4 Pathological principles
Physical considerations
Pathological factors to consider are both local and general.
Local factors
Inflammation (Fig. 4.1)
Inflammation may have an acute and a chronic stage. Acute inflammation is the response of the tissues to injury. It is a common process which occurs following mechanical or chemical trauma, infection, extremes of temperature, ischaemia, bacterial invasion and faulty immune reactions (Box 4.1). It is a necessary and positive event, being an important defensive mechanism essential for adequate healing to occur. It can, however, be induced or maintained inappropriately, in which case it may cause severe tissue damage, pain, deformity and loss of function in the affected parts.
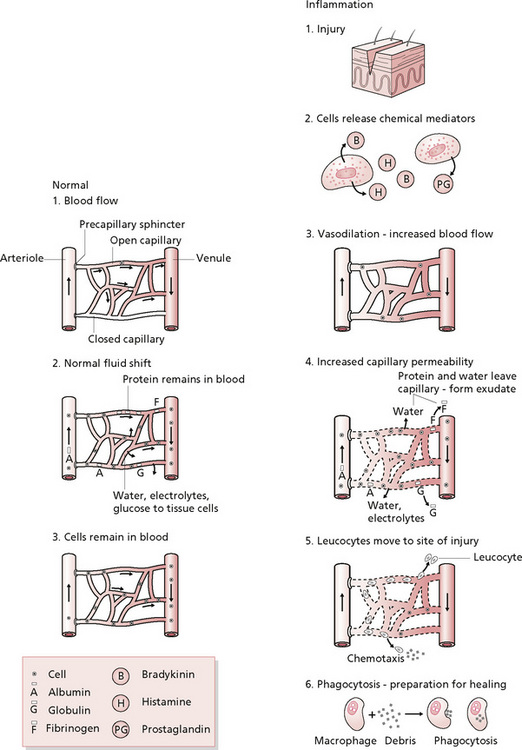
Figure 4.1 • Inflammation: a comparison of normal capillary exchange and inflammatory response.
Reprinted from Pathophysiology for the Health-related Professions, Gould (1997) with permission from Elsevier.
Box 4.1 Stages of acute inflammation
• Transient phase: mild injury, caused by histamine, lasts approximately 15 minutes.
• Delayed persistent phase: delayed response in which swelling may take up to 24 hours to reach a maximum because of endothelial cell damage.
• Immediate persistent response: may last for several days until damaged endothelial cells are replaced.
Note that massage is contraindicated over an area of acute inflammation.
The subacute phase lasts from 2 to 4 weeks after injury and is the period when resolution becomes complete and symptoms gradually subside (Kloth et al 1990).
Chronic inflammation
The symptoms of inflammation (see Box 4.2) are known as the four cardinal signs. Redness is caused by the capillary vasodilatation and increased blood flow; swelling is caused by the inflammatory exudate in the tissues, enhanced by a reduction in lymphatic drainage in the area due to fibrinogen clots; heat is due to increased blood flow; and pain results from the former events, particularly the distension of tissues, pressure exerted by the oedema in limited tissue space and chemical irritation from inflammatory mediators.
Healing (Fig. 4.2)
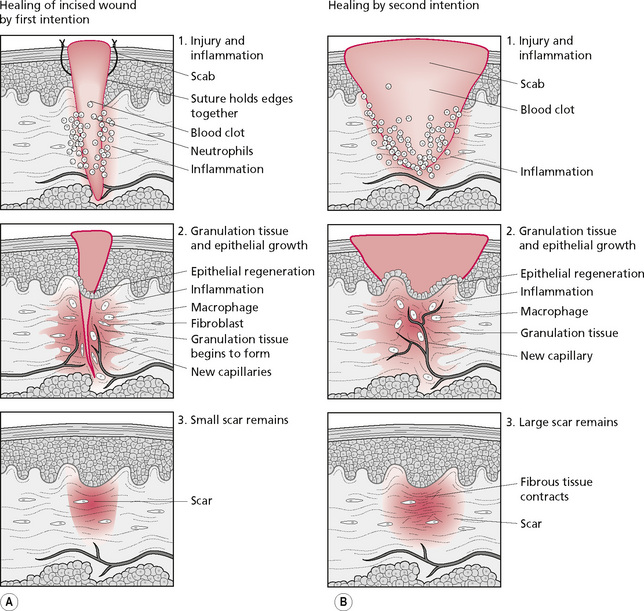
Figure 4.2 • The healing process.
Reprinted from Pathophysiology for the Health-related Professions, Gould (1997) with permission from Elsevier.
There are two types of healing, the distinction being whether there is tissue loss. If the wound is a neat incision (a cut with a knife, for example) there is no tissue loss, whereas in the case of a skin graze, or a blow leaving crushed muscle fibres which die, tissue loss leaves a gap. Wounds without tissue loss heal by ‘first intention’ and those with tissue loss heal with ‘second intention’ (Fig. 4.2).
Mechanical stress is important at this stage for the remodelling of collagen (replacement of type III with type I collagen) and also for alignment along the lines of stress. This alignment is due to the piezo-electrical effect whereby electrical streaming potentials result from mechanical stress and dictate the remodelling process. This stress is usually produced internally by normal functional activity, for example when muscle contraction exerts a pull on a tendon or when joint movement applies forces to ligaments. The effect may be enhanced with artificial stress, applied externally by manipulation of the tissues. Massage, therefore, will promote remodelling and thereby increase the tensile strength of the tissues. This effect is particularly important where immobility, either local or general, has been enforced. The lack of movement will have resulted in reduced stress being exerted on the tissues which has a weakening effect, even in normal tissues, as demonstrated by research (Akeson et al 1973).
Friction massage has been found not to influence the vascularity, pliability or height of hypertrophic scarring (as assessed by the Vancouver Burn Scar Assessment Scale) when it was given to 30 children for 10 minutes daily over a 3-month period (Patino et al 1999). The choice of frictions as a massage technique in this study can be questioned. It placed a high level of dynamic mechanical stimulation in tissues in which, in the case of hypertrophic scarring, the balance between the lysis and synthesis of collagen has been lost. It is perhaps unsurprising that this study yielded negative results when there is evidence that continuous pressure is effective in reducing the effects of hypertrophic scarring.
• Enhance natural healing processes;
• Increase surrounding circulation, thereby increasing local blood flow;
• Increase venous and lymphatic drainage from the area, enhancing the removal of waste products and proteins;
• Promote remodelling of collagen;
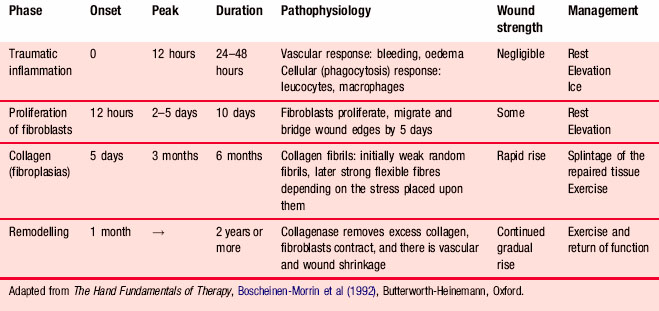
At all times, the stage of healing must be considered—this guides the effectiveness and safety of the techniques. The timetable of healing is now well established and the summary in Table 4.1 provides a good basis for clinical decision-making and treatment planning.
At this chronic stage, massage should be vigorous, focusing on prolonged stretching manipulations.
Fluid balance in the body
To maintain a perfect balance of fluid between the circulatory system and the tissues, the circulation must be operating normally, in both the structure of the carrying vessels and the constituents of the blood itself. The heart pumps arterial blood into the periphery of the body, through the arterial system, so the veins must operate an efficient system of return. They must be sufficiently pliable to be squeezed by contracting muscles, to pump the blood from the superficial veins into the deep veins and then upwards along the venous system, against gravity. Valves stop the back-flow of blood when the muscles relax, thus contributing to the pumping effect. A strong dynamic muscle pump will make this system extremely efficient, and weakened muscles or immobility will decrease its effectiveness. The volume being returned to the heart must match the volume being pumped by the heart, and a system of fluid balance maintenance must operate successfully at the arteriovenous capillary loop, through pressure equalisation between the tissues and vessels (see Chapter 2). Adequate tissue pressure around the muscles created by the fascial layers will give the muscles a firm covering to contract against, ensuring that good squeezing of the veins occurs.
Causes of oedema
• Inflammation, as in an acute injury or an allergic response in the skin, causes increased permeability of the capillaries, and excess fluid will leave the circulation for the tissues.
• If pressure is placed on any part of the circulatory system, as in pregnancy, varicosity or thrombosis in the veins, the increased hydrostatic pressure within the vessels will be in excess of that in the tissues, resulting in oedema.
• Pressure can be increased in the circulatory system by heart malfunction. Cor pulmonale results from pulmonary conditions in which the pressure in the pulmonary artery is increased, exerting a back pressure on the right ventricle, resulting in hypertrophy and reduced output by the insufficient heart musculature. The back pressure causes congestion in the veins of the periphery, raising the hydrostatic pressure in the venous blood with inevitable oedema.
• Insufficiency of the lymphatic system, for example congenital absence or damage to the lymph glands by radiotherapy or surgery, means that proteinous fluid accumulates in the tissues.
• Other medical conditions can create oedema in the tissues. Heart failure, which lowers cardiac output, leads to a lowered capillary pressure, which affects perfusion in the kidneys. Sodium and water are retained by the body, some of the fluid being pushed into the tissues. Primary renal disease invariably leads to a reduced filtration rate with excess retention of salts and fluid (Woolf 1988).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree