Partial Tears of the Scapholunate Ligament
15.1 Introduction
Partial damage of the scapholunate ligament causes chronic wrist pain. Its evolution (natural history) is poorly understood and controversial and its treatment is still the subject of debate. The aim of this chapter is to enable you to treat patients with this type of lesion, from the initial diagnosis to the various therapeutic options currently available.
15.2 Anatomy and Pathophysiology
This chapter gives a brief reminder of the anatomy and role of the scapholunate ligament. For Sokolow and Saffar,1 the scapholunate is traditionally divided into three parts. The anterior part, starting with the ligament of Testut, is richly vascularized thanks to that ligament, which corresponds to a neurovascular bundle. The anterior part, essentially made up of collagen fibers, is the largest zone of the scapholunate ligament and seems to play a proprioceptive role. The intermediate part is not vascularized and is similar to fibrocartilage. Nontraumatic perforations of degenerative origin can affect this zone. Lesions in this central zone can occur without compromising the stability of the carpus or causing pain. The posterior part of the scapholunate ligament is thicker and plays a greater stabilizing role. It is twice as resistant as the anterior part.
Recent anatomical research2 has isolated an anatomical structure linking the dorsal part of the scapholunate ligament to the dorsal capsule: the dorsal capsuloligamentous scapholunate septum (DCSS). It is the dorsal reflection zone of the scapholunate ligament. Everything indicates that the DCSS plays a key role in scapholunate stability. We know that an isolated tear of the scapholunate seems insufficient to cause instability and the development of osteoarthritis. A lesion affecting the ulnar ligament and the DCSS would be required to observe the onset of scapholunate diastasis (▶ Fig. 15.1 and ▶ Fig. 15.2).
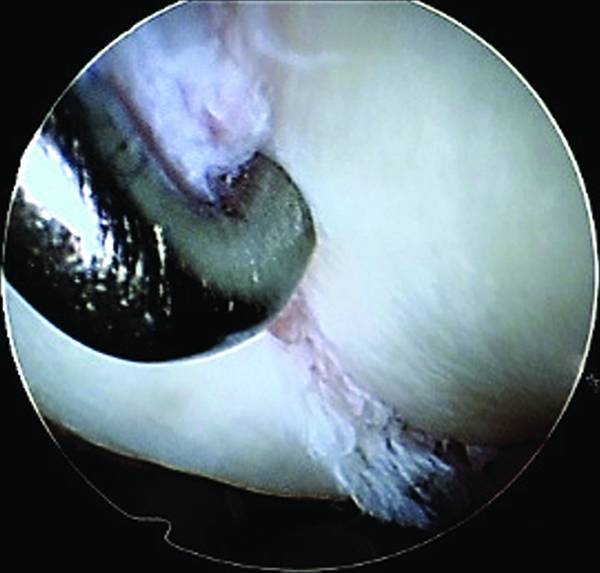
Fig. 15.1 Total fresh rupture of the scapholunate ligament (radiocarpal view).

Fig. 15.2 Same patient as in ▶ Fig. 15.1, midcarpal view: it is impossible to introduce the probe between the scaphoid and the lunate.
15.3 Natural History and Definition of a Partial Tear of the Scapholunate Ligament
The impact of a tear of the scapholunate ligament remains uncertain because of the lack of knowledge of scapholunate tears and their progression. Watson and Ballet3 showed that static instabilities inexorably develop into radiocarpal then midcarpal arthropathy, but we do not know the natural progression of predynamic instabilities. O’Meeghan4 followed 11 patients (12 wrists) suffering from an injury to the scapholunate ligament confirmed by arthroscopy (grades 1 and 2 according to the Kozin classification) with an average follow-up of 4.5 years (2.5–11 years). There were predynamic instabilities, with no radiological scapholunate diastasis. The common denominator of these patients, apart from the ligamentary tear, was that they had refused additional surgery. At the last visit, only one patient showed onset of radiocarpal osteoarthritis; there was no radiological modification in the other patients. Out of the 11 patients studied, all except one had to change profession and give up sports. Finally, the 11 patients continued to suffer with a decrease in articular strength and amplitude in relation to the contralateral side. This work has the merit of underlining the clinical impact of a partial injury of the scapholunate ligament with no radiological sign of destabilization of the carpus (predynamic damage). This is an important notion: a low-grade ligamentary lesion with no initial instability can lead to chronic pain, with a more or less rapid osteoarthritic progression, and have significant repercussions in everyday activities.
The second aspect of our lack of knowledge concerning scapholunate tears is the actual definition of a partial tear of the scapholunate ligament.
The definition usually reserved for a partial tear of the scapholunate ligament is a lesion of one of the three parts of the scapholunate ligament (anterior, intermediate, posterior); a complete lesion corresponds to the simultaneous damage of the three segments.
In their anatomical work, Van Overstraeten et al2 reported the existence of a dorsal bridge connecting the scapholunate ligament to the dorsal capsule: the DCSS. They showed that the detachment of the DCSS was required to obtain scapholunate diastasis; an isolated tear of the scapholunate ligament (three parts) did not lead to diastasis.
Mathoulin et al5 reported a series of repairs of scapholunate ligament tears by simple arthroscopic capsular suturing, with good results. The area sutured by arthroscopy corresponds to the DCSS described by Van Overstraeten et al.2
From these anatomical and clinical studies, it seems that the accepted definition of a partial tear of the scapholunate ligament is a tear affecting one or several compartments of the scapholunate ligament, but with no damage to the DCSS.
15.4 Diagnosis of a Partial Tear of the Scapholunate Ligament
The diagnosis can be made at the acute stage after wrist trauma or at the chronic stage, that is, at least 3 months after the wrist trauma, owing to persistent pain. The classic clinical sign is pain on the dorsal edge of the wrist, next to the scapholunate ligament, 10 mm distally in relation to the Lister tubercle. This pain is enhanced during effort and with forced flexion and extension. The differential diagnosis can be a subretinacular cyst or extensor tenosynovitis. The Watson test described for detecting scapholunate instability is rarely positive in the early stages (predynamic instability).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








