Palpitations and Arrhythmias (Case 6)
Arzhang Fallahi MD and Michael Kim MD
Case:
An ECG reveals a narrow complex tachycardia at 135 bpm, irregularly irregular with no P waves and no delta waves; aVL shows a QRS complex of 12 little boxes in height; no other ST elevations or depressions are noted.
Speaking Intelligently
The approach to a patient with palpitations is as follows:
1. Assess airway, breathing, and circulation with IV access, oxygen administration, and cardiac monitoring; with a 12-lead ECG; and with initial blood work (including troponin concentrations).
2. Clinically assess associated signs of the tachycardia: hypotension, heart failure or pulmonary congestion, shortness of breath, renal failure, shock, altered mental status, angina, or acute myocardial infarction. A quick assessment of vital signs must be made even before one takes a detailed history. Ultimately, is the patient stable or unstable? Arrhythmias such as ventricular tachycardia, ventricular fibrillation, or any heart rhythm with profound hypotension are a medical emergency, which may require immediate management.
3. The history of the palpitations is a key point. Is this new? Does the patient have a history of cardiac arrhythmias? Is the patient on any medications that may contribute? Are the palpitations associated with any chest pain? Is there any history of thyroid disease? The underlying cause of the tachycardia must be determined from the very outset. Is the patient having an acute coronary event? Does the patient have signs of heart failure or pulmonary disease? Is the patient hypo- or hypervolemic? Is the process acute or chronic in nature?
4. Assess for comorbidities: lung disease (asthma, chronic obstructive pulmonary disease [COPD], pulmonary hypertension, restrictive lung disease), cardiac disease, hypertension, age, diabetes, history of stroke. Comorbidities will help in risk-stratifying the patient, as well as in guiding management.
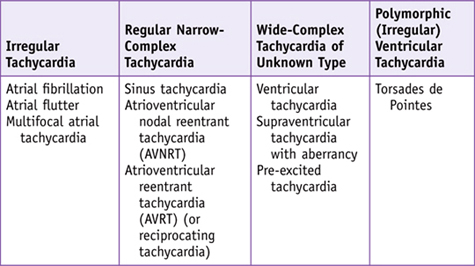
5. The tachyarrhythmia must be quickly assessed using the four main categories listed above to guide subsequent management.
• First and foremost, the patient must be quickly assessed systematically for airway, breathing, and circulation. Prompt IV access, administration of oxygen, and cardiac monitoring should be instituted. A STAT ECG is also critical to guide subsequent management of the tachyarrhythmia.
• Given the clinical presentation, the patient appears to be stable, but with such an elevated heart rate at rest, his condition is tenuous and requires prompt management. The irregular narrow complex tachycardia limits our main differential to atrial fibrillation, atrial flutter, and multifocal atrial tachycardia. Given the complete absence of P waves and no mention of flutter waves, this patient most likely has atrial fibrillation with a rapid ventricular response. This is the most common tachyarrhythmia seen, and given the patient’s age and history of hypertension, with a suggestion of LVH on the ECG, we can be even more confident in our diagnosis.
• The next two steps are to control the rate and determine the underlying cause of the atrial fibrillation. Certain history will help determine therapeutic options. Does the patient have normal LV function? Does the patient have Wolff-Parkinson-White syndrome? Is the duration of symptoms less than or more than 48 hours? Is anticoagulation indicated? Can the patient undergo electrical cardioversion safely, or would pharmacologic conversion be preferable? What is the risk of embolization? Is the ventricular rate too high?
• The patient is not hypotensive and shows no signs of heart failure. However, given his age and chronic symptoms, it is unclear if his symptoms have been going on for 48 hours or more. Together, this increases his risk for embolization; therefore, electrical cardioversion would not be the best initial option. One must look at comorbidities in determining which pharmacologic agent to use. Atrioventricular (AV) nodal agents such as β-blockers or calcium channel blockers are important for rate control, while amiodarone is one of the main agents used for rhythm control. In patients with severe asthma, β-blockers may exacerbate the condition, and in patients with heart failure and hypotension, calcium channel blockers can result in decompensation. In patients with severely reduced ejection fraction, agents such as digoxin, in combination with AV nodal agents, may be of benefit.
• There are various precipitants of atrial fibrillation, but initially acute coronary syndrome must be ruled out. Monitoring for signs of angina and elevated cardiac markers is crucial. Hypo- or hypervolemia may also trigger atrial fibrillation. Use of sympathomimetic agents such as caffeine, amphetamines, and cocaine can also trigger tachycardia and must be considered.
• Determine when the palpitations started and what triggered them. Associated symptoms, such as chest pain, may suggest an acute coronary event. Other contributing symptoms such as shortness of breath, leg swelling, and paroxysmal nocturnal dyspnea may suggest CHF. Symptoms such as weight loss and heat intolerance may suggest an endocrine etiology such as hyperthyroidism. The time course of symptoms is also important. Is this acute, chronic, or intermittent?
• Risk stratification, such as patient age, history of CHF, diabetes, and history of stroke, will help guide subsequent management.
• Medications, diet, and social history: Has the patient taken any medications that may have contributed to tachycardia? Does the patient have a history of illicit drug use?
• Vital signs: Assess the patient’s heart rate, and check for hypertension or hypotension. The patient should also be assessed for respiratory distress and oxygen saturation. Monitor the patient’s temperature to see if infection may be the cause for the underlying condition.
• General appearance: Examine for diaphoresis, respiratory distress, and signs of shock for potential hypotension requiring immediate intervention.
• Respiratory exam: Listen to breath sounds bilaterally to make sure they are symmetric, and listen for any signs of fluid accumulation from either pulmonary and/or cardiac dysfunction or other diseases. Percussion may help identify areas of consolidation.
• Cardiac auscultation (to determine if rate is regular or irregular): Determine whether the heart sounds appear distant, which may suggest a pericardial effusion; assess for murmurs and abnormal heart sounds, since an S3 gallop may indicate CHF or a dilated chamber, while an S4 gallop may indicate the stiff LV of hypertensive heart disease. Look at neck veins to see if they are elevated, which may indicate volume overload or an inability to adequately distribute blood volume.
• Vascular auscultation (carotid bruits): to assess atherosclerotic status.
• Abdominal examination: Assess that there is no evidence of an acute abdomen or possible gastrointestinal hemorrhage, which could have led to the tachycardia.
• Neurologic examination: Quickly assess patient’s mental status to determine if there is adequate perfusion of the brain. A screening neurologic exam should be performed to see if there are any focal deficits that might preclude use of anticoagulation therapy.
• Extremities: Check to see if extremities are warm to assess perfusion.
Only gold members can continue reading.
Log In or
Register to continue
Related
Stay updated, free articles. Join our Telegram channel
Join