanism injuries are expected to heal well with closed treatment. Higher-energy mechanism injuries can be associated with open fractures and a higher rate of subsequent disability.
Tibia/fibula fractures represent a wide spectrum of injury severity and are common fractures in children. In general most low-energy mechanism injuries are expected to heal well with closed treatment. Higher-energy mechanism injuries can be associated with open fractures and a higher rate of subsequent disability.
Treatment options
Fractures of the proximal tibial metaphysis
 Closed manipulation to correct valgus angulation under anesthesia and application of a long leg cast with knee extended is the treatment of choice.
Closed manipulation to correct valgus angulation under anesthesia and application of a long leg cast with knee extended is the treatment of choice.
 Immobilize for 4 to 6 weeks in a cast.
Immobilize for 4 to 6 weeks in a cast.
 Monitor weekly radiographs for first 3 weeks and then spread out future radiographs.
Monitor weekly radiographs for first 3 weeks and then spread out future radiographs.
 Remove cast when fracture is healed. Progress knee range of motion and activities as tolerated.
Remove cast when fracture is healed. Progress knee range of motion and activities as tolerated.
 Valgus deformity of less than 15 degrees generally remodels and improves with time.
Valgus deformity of less than 15 degrees generally remodels and improves with time.
Fractures of the tibial and fibular shafts, isolated fractures of the tibial shaft, fractures of the distal tibial metaphysis
 Closed fractures should be treated with immobilization in a cast.
Closed fractures should be treated with immobilization in a cast.
 Obtain closed reduction and long leg casting with approximately 30 degrees of knee flexion.
Obtain closed reduction and long leg casting with approximately 30 degrees of knee flexion.
 Acceptable alignment is 5 degrees varus/valgus, 5 degrees flexion/extension, less than 1 cm shortening, and less than 50% translation.
Acceptable alignment is 5 degrees varus/valgus, 5 degrees flexion/extension, less than 1 cm shortening, and less than 50% translation.
 Immobilize for 4 to 6 weeks in long leg cast, and instruct patient not to bear weight.
Immobilize for 4 to 6 weeks in long leg cast, and instruct patient not to bear weight.
 Monitor weekly radiographs for first 3 weeks, and then spread out future radiographs.
Monitor weekly radiographs for first 3 weeks, and then spread out future radiographs.
 Transition to short leg cast or patellar tendon-bearing cast with healing fracture for 2 more weeks.
Transition to short leg cast or patellar tendon-bearing cast with healing fracture for 2 more weeks.
Operative management
Informed consent and counseling
 Tibia fractures can develop rotational or angular malunion, as well as length discrepancy to the contralateral leg. Proximal metaphyseal fractures tend to angulate toward valgus, whereas isolated tibial fractures tend to angulate in varus after initial casting. Repeat manipulations may be necessary to maintain some reductions, and if these fail operative management is indicated.
Tibia fractures can develop rotational or angular malunion, as well as length discrepancy to the contralateral leg. Proximal metaphyseal fractures tend to angulate toward valgus, whereas isolated tibial fractures tend to angulate in varus after initial casting. Repeat manipulations may be necessary to maintain some reductions, and if these fail operative management is indicated.
Pediatrics