Chapter 15 Patellofemoral Arthroplasty
Introduction
Isolated patellofemoral arthritis occurs in approximately 5% to 10% of patients undergoing prosthetic replacement. A radiographic study of 206 patients attending an outpatient orthopedic clinic with arthritis of the knee revealed that 9.2% of the patients had isolated patellofemoral arthritis.1
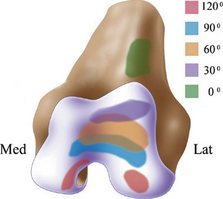
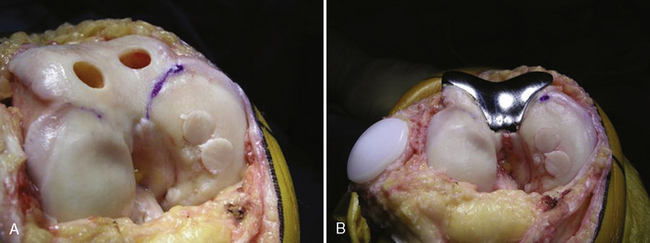
Ideally, the goals of a patellofemoral prosthesis include alleviation of patellofemoral symptoms and improved functionality. The prosthetic design should be conservative and joint preserving. The trochlea implant should remove minimal bone stock and allow mismatch of sizes between the trochlea and patella with minimal incongruity. A trochlea design should allow for deep flexion prior to the patella prosthesis disengaging the trochlea prosthesis so that the native tibiofemoral cartilage is not abraded by the polyethylene patella (Figure 15–1).2 Implant characteristics should include a design based on existing total knee arthroplasty models such that implant failure or progression of tibiofemoral arthritis would allow easy conversion to total knee arthroplasty while retaining the existing patella prosthesis.
Argenson et al3 proposed a useful clinical categorization of osteoarthritis of the patellofemoral joint: (1) secondary to dysplasia, (2) osteoarthritis involving primarily the patellofemoral joint, and (3) posttraumatic osteoarthritis in the patellofemoral joint secondary to patellar fracture. The group with dysplasia was the youngest group of patients in the series. They generally had a chronic history of patellar maltracking. Realignment surgery was frequent prior to prosthetic reconstruction. The long-term results of the first group, the dysplastic group, was the best in the series. This is not unexpected because these patients generally had normal tibiofemoral alignment and did not have a propensity to osteoarthritis because their arthritic condition was secondary to dysplasia of the trochlea and with abnormal shear forces and secondary osteoarthritis. The second group, the osteoarthritic group, was the most unpredictable. These patients generally did well in the first 5 years; however, progression of tibiofemoral joint arthritis was the source of joint failure. The prosthesis itself generally did not fail. The third group, with posttraumatic patellar fracture, also did well as long as they did not have patella infera. Patella infera with a polyethylene resurfacing patella results in premature abrasive changes to the articular surface of the tibiofemoral joint and failure of the joint.
Indications
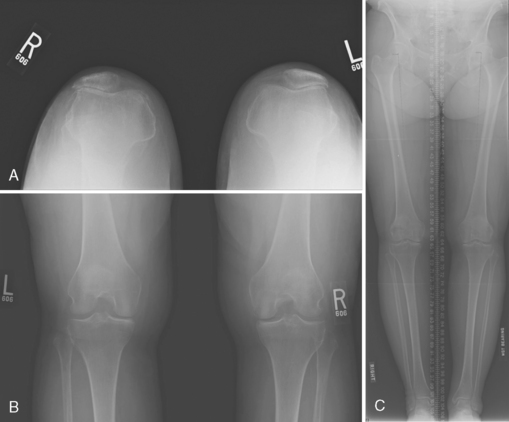
Indications for patellofemoral arthroplasty include end-stage patellofemoral osteoarthritis secondary to patellofemoral dysplasia, osteoarthritis, and patellar fracture as noted by Argenson et al.3 Contraindications to the procedure include patella infera and inflammatory arthritis. Relative contraindications include age approaching that for total knee arthroplasty (i.e., 60s), crystal arthropathy, and tibiofemoral malalignment (Figure 15–2).
Patellofemoral replacement is used as a transition operation for patients prior to total knee arthroplasty. The younger the patient with end-stage patellofemoral arthritis, the more likely a patellofemoral prosthesis, including osteochondral graft transfer to early damage in the tibiofemoral joint (Figure 15–3) or excepting mild malalignment of the tibiofemoral joint (Figure 15–4), will be used rather than total knee arthroplasty with subsequent early failure of part of the joint. Conversion to total knee arthroplasty in a young patient has not always been necessary if isolated unicompartmental replacement could be performed in addition to leaving the existing patellofemoral replacement (Figure 15–5). In my experience, patients are in their 40s and early 50s when patellofemoral arthroplasty is performed. When patients present with patellofemoral dysplasia, they frequently have a longstanding history of recurrent instability and prior surgeries, frequently including tibial tubercle realignment osteotomy. Some patients undergo tibial tubercle osteotomy at the time of patellofemoral replacement in order to maintain stability of the implant (Figure 15–6).