Chapter 196 Parkinson’s Disease
 Diagnostic Summary
Diagnostic Summary
Motor symptoms are considered cardinal in Parkinson’s disease (PD)1:
• Tremor—The most common parkinsonian feature is a resting tremor, maximal when the limb is at rest and diminishing with voluntary movement and sleep. The tremor affects to a greater extent the most distal part of the extremity; it is typically unilateral at onset, becoming bilateral as the disease progresses. Approximately 30% of PD sufferers do not have tremor at disease onset, yet most develop it as disease progresses.
• Joint stiffness and increased muscle tone—Combined with a resting tremor produces a ratchety “cogwheel rigidity” when the limb is passively moved.
• Slow movement (bradykinesia) or inability to move (akinesia)—Produces difficulties not only with the execution of a movement but also with the planning and initiation of movement. Performance of sequential and simultaneous movements is also hindered. For many, bradykinesia is the most disabling symptom in the early stages of PD.2
• Postural instability is typical in the late stages of PD, leading to impaired balance and frequent falls. It is often absent in the initial stages of disease, especially in younger patients.
• “Pill rolling” motion of the thumb and forefinger.
• Stooped posture, progressively shortened and accelerated steps that get progressively faster and may end up in a fall (“festinating gait”).
• Reduced or fixed facial expressions (“masked face”); low-volume or monotone voice or both.
• Small handwriting (micrographia) that decreases in size toward the end of a writing sample.
• Gastrointestinal symptoms: Constipation is often one of the earliest symptoms, with difficulty swallowing (dysphagia) common later in the disease course.
Neuropsychiatry
• Cognitive disturbances are being increasingly recognized as symptoms of PD. Although they can occur early in PD, cognitive deficits progress with the course of disease, leading to dementia in about 80% of cases,3,4 by the tenth year. Most common cognitive deficits include the ability to make decisions and adapt to new environments, poor problem solving, fluctuations in attention, slowed cognitive speed, and memory problems—specifically in recalling learned information, with an important improvement when cues are given.
• Alterations in behavior and mood, including depression, apathy, and anxiety. Poor impulse control can result in behaviors such as punding, binge eating, craving, hypersexuality, or pathologic gambling. These are likely related to a dopamine dysregulation syndrome often associated with the medications for PD.1
• Psychotic symptoms, such as hallucinations or delusions, can be common in later PD.1
 General Considerations
General Considerations
Epidemiology
First described by James Parkinson in 1817, PD occurs in approximately 0.3% of the general population and about 1% of the population older than 60 years of age in industrialized countries.2,5
This progressive neurologic disorder results from a deterioration of neurons in the substantia nigra. This creates a shortage of the neurotransmitter dopamine, causing the impairments that characterize the disease. People with PD often experience limb tremor, muscle rigidity, difficulty walking, and problems with balance and coordination. According to the Parkinson’s Disease Foundation, PD affects more than 7 million people worldwide and at least 1 million in the United States.5 About 50,000 new cases are reported annually in the United States. These figures are expected to increase as the average age of the population increases. The disorder appears to be slightly more common in men than women, with whites being 1.5% more likely to contract PD than African or Asian populations in industrialized countries.
Pathophysiology
As with most neurodegenerative diseases, oxidative and nitric oxide stress, inflammation, and mitochondrial dysfunction are the primary contributors to cell death. A decrease in glutathione concentrations, the brain’s primary antioxidant, is the earliest reported biochemical event to occur in the parkinsonian substantia nigra. Mitochondrial dysfunction has been implicated ever since it was observed that an inhibitor of complex I of the electron transport chain can induce parkinsonism. Recent research indicates that several PD-associated genes interface with pathways regulating mitochondrial function, morphology, and dynamics. Sporadic and familial PD may converge at the level of mitochondrial integrity.6
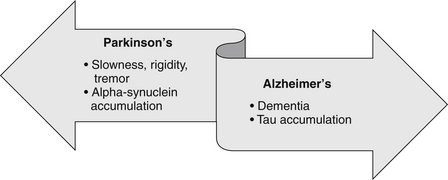
Several neurodegenerative disorders have excessive protein deposition as a common pathophysiologic mechanism; the primary differences being the location of deposition and/or the protein(s) that accumulate (Figure 196-1).
Substantia Nigra Cell Death
Apoptosis accounts for much of the pathology seen in PD as well as in diseases like Alzheimer’s disease, Huntington’s disease, and amyotrophic lateral sclerosis (Lou Gehrig’s disease), which are marked by the loss of brain neurons. Elevated apoptosis in these neurologic diseases seems to be related to a lack of production of nerve growth factor and to free radical damage. A combination of such factors could likely cause many cells to destroy themselves. Manipulation of this process of apoptosis may help in treating these neurologic diseases. In fact, studies in animal models imply that long-term delivery of nerve growth factors could protect against programmed cell death in these conditions.7–9 Until the mechanisms of apoptosis are elucidated, some natural therapeutics that may decrease programmed cell death, such as melatonin therapy, may be of benefit in PD (see further discussion of melatonin later).
Oxidative Stress and Glutathione Deficiency
Biochemical changes including increased levels of neurotoxic metals, the inhibition of mitochondrial complex I activity, and depleted glutathione levels occurring in the substantia nigra10 all suggest that oxidative stress is present and pathologically involved in PD patients.11 Using healthy patients as a control, studies in patients dying from PD have observed 40% reduced glutathione levels in these patients, whereas oxidized glutathione was insignificantly marginally elevated.12 Depletion of glutathione levels in the brain may be an early component of the disease process, because these suboptimal levels have also been found to occur in presymptomatic PD, also known as incidental Lewy body disease.13
Some researchers are finding that this glutathione deficiency may be a common denominator in all parkinsonian conditions associated with nigral damage.10 Although not completely elucidated, it is known that glutathione exhibits several functions in the brain by acting as an antioxidant and a redox regulator. Glutathione depletion has been shown to affect mitochondrial function probably via selective inhibition of mitochondrial complex I activity. Oxidative damage due to glutathione depletion may also encourage the aggregation of defective proteins, leading to cell death of nigral-striatal dopaminergic neurons.11
Glutathione depletion may enhance the susceptibility of substantia nigra to destruction by endogenous or exogenous toxins. Restoring antioxidant levels within the brain may be a valuable therapeutic strategy for PD.10
Environmental Exposures
Epidemiologic studies and animal experimental models have identified an association between PD and the following environmental risk factors: rural residence, farming, well-water drinking, exposure to pesticides (including organochlorines, carbamates, paraquat, maneb, rotenone, and diethyldithiocarbamate), and long-term occupational exposure to copper, iron, lead, and manganese.14 Additionally, it is possible that the pesticides and metals act synergistically with other exposures to increase the risk of PD.15–18 Another example of environmental exposure is iatrogenic parkinsonism caused by exposure to central dopamine antagonists. The literature for these associations is provided below.
MPTP
The first hint that PD may be related to an environmental toxin came from a report based on a series of patients who developed parkinsonism after exposure to 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP), a contaminant found in synthetic heroin.19 It was found that MPTP can freely cross the blood–brain barrier, is selectively taken up by dopaminergic cells, and inhibits mitochondrial complex 1 function in the respiratory chain, an established factor in the PD pathophysiology.20 MPTP is the only environmental agent that has been directly linked to the development of levodopa-responsive parkinsonism, a form that is clinically indistinguishable from PD.1
Rotenone
Rats exposed to the organic pesticide rotenone develop parkinsonian symptoms as well as changes in the brain resembling those seen in PD in humans. Mimicking the effect of MPTP, rotenone works by inhibiting complex I of the mitochondrial respiratory chain. It was observed that chronic, systemic inhibition of mitochondrial complex I by the lipophilic pesticide rotenone can cause highly selective nigrostriatal dopaminergic degeneration that is associated behaviorally with hypokinesia and rigidity. Additionally, nigral neurons in rotenone-treated rats accumulate fibrillar cytoplasmic inclusions that contain ubiquitin and α-synuclein.21 These inclusions are the major constituent of intracellular protein inclusions forming the Lewy bodies and Lewy neuritis in dopaminergic neurons of the substantia nigra. Other studies have also shown that chronic administration of rotenone over a long period can increase nitric oxide and lipid peroxidation products in the brain cortex and striatum in rats, which then clearly mimic parkinsonian behavioral symptoms such as akinesia and rigidity.22 Interestingly, rotenone is a natural pesticide and until very recently was allowed to be used in organic produce.
A 2009 case-controlled multicenter study analyzed the effect that occupation had on PD risk. Occupational pesticide exposure emerged as the most consistent etiologic association with parkinsonism. In experimental settings, the three specific pesticides identified (2,4-dichlorophenoxyacetic acid, paraquat, and permethrin) all have effects on dopaminergic neurons. This convergence of epidemiologic and laboratory data from experimental models of PD lends credence to a causative role of certain pesticides in the neurodegenerative process.23
Maneb and paraquat, two widely used pesticides, have been associated with PD. Researchers studied pesticide exposure in California’s Central Valley and found that when people were exposed to both maneb and paraquat within 500 meters of their homes, their likelihood of being diagnosed with PD was substantially increased as compared with those without exposure. The majority of the risk for being diagnosed with PD was attributed to exposure between 1974 and 1989—and all those so exposed were then children, teenagers, or young adults. This group of people, who had younger-onset PD (meaning that they were diagnosed before the age of 60), were four to six times more likely to develop PD if they were exposed to both pesticides.24
Solvents
Some case-control studies and case reports have shown an association between solvent exposure and parkinsonism.25 Records from a major United Kingdom engineering company were culled in order to explore the relationship of metal and solvent exposure and PD. The results of this survey demonstrated a significant exposure-response relationship for solvents and almost a 400% increase in risk for employees exposed for 30 years or more. This study suggests that sustained cumulative exposure is probably significant because there was no evidence of overall increase in risk for those exposed for shorter durations. The authors noted that possibly the more heavily affected workers experienced exposure before the introduction of stricter industrial environmental controls later in the twentieth century or exposure to older solvents such as trichloroethylene, 1,1,1-trichloroethane, carbon tetrachloride, kerosene, white spirit, and acetone, which were more widely used three or more decades ago and may have played a greater etiologic role.26
Although the study mentioned previously showed no increased risk of PD in relation to metal exposure, occupational exposure to specific metals—especially manganese, copper, lead, iron, mercury, zinc, and aluminum—appears, based on epidemiologic studies, to be a risk factor for PD.27 Elevated levels of several of these metals have also been reported in the substantia nigra of PD subjects. Like pesticides, several divalent and trivalent metal ions are also found to contribute to accelerations in the rate of α-synuclein fibril formation. In one study, aluminum contributed to fibril formation, along with the chloride salts of copper2+, iron3+, cobalt3+ and manganese2+.27 Chronic mercury inhalation has also been linked to cortical and cerebellar atrophy, dementia, Parkinson’s disease, and ataxia of the lower limbs.28
Manganese
Manganese toxicity is different than PD, but the two present very similarly. With toxicity, manganese-induced damage is found in the substantia nigra, globus pallidus, and caudate nucleus with depletion of dopamine and serotonin levels and has been linked to psychiatric changes followed by impaired motor activity with muscle rigidity and tremors.14
Welders, who are commonly exposed to substantial amounts of manganese, do not have a higher incidence of PD, but they do appear to develop the disease approximately 11 years before most other PD patients do. Other sources of manganese include well water and industrial waste. Unfortunately, it is not routine to assess manganese levels in patients presumed to have PD, and little research has been done on chronic, low-level exposure to ambient manganese (i.e., from industrial waste.) As imaging techniques improve and become more readily available, it will be easier to differentiate manganism from PD.
Iron
Iron accumulation has been related to neurologic disorders such as Alzheimer’s disease, PD, type I neurodegeneration with brain iron accumulation, and others. Increased levels of iron as well as accompanying lipid peroxidation combined with a decreased level of glutathione and superoxide dismutase activity are present in the substantia nigra of patients with PD.11,29 Although it is unclear whether the accumulation of iron in the brain is primary or secondary to the development of neurodegenerative disorders,30 one animal study has shown that unilateral injection of FeCl3 into the substantia nigra of adult rats results in a 95% decrease of striatal dopamine, which impaired dopamine-related behavioral responses. This supports the assumption that iron may trigger the dopaminergic neurodegeneration of PD.31
Detoxification Dysfunction
The role of xenobiotic metabolizing enzymes (XMEs) in the disease etiology of PD has been under investigation by numerous researchers for the last two decades. The association of a number of defects in both phase I and phase II reactions with PD and motor neuron disease has been extensively studied. It has been demonstrated by in vivo or in vitro methods and by the functional genomics of XMEs and neurodegenerative diseases that PD and motor neuron disease (MND) can be associated with problems in xenobiotic metabolism; moreover, it appears that 38% to 39% of patients with MND/PD have a defect in the S-oxidation of the mucoactive drug carbocysteine by an unknown cytosolic oxidase. This implies that in a significant number of PD patients there may be an underlying dysfunction in the body’s ability to detoxify.32
This dysfunction theoretically could lead to an increased vulnerability to neurotoxins following exposure to sulfur-containing substances.33 Connections with Alzheimer’s disease and other motor neuron diseases have also been made.34 Certainly genetic determination is but one factor and must be looked at in light of the strong support that has been found for the roles of nutritional and environmental factors, discussed elsewhere in this chapter.35
 Therapeutic Considerations
Therapeutic Considerations
Conventional Medicine
Unfortunately, no conventional therapy has been shown to modify the progressive pathology of degeneration in PD.36 However, PD symptoms are somewhat treatable. For decades, the drug levodopa, commonly known as L-dopa, has been the mainstay of PD treatment. It is synthesized by the enzyme tyrosine hydroxylase from the food-derived aromatic amino acid tyrosine. Modern treatment combines L-dopa with a peripheral decarboxylase enzyme inhibitor to minimize conversion of L-dopa to dopamine outside the nervous system.29
Although initially effective in the early stages of the disease, L-dopa provides only symptomatic relief without altering disease progression, and it loses efficacy with time.2 The side effects of L-dopa can include motor complications, particularly fluctuations and dyskinesias, as well as nausea, vomiting, orthostatic hypotension, sedation, hallucinations, and delusions; moreover, L-dopa contributes to decreased slow-wave peristaltic activity,37 which may contribute to inadequate digestive function. It may also contribute to subtle detrimental effects on cognitive function38 and may have a wide array of other psychiatric manifestations, such as propensity to gamble.39 Responses to the drug may become more erratic over time. For these reasons, newer drugs are now also used either alone or in combination with L-dopa. Proper concomitant naturopathic care can drastically reduce the side effects of L-dopa. It is important to emphasize that in spite of the side effects, this drug is excellent for controlling symptoms and must be considered as part of the overall treatment plan.
After being virtually abandoned for 20 years, another allopathic treatment that is gaining more prominence is deep brain stimulation (DBS). DBS involves implanting a brain stimulator, a device similar to a heart pacemaker, in a certain area of the brain. The desired effect is to decrease the overactivity of the excitatory glutamatergic subthalamus–internal pallidum pathway caused by the loss of dopaminergic neurons within the substantia nigra. How DBS works is not well known, but it has been hypothesized that the stimulatory effect may modulate the neuronal activity and thus avoid disease-related abnormal neuronal discharges. Potential candidates for DBS are selected according to strict criteria. For some people, DBS may control symptoms so well that medications can be greatly reduced.40
Diet
Healthy dietary habits might be useful to treat and prevent PD. One large case-control study41,42 revealed that PD patients tended to consume fewer raw vegetables, less alcohol and coffee, and more meat than control subjects. Patients with PD also reported higher carbohydrate consumption and equivalent intakes of protein and fat. Other researchers have shown an increased consumption of animal-source fat in patients with PD.43–45 Although researchers need to learn more about how food choices relate to PD, a higher intake of vegetables and a low intake of fat seem to be reasonable choices in helping to prevent and possibly treat neurodegeneration.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree