Chapter 16 Patient-Specific Unicompartmental and Bicompartmental Resurfacing Arthroplasty
Introduction
Total knee arthroplasty has become one of the most common surgical procedures due to its clinical success and longevity. In the United States, more than 500,000 primary total knee replacements were performed in 2006.1 This volume is expected to grow to 3.48 million by 2030.2
Imaging technology
The process for building patient-specific implants and instruments begins with a preoperative computed tomographic (CT) scan performed on commonly available machines (Figure 16–1). The scan, which includes partial views of the hip and ankle, is converted into a virtual three-dimensional model of the patient’s knee. The partial views of the hip and ankle are used to align the implant and cut guides in relation to the patient’s anatomic and mechanical axes.
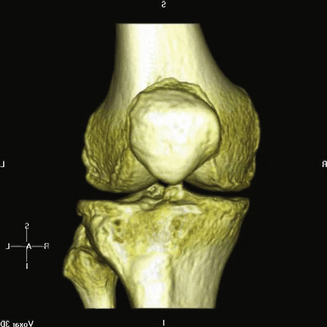
Figure 16–1 Three-dimensional image of the knee taken by a multidetector computed tomographic scanner
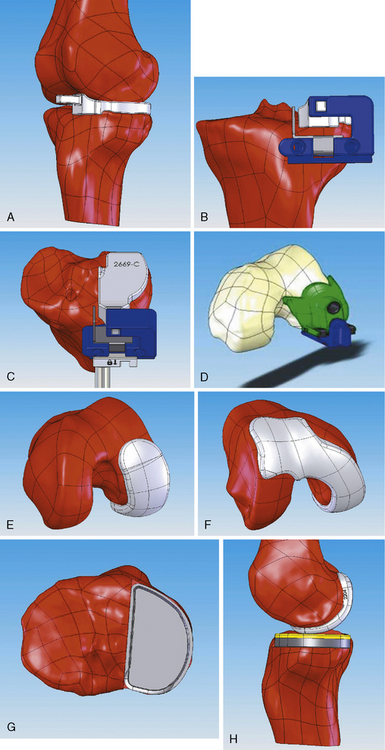
One of the more unusual aspects of surgery using patient-specific implants is the instrumentation set, which consists of a small number of guides that are generated for one-time use with each implant. The cut guides are matched to the patient’s anatomy using the same process as the implants, thus eliminating intraoperative sizing and allowing for tactile feedback to help establish positioning. The instruments are prenavigated using the scan data so that all cuts and drill holes are set with respect to the axis (Figure 16–2).