Fig. 10.1
a A 3-year-old with a crushing injury to the left thumb from getting her thumb stuck in a bicycle gearshift. b Transverse laceration to the nail bed noted after debridement of the edges. c Nail bed repaired with 6.0 chromic sutures. d Nail plate replaced
There is a lack of quality evidence from randomized controlled trials to guide key treatment decisions for the management of fingertip injuries in children regarding whether or not prophylactic antibiotics should be given following surgical treatment or the superiority of paraffin dressing over a silicone net dressing.
Regarding the question of prophylactic antibiotic use after surgical repair either in the emergency room (ER) or operation room (OR), no conclusive evidence has been elicited regarding the benefits of prophylactic antibiotic use after surgery [17]. In a large prospective controlled study involving 135 patients with injuries ranging from skin and nail bed lacerations to loss of skin pulp and partial and complete amputations, 69 had no antibiotics and 66 were given cephalexin. Only two infections were reported. One was in the antibiotic group and the other was in the group that received no antibiotics. The authors concluded that no antibiotics are needed to treat acute fingertip injuries as long as the wounds were thoroughly cleaned and debrided [18]. In another study, infections that did result following surgery were related to more severe injuries (partial amputation), requiring a larger than average number of sutures [17].
Comparison of silicone net dressings with paraffin gauze dressings after surgical or conservative management of fingertip injuries reveals a lack of quality evidence of support of one practice over another, with regard to healing time, wound infection, or skin necrosis [17, 19]. Low-quality evidence does not allow firm conclusions to be drawn regarding the superiority of a specific dressing on healing time or complications. However, silicone dressings may be less likely to adhere to wounds, thereby making their eventual removal less distressing to the child [19]. No evidence exists regarding longer-term outcomes on fingertip function, nail growth, or nail deformity.
Fingertip Amputations
In the past, fingertip amputations in children were treated by composite grafting, a euphemism for nonvascular reattachment of the tip [20], local flap coverage, or conservative dressing change. In a study by Moiemen, the outcome of composite graft replacement of 50 amputated digital tips in 50 children over a period of 3 years and 6 months was investigated [21]. Eleven of 18 tips (61 %) which were replaced within 5 h survived completely while none of 32 digital tips replaced after 5 h survived completely. This difference was highly significant. For those children who fail this technique and have to rely on secondary reconstruction often end up with a shortened, deformed finger . This may result in negative psychological effects for the child as they enter school age. Thus, replantation of amputated digits in the pediatric hand has gained popularity over the past 20 years. However, studies have shown that it has lower rates of success than in the adult population at 69 % [22] as compared to adults at 90 % [23]. This is supposedly due to the increased frequency of crush and avulsion injuries in children and the smaller size of the vessels [24]. Children tend to heal quickly and adapt more effectively to traumatic events. Many of the injuries contraindicated for replantation in adults can be surgically repaired in children. Amputations distal to the lunula of the fingernail may be treated with primary suturing and microsurgical techniques. There are very few contraindications for replantation in the pediatric population due to improved tissue resiliency [24].
However, replantation at a level distal to the distal-interphalangeal joint is technically difficult. Skills proficient with microsurgical techniques are required, as is experience with pediatric patients. The diameter of the terminal arteries might be less than 0.5 mm in children. Veins are even smaller at 0.2 mm [25]. Anastomosis of such small vessels is technically demanding, and requires high-power microscopic magnification. In their series, Shi et al. used 11-0 or 12-0 suture under 25–30x magnification. They used three to four stitches for vascular anastomoses, suggesting that additional sutures were unnecessary and may add damage to the vessel intima, thus increase risk of thrombosis [26].
Despite the fact that good results have been obtained in fingertip replantations of children, it is mandatory to point out that the candidacy for replantation should be carefully assessed before surgery. Yamano classified amputations into four types according to the extent and severity of the injury: clean-cut, blunt-cut, avulsion, or crush [27]. Although replantation of clean-cut amputations has a higher survival rate, crush-amputated replantation is more liable to fail [28]. This may be due to the significant intimal and surrounding soft tissue damage incurred with crush mechanisms of injury. Shi et al. suggest that amputations involving a crush mechanism of injury should be contraindicated for replantation [26].
Apart from the difficulty of repairing small arteries, reestablishing venous outflow poses its own set of challenges. Dorsal veins have been demonstrated difficult to retrieve in some series [29]. With such cases, an artery- only technique of repair, where only one artery is repaired and venous drainage is provided by bloodletting technique, has been used for reperfusion. The bloodletting technique involves excision of a small square of skin from the distal fingertip or a transverse or oblique fish-mouth incision at the pulp tip limited to the dermis layer. The fingertip is evaluated frequently on the basis of its color. If the replant is blue or cyanotic, bloodletting is enhanced. If the tip is pink in color, it is reduced. It is altogether discontinued when the replanted tip takes on a constant pink color that indicates establishment of balanced arterial inflow and venous outflow. Generally, this takes 4–6 days to reestablish venous circulation [26]. Many of these children will require blood transfusions during the early stages of bloodletting, especially if anticoagulants such as heparin, dextran, or aspirin are used [30].
Sensory recovery is another parameter to consider efficacy of digital replantation. Sensory return has been reported in fingertip replantations without nerve repair [31]. Good restoration of nerve function as measured by sharp/dull perception, static two-point discrimination, “skin wrinkle” test, and Semms–Weinstein monofilament testing is related to spontaneous neurotization in children [32]. Factors such as younger age, more distal amputations, and generally good health and tissue resiliency of children contribute to overall good final outcomes [26].
In general, there are factors that have been shown to predict success or failure in replantation in children. Replants that showed poor reflow did not have a successful venous repair or involved an avulsion injury as opposed to a clean-cut were more likely to fail despite local or systemic anticoagulation therapy. One must also take into account that bone growth after replantation is critical to long-term success in restoring function. The physis of the distal phalanx retains an ability to function up to 80 % normal but outcomes are unpredictable [33]. In addition, rehabilitation improved range of motion, decreased stiffness, and indirectly improved functional sensibility [31].
Pediatric Shaft Fractures of the Distal Phalanx (Seymour Fracture)
Suspicion of fracture involving the distal phalanx should be considered with the mechanism of injury, typically a crush mechanism. Seymour fracture involves disruption of the growth plate of the distal phalanx. Detection of this injury can be difficult, as the initial radiographs may be unremarkable. Follow-up films may demonstrate displacement of the distal portion of the phalanx in a flexed position.
A hyperflexion deformity to the fingertip in a child is frequently mistaken for a mallet finger . In reality, the extensor tendon is still attached to the proximal dorsal metaphysis of the distal phalanx, as the flexor digitorum profundus tendon insertion is more distal [34]. Thus, with disruption of the cartilaginous physeal plate, the proximal fragment will be forced into extension and the distal fragment will flex causing an “open-book” flexion fracture of the physis at the proximal end of the distal phalanx. In preadolescents, the fracture is either a Salter–Harris type 1 or 2 (Fig. 10.2), and in adolescents it is generally a type-3 pattern. The diagnosis can be tricky in very small children, under 3 years old, whose epiphysis may not be calcified.

Fig. 10.2
Lateral radiograph of Seymour fracture. Note preservation of articular alignment with displacement of physis. FDP insertion provides deforming force. FDP flexor digitorum profundus
One must carefully examine the nail bed for a transverse laceration and that can only be done by removing the nail plate. In many cases, the nail plate is already avulsed out of the eponychial fold. The nail bed is usually interposed into the fractured physis. This interposition has several ramifications. Firstly, this injury needs to be treated as an open fracture that should be thoroughly cleaned or an infection will result that will destroy the growth plate. In addition, leaving the tissue interposed will result in malunion resulting in a pseudo-mallet deformity (Fig. 10.3).
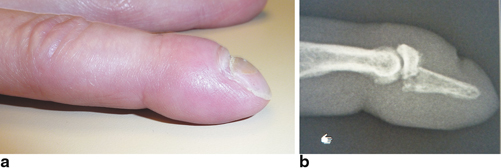
Fig. 10.3
a Pseudo-mallet deformity from an old untreated Seymour fracture. b. Lateral X-ray of a pseudo mallet deformity due to a malunion of the proximal metaphysic
Thus, if left untreated, growth arrest at the distal phalanx is virtually inevitable and in young children it will result in a shortened distal phalanx with stiffness in the distal-interphalangeal joint (DIPJ) as well as a permanent nail deformity or even absence of the nail plate. These injuries, if closed, can be treated with simple reduction with or without K-wire fixation. However, most of these injuries are open with the physis herniated through the nail bed (Fig. 10.4a, b, c).

Fig. 10.4
a Seymour fracture with herniation of physis. Nail plate is removed to identify pathology. b Herniation of physis noted after removal of nail plate. c Seymour fracture deformity accentuation to emphasize physeal instability
Rogers and Labow described a 6-year-old child who was 3 years after a crush injury to the fingertip which was treated expectantly [35]. At 3 years, there was gross nail plate deformity over a nonunion at the distal phalanx. The idea that a small child’s fingertips “do fine” regardless of what is done has no basis in fact. Treatment must include removal of the nail plate, careful debridement of the physis, removal of the soft tissue, irrigation, fracture reduction, repair of the nail bed, and replacement of the cleaned nail plate under the eponychial fold to act as a stent to help hold the reduction. A longitudinal K-wire is placed across the fracture, if needed. Good results can be obtained even with delayed presentation up to 1 month. Beyond that time, healing may be too definitive, and resultant deformity may adversely affect function and appearance [34] (Fig. 10.5).
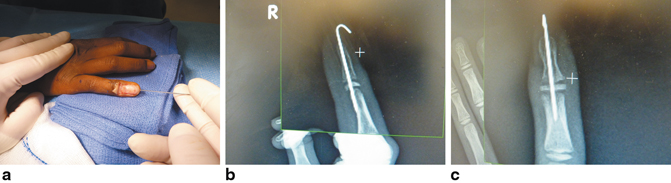
Fig. 10.5
a Appearance after open reduction of physis with retrograde percutaneous pin application. b Lateral radiograph after open reduction percutaneous pinning. c Anteroposterior radiograph with reduced physis after open reduction percutaneous pinning
Pediatric Middle Phalanx Fractures
Fractures of the distal portion of the middle phalanx may also be involved with the crush mechanism of injury. These can present themselves initially as rather benign injuries, as often neither nail plate, nail bed nor physeal plate are involved (Fig. 10.6). However, close inspection of the radiographs of the distal portion of the middle phalanx and its articular condyle may reveal joint disruption and inherent instability or malalignment of the joint (Fig. 10.7). These fractures, if not managed in a timely fashion, may become difficult to reduce via closed reduction methods due to the healing capacity of a healthy child. In addition, due to external forces surrounding the joint in the way of tendinous insertions, it may be difficult to maintain any reduction of these injuries without internal fixation. Open reduction of the small fragments with judicious use of internal fixation may provide sufficient positioning of the fracture fragments and stabilization to allow for satisfactory healing and minimization of functional limitations due to malunion or instability .
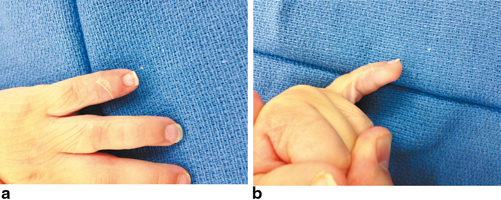
Fig. 10.6
a Appearance of crush injury to small finger in a 3-year-old. b Appearance of crush injury to small finger in a 3-year-old

Fig. 10.7
a AP radiographs show subtle disruption of distal portion of middle phalanx. b Lateral radiograph with more profound deformity of distal middle phalanx condyle with clearly identified malalignment of the distal interphalangeal joint. AP anteroposterior
Classification
Fingertip injuries involve three basic structures: soft tissue, nail and its supporting tissues, and the distal phalanx. Any one of these or a combination of all these structures may be involved in injury to the fingertip in a child. However, due to the varied involvement of injured tissues, wordy descriptions can prevent succinct communication and description of the injury at hand. Classification systems should concisely convey the description of the injury details, they should help determine the injury severity, and provide for treatment recommendations on the basis of injury severity.
Evans and Bernadis (2000) presented a fingertip injury classification system that described the injury on the basis of “pulp, nail, bone” (PNB), as often is the case, all three components may be involved. Each of these structures was given a numeric value depending on its level of injury [36]. These subdivisions of injury level for the given structure started at 0, indicating no damage, to the highest number (7 for pulp; 8 for nail and bone), indicating total loss of that structure (Table 10.1). For any given fingertip injury, the three tissues are graded and a three-digit number is elicited that should accurately define the injury. Validity and applicability of this system remain to be determined. However, it has promise for a number of uses including injury description, standardization of treatment parameters, and may provide a basis for comparative studies of the result of treatment with readily available data derived from the numeric nature of the system.
Table 10.1
The “pulp, nail, bone” (PNB) classification of fingertip injuries
Pulp level | |
0 | Intact |
1 | Laceration |
2 | Crush |
3 | Distal traverse |
4 | Palmar oblique |
5 | Dorsal oblique |
6 | Lateral |
7 | Complete |
Nail level | |
0 | Intact |
1 | Sterile matrix laceration |
2 | Germinal and sterile matrix laceration |
3 | Crush |
4 | Proximal nail bed avulsion |
5 | Distal third |
6 | Distal two thirds |
7 | Lateral |
8 | Complete |
Bone level | |
0 | Intact |
1 | Tuft loss |
2 | Comminuted nonarticular fracture
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|





