Fig. 8.1
anterior and medial views of the knee joint from volume rendered computed tomography depicting the normal anatomy and relations
8.1 Proximal Procedures
Patellar instability is a term that describes a multitude of causes that lead to chronic lateral patellar subluxation or recurrent episodes of dislocation. The clinical presentation is usually residual after an acute dislocation in patients with altered patello-femoral and extensor mechanism morphology.
The clinical exam findings are the most important when deciding for surgical treatment of patellar instability. The positive apprehension test is a very suggestive subjective measure of lateral instability. It is performed with the patient supine and the knee close to full extension. The examiner gently pushes lateral on the patella while the patient’s intension is to apprehend and terminate the action. The lateral glide should have no firm endpoint and the translation should be greater than two quadrants (roughly patellar quarters) or 10 mm. The knee is put through flexion and the centration of the patella in the trochlea is observed. Permanent lateral dislocation will require more than MPFL reconstruction.
8.1.1 Lateral Release
Is commonly performed during arthroscopic procedures. However, the indications have reduced considerable and there is very little evidence to support isolated use. The main indication to performing lateral release, isolated or in association with proximal or distal procedures is excessive patellar tilt and lateral facet hyperpressure due to tightness of the lateral retinaculum or a dysplastic quadriceps. In other circumstances, lateral retinacular release may aggravate patellar instability in early flexion [2, 12].
The patellar tilt is the angle formed by the transverse axis of the patella to a line tangential to the posterior femoral condyles. 3D CT images visualize the abnormalities but are not able to quantify them (Fig. 8.2):
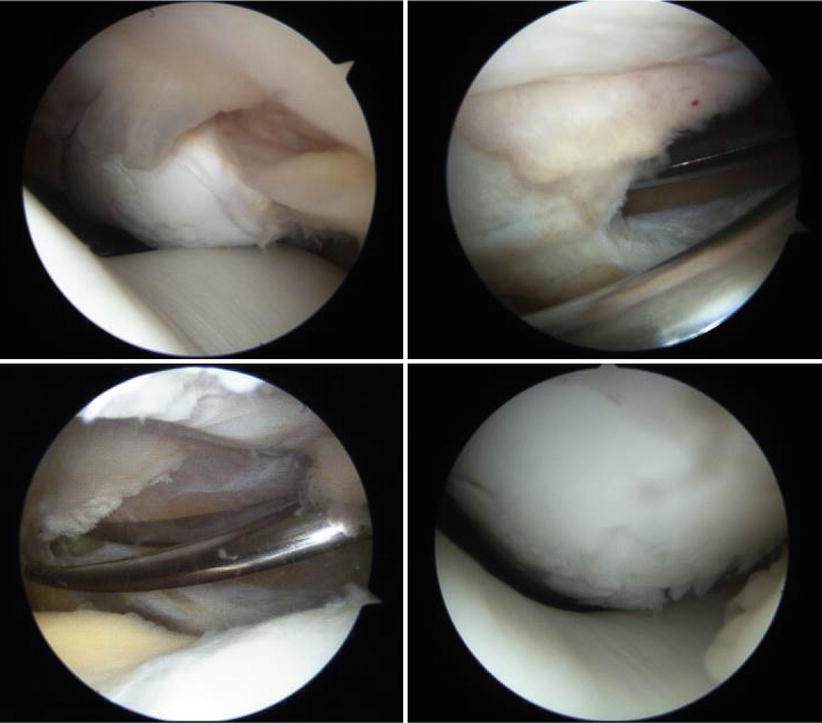
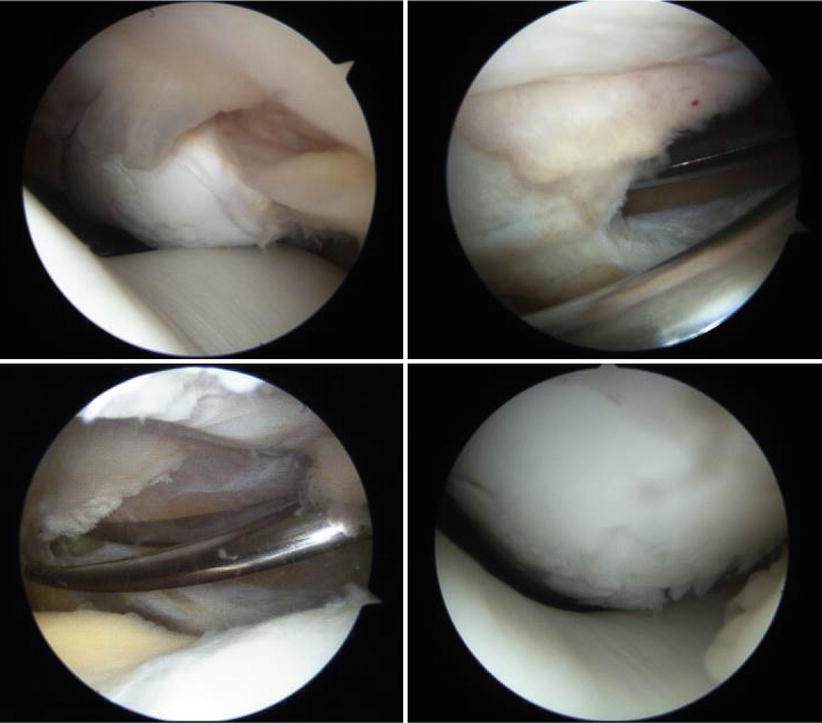
Fig. 8.2
Arthroscopic view through the anteromedial portal with the knee in extension; the patella is not centered in the trochlea. Lateral retinaculum release is performed with the scissors and this improves the tracking. The patellar cartilage is fragmented
8.1.2 Medial Reefing
Medial plication can be done mini open or arthroscopic. Three to five sutures (PDS No.1) are started from the distal third of the patella. These are passed over the ruptured medial structures if visible, such as in acute cases. If not, a 2 cm bridging from the medial border of the patella can be selected. Simple or vertical mattress type sutures can be performed, with the later having a true plication effect. Stability during range of motion is verified and additional sutures may be added or cut if inappropriate patellar tracking is observed. For the arthroscopic technique, the sutures are passed similar to ‘outside in’ meniscal sutures: two needles are used to pass a No.1 PDS and looped No.2/0 PDS sutures respectively. The No.1 is then passed through the loop with the aid of the probe or a grasp. The procedure is repeated for each suture and all are tightened at the end, with the knee in 60° of flexion.
8.2 MPFL Reconstruction
The acute lateral patella dislocation almost always tears the aponeurotic medial constraints and the medial patello-femoral ligament (MPFL). Nonsurgical approach is the recommended treatment for the initial episode, unless osteochondral fractures are loose in the joint. After reduction, the knee is immobilized in 20° of flexion. Gradual range of motion is started after two weeks with the orthosis on. Vastus medialis oblique (VMO) strengthening exercises are started after 6 weeks. This leads to 15–44 % recurrence rates, compared to 10–20 % after reconstruction of the MPFL, even in pediatric patients [19, 17].
The MPFL is the main passive medial restraint [1] and the VMO the main dynamic stabilizer, with obliquely oriented fibers. The MPFL is most taut with the quadriceps contracted and the knee in extension. During early flexion (20°), it resists lateral tensions and centers the patella in the trochlear groove [2]. The lateral trochlear facet becomes the main stabilizer in higher flexion (over 30°) [3]. It also resists lateral patellar tilt and rotation up to 90° of flexion.
Numerous variations for MPFL reconstruction have been described [14]. The procedure is suitable for a patient without significant anterior knee pain, with recurrent episodes of dislocation that are not permanent during flexion, a positive apprehension test and excessive lateral glide and mild patello-femoral arthritis at most. The MPFL reconstruction improves clinical symptoms and reduces the patellar tilt even in the presence of mild trochlear dysplasia or a TT-TG distance over 20 mm without tibial tuberosity medialization [15, 16] (Fig. 8.3).
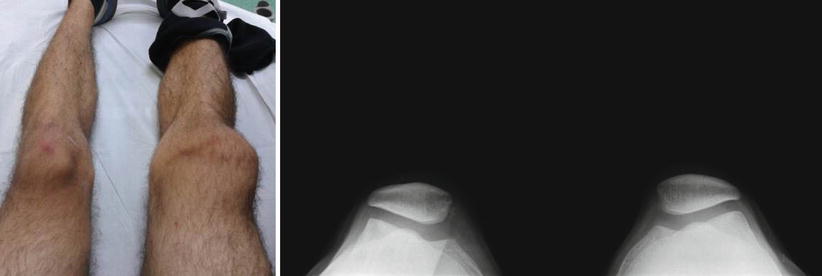
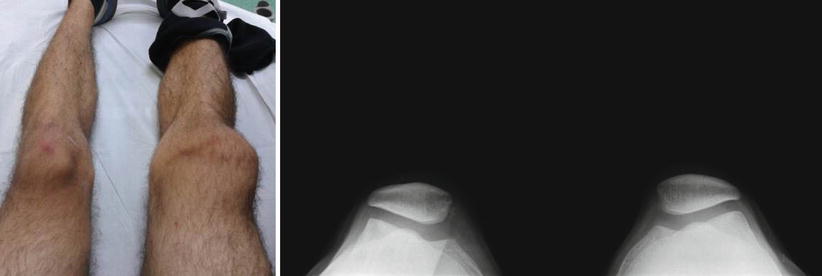
Fig. 8.3
Clinical aspect of recurrent (third) right patellar dislocation during sports. Merchant view shows a Wiberg type III patella, a wide trochlear groove angle and small bony avulsions on the right medial side
8.2.1 Surgical Technique
The patient is positioned supine with a Tourniquet cuff on the thigh and in the leg holder. The operating table can be complete or with the leg support dropped, leaving the knee flexed and the leg hanging down freely. The femoral tunnel is recommended to be checked intraoperatively with radioscopic imaging and thus a true lateral view of the distal femur should be possible when the patient is positioned and before sterile draping.
Standard arthroscopic anterolateral and anteromedial portals are used to confirm the inappropriate patellar tracking and explore the articulation. An accessory superolateral portal can facilitate examination of the patella in the trochlea as well as document postoperative reduction.
The most commonly used graft is the semitendinosus (semi T). The gracilis may not have sufficient length routinely but otherwise can also be used. The harvest is usually performed in the same fashion as for ACL reconstruction (see Sect. 3.7.1). Alternatively, the hamstrings can be harvested by slightly extending the incision made for the femoral fixation. A 24 mm long free semi T is cleaned of remaining muscle and 4 (2 cm) looped traction sutures (No.2 non- or absorbable) are saw on both free ends. It is than sized single and double (looped) for adequate tunnel accommodation.
A vertical incision is made on the medial side of the patella (3 cm). The dissection is advanced deeper but proud of the knee capsule (remains extraarticular). This vertically oriented ligament is found between layers 2 and 3, together with the medial collateral ligament. The patellar attachment of the MPFL is wider and located approximately at the junction of the upper and middle thirds of the patella, where the medial border becomes more vertical. The patellar bone is exposed and two tunnels are drilled 1 cm apart, close to the articular surface. These are used for the patellar attachment, which can be done either by transosseous tunnels or anchors. If the later is chosen, the 4.5 mm tunnels are advanced to a depth of 1 cm with exit holes on the anterior cortex of patella. This way the fracture risk is reduced, compared to drilling all the way through the lateral border. The graft is than attached to the patella at the middle of the loop using two anchors (Fig. 8.4);
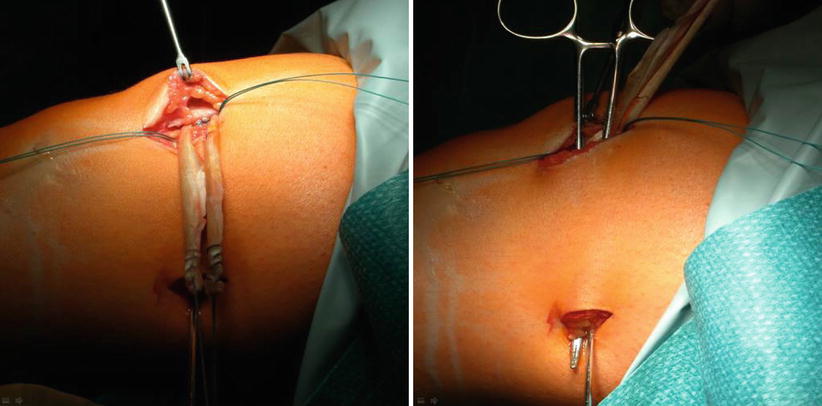
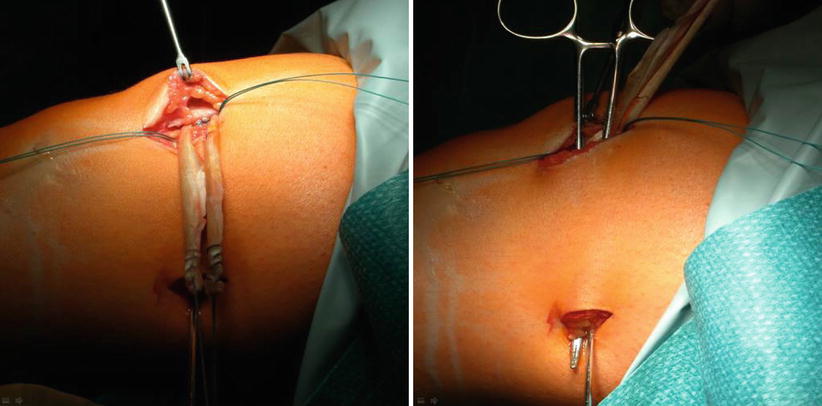
Fig. 8.4
The graft is attached to the patella using 2 anchors; leader sutures are than passed using a small forceps between layers 2 and 3
A small (2 cm) incision is made between the adductor tubercle and the medial epicondyle. These structures usually can be palpated with the knee flexed to move the hamstrings posteriorly. The MPFL attaches to the femur in the saddle between the medial epicondyle and the adductor tubercle: 10 mm proximal and 2 mm posterior to the medial epicondyle or approximately 4 mm distal and 2 mm anterior to the adductor tubercle [13]. Dissection is carried deeper to expose the bone in the saddle created between these two structures. A pin with a loop for suture passage (from the ACL instrument set) is placed in the femoral insertion and the position is checked with intraoperative radioscopy (Fig. 8.5). For safer passage, it should be slightly angled proximal and anterior. This positioning is one of the most critical steps of the procedure. It should lie proximal to the intersection of the Blumensaat line and the posterior femoral cortex, along a line extending distal from the posterior cortex of the femoral shaft on a true lateral view (both condyles overlapping). Schöttle et al. found this radiographic location to be situated 1 mm anterior to the posterior cortex line, 2.5 mm distal to the posterior origin of the medial femoral condyle and proximal to the level of the posterior point of the Blumensaat line (Fig. 8.6) [20]. A forceps is passed from the femoral attachment between the layers and the sutures along with the graft are passed. By temporarily securing the graft to the pin a check of the reduction and the isometry can be performed.

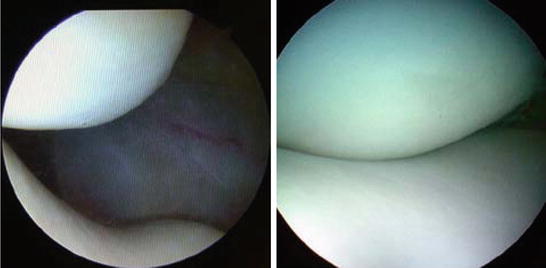

Fig. 8.5
The radiographic landmarks of the femoral insertion according to Schöttle et al.; a pin is placed in the femoral insertion and the position is checked with intraoperative radioscopy
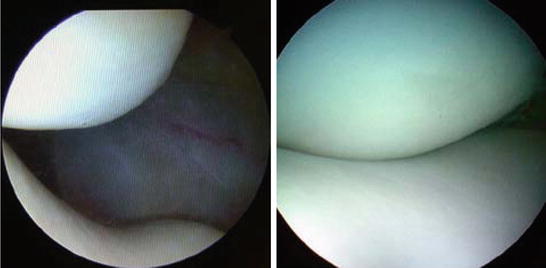
Fig. 8.6
Arthroscopic view through the anterolateral portal before and after MPFL reconstruction
The femoral positioning should allow for a relatively isometric behavior throughout the range of motion. The pin is then advanced through the lateral femoral cortex and an appropriately sized 20 mm tunnel is drilled. The graft’s leader sutures are passed through. The tension is decided by pulling on the graft traction lines from the lateral side. It should not overload the patello-femoral compartment. Physiologic (less than 2 quadrants or 10 mm) lateral glide should be possible with the knee extended after reconstruction. The free ends are then secured in the femoral tunnel with the corresponding interference screw. Postoperatively, the patient is immobilized and weight-bearing is limited for the first 2 weeks. Range of motion exercises are started as soon as possible.
The isometric femoral fixation will pass near the open physes in skeletally immature patients. Alternative techniques have been described for pediatric patients, which use the adductor tendon. The graft is passed around the most distal portion, forming a sling. This way there is no interference with the growth physes. The position closely resembles the true isometric position of the native MPFL, although the result is a graft attached slightly more proximal.
8.3 Distal Realignment
8.3.1 Patellar Height
High riding patella is a cause of instability due to inappropriate entry in the trochlear groove during flexion initiation. There are three commonly used indexes to measure the position of the patella to the articular surface:
The Insall – Salvati ratio is defined by distracting the length of the patellar tendon from the maximum length of the patella in the sagittal plane. The normal value is between 0.8 and 1.2. The main drawback is that this ratio does not relate the height of the patella to the articular surface if the tibial tubercle insertion is abnormal.
Blackburne and Peel used [4] the ratio of the articular length of the patella to the height of the lower pole of the articular cartilage above the tibial plateau. Normal values were found between 0.54 and 1.06 [5].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








