Pain is one of the most common, severe, and treatment-resistant complications that follows SCI. Recent years have seen a surge of research on methods for assessing and treating spinal cord injury pain. In this article, pain after SCI is reviewed in terms of nature, scope, assessment techniques, and treatment strategies.
Pain is common enough after spinal cord injury (SCI) to be considered an expected condition. Recent studies estimate the prevalence of pain after SCI to be between 77% and 81% . Moreover, for many persons with SCI this pain is severe and has significant impact on daily functioning. Studies using standardized measures suggest that the intensity of pain is severe for between 20% and 33% of persons with pain after SCI . Moderate to severe pain-related disability is found among 29% to 40% of persons with SCI who have pain . The importance of pain to persons with SCI is further underscored by research that has consistently implicated pain in outcomes such as reduced quality of life, functional impairments, and depression . Some studies have suggested that the impact of pain on quality of life (QOL) may be greater than that of the injury itself . Pain conditions among persons with SCI tend to be stable over time, across studies with follow-up periods ranging from 2 to 10 years . In fact, changes in a pain condition that do occur over time after SCI are likely to assume a worsening course .
Spinal cord injury pain types and taxonomies
SCI pain manifests in a multiplicity of forms; the typical patient experiences numerous types of pain that differ by location, qualitative descriptors, and purported etiology . The complexity of SCI pain has direct bearing on its broad impact on functioning and resistance to treatment. Essential to clinical care of pain after SCI is the development of methods for rendering pain less mysterious and confusing, namely, valid and reliable methods for characterizing and categorizing pain. Development of valid and reliable SCI pain taxonomies has long been the aim of researchers. The sheer number of taxonomies that have been developed, and inconsistencies between taxonomies, underlines the complex and frustrating nature of pain after SCI. This section of the article will focus on common characteristics of the taxonomies and highlights a number of categorical systems that have been the subject of empirical studies of reliability.
Numerous pain types associated with spinal cord injury have been identified, primarily based on alleged causes, location of pain, and pain descriptors. Most taxonomic systems share two basic categories of pain after SCI: musculoskeletal/nociceptive and neuropathic/neurologic. As a major category, neuropathic pain is prevalent in 30% to 40% of persons with SCI five or more years after injury . Musculoskeletal pain appears to be more common, occurring in 50% to 60% of persons with SCI five or more years after injury . However, when “worst” SCI pains are identified, the majority (50% to 56%) are likely to be neuropathic, as opposed to musculoskeletal . SCI pain types and subtypes are presented in Table 1 according to the major classification systems.
| Bryce/Ragnarsson | Cardenas | Donovan | IASP | Tunks |
|---|---|---|---|---|
| Above level | Neurologic | (1) Segmental | Nociceptive | Above level |
| (1) Nociceptive | (1) Spinal cord | (2) Spinal cord | (1) Musculoskeletal | (1) Myofascial |
| (2) Neuropathic | (2) Transition zone | (3) Visceral | (2) Visceral | (2) Syringomyelia |
| At level | (3) Radicular | (4) Mechanical | Neuropathic | (3) Non–spinal cord injury |
| (3) Nociceptive | (4) Visceral | (5) Psychogenic | (3) Above level | At level |
| (4) Neuropathic | Musculoskeletal | (4) At level | (4) Radicular | |
| Below level | (5) Mechanical spine | (5) Below level | (5) Hyperalgesic border reaction | |
| (5) Nociceptive | (6) Overuse | (6) Fracture | ||
| (6) Neuropathic | (7) Myofascial (incomplete) | |||
| Below level | ||||
| (8) Diffuse burning | ||||
| (9) Phantom | ||||
| (10) Visceral | ||||
| (11) Myofascial (incomplete) |
Musculoskeletal pain refers to pain originating from damage to tissue and bone structures and may include the following pain subtypes. In the immediate aftermath of injury the sources of pain may be obviously related to bone, joint, and tissue trauma. Also, pain may stem from fractured vertebrae and torn ligaments that destabilize the spine. Pain related to spine instability is affected by positioning and activity. Muscle spasm pain may arise long after the injury. Overuse pain, or pressure syndromes, typically occur in areas of normal sensation and high activity, such as the shoulder.
Neuropathic pain (also called neurologic or central pain) is directly attributable to spinal cord damage and has been divided further into a number of subtypes. One subtype of neuropathic pain, SCI pain, is typically perceived below the level of injury in areas without normal sensation. Transition zone pain occurs at the level of injury and may include pain caused by nerve entrapment. Radicular pain is neuropathic pain occurring at the level of injury caused by nerve root damage related to the initial injury or subsequent irritation. Visceral pain occurs in the abdominal region, typically well after initial injury and often in the absence of visceral pathology. Visceral pain is considered neurologic/neuropathic in some classification systems. However, causes of visceral pain can include conditions such as bowel and urinary tract obstruction, renal calculi, or other intra-abdominal pathologies, suggesting that visceral pain may be categorized better as nociceptive pain in some cases.
Reliability of spinal cord injury pain classification schemes
Although there are numerous ways to determine a classification system’s reliability, most studies have focused on interrater reliability, meaning the degree of agreement between two raters of the same variable. Reliability of a pain classification system is fundamental for determining the system’s validity, meaning the degree to which the system is measuring what it purports to measure. Interrater reliability is commonly indexed as a Kappa coefficient, having a range from −1.0 to 1.0, with 1.0 indicating perfect agreement between raters. Values greater than .60 or .70 are considered to represent adequate interrater reliability. As seen in Table 2 , the interrater reliability of major SCI pain classification systems has been modest, at best, across independent studies. Across classification systems, raters disagree on the classification of between 20% and 50% of pain sites. The apparent differences in performance of these classification systems may be caused by variability in the complexity of systems in terms of how many pain types and subtypes are included. As noted by Putzke and colleagues , the reliability of classification systems increases as the number of pain types decreases. Classification systems show better interrater reliability when broad pain types are considered, such as nociceptive-neuropathic or location of pain relative to injury level . Also, it is important to note that methodologic differences between studies in Table 2 may have bearing on results. Specifically, interrater reliability for the Bryce and colleagues system reflected comparisons between physicians recruited for the study and the investigators themselves. In the study of the Cardenas system, interrater reliability was based on ratings of questionnaire data. However, in a subset of ratings made using information gained from clinical interview and physical examination, the Kappa coefficient was comparable though somewhat reduced (.66 compared with .68 with questionnaire data).
| Kappa coefficient | Percent agreement | |
|---|---|---|
| Bryce and colleagues | .70 | Unavailable |
| Cardenas | .68 | Unavailable |
| Donovan | .55 | 50%–62% |
| IASP | .49 | 52% |
| Tunks | .49 | 27% |
Use of verbal descriptors to categorize pain may also have bearing on the limited reliability of classification systems. Verbal pain descriptors, while being a standard method for classifying SCI pain, actually have limited utility in discriminating between pain types. A number of investigators have found considerable overlap in verbal descriptors for broad pain types. For example, each verbal descriptor (eg, burning, aching, shooting, stabbing, tingling) may be endorsed at least 8% of the time for each of the most common pain types across classification systems . Cardenas and colleagues found that “aching”, a term typically thought to be descriptive of musculoskeletal pain generally and overuse pain specifically, was also used by patients to describe 64% to 67% of pains classified as neuropathic during examination.
Various SCI pain classification systems may be adequate for identifying the two broad types of pain, musculoskeletal and neuropathic, but additional research is required to develop more reliable taxonomic methods.
Psychological aspects of spinal cord injury pain
Absent from most classification systems is the concept of a pain type that is purely psychological in origin. Rather, psychological factors such as mood, thoughts, and social interactions may be considered to have a bidirectional relationship with all types of pain, with particularly important roles in the development of chronic pain and pain-related functional disability . As noted earlier in this chapter, most if not all persons with SCI endure pain on a daily basis for years, and yet only a minority experience clinically meaningful pain-related functional disability. Understanding the differential impact of pain on functioning across individuals is an important goal for research, with direct bearing on allocation of health care resources and the design of more effective interventions. With this aim in mind, numerous investigators have examined what demographic, medical, or SCI-related factors might predict variability in the functional impact of pain. Consistent predictors of pain-related disability have not emerged from these studies, as noted in past reviews that span decades of research . One explanation for the inconsistent findings relates to methodologic problems across studies, such as small sample sizes, cross-sectional designs, and variability in how pain-related disability is defined and measured. Alternatively, consistent findings may be elusive if variability in pain-related disability is largely accounted for by psychological factors. For example, a well-replicated finding in both cross-sectional and longitudinal studies is that psychological factors, such as mood or cognitions, are better predictors of pain interference than injury-related factors such as level, completeness, or etiology of injury .
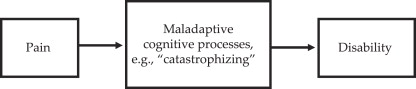
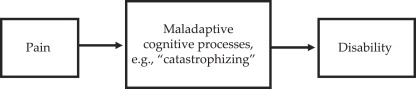
These findings have stimulated research and theorizing regarding explanatory models of psychological factors and pain-related disability. Prominent in this research have been theories emphasizing the role of maladaptive cognitive processes, such as catastrophizing, in the development and maintenance of functional disability related to pain. Catastrophizing refers to exaggerated negative expectations or interpretations of an experience, such as pain . The degree to which one catastrophizes (“I cannot stand this pain! It will never get better!”) is thought to be associated with the impact of pain on outcomes such as functioning and well-being. Strong associations between catastrophizing and functioning have been observed across diverse patient groups while controlling for possible confounds such as pain severity, illness severity, or personality . Consistent with research among other populations, catastrophizing has been shown to be a potent predictor of pain-related functional disability among persons with SCI . Catastrophizing is thought to play a mediating role between pain and functioning in most models. For example, painful stimuli may serve to activate “pain schemas,” or memory stores of knowledge related to pain, that support cognitive-processing biases such as catastrophizing . Biases in cognitive processing may involve enhanced memory for, or attention toward, negatively valenced illness-related information . The effect of cognitive processing biases such as catastrophizing may be to heighten the threat value of pain and highlight inadequacies in personal coping resources, with ultimate impact on activity levels and function ( Fig. 1 ; ).
The impact of pain on psychological adjustment is also important to describe. Cross-sectional, correlational studies consistently show associations between pain and various indicators of psychosocial adjustment after SCI . While this evidence supports causal hypotheses regarding the effect of pain on psychosocial adjustment of persons with SCI, it may be just as likely that psychosocial adjustment is influencing pain. However, prospective studies suggest that pain may precede conditions reflective of psychosocial maladjustment, such as clinical depression .
Assessment of spinal cord injury pain
Medical assessment
Pain assessment procedures that have been detailed elsewhere are reviewed here. Assessment of pain in persons with SCI should begin with classification of the pain according to mechanism to suggest the most appropriate first-line treatment strategies. Most classification systems rely on neurologic level determined by examination and verbal descriptions of pain locations (eg, above, at, or below level) and pain qualities (eg, burning, aching, stabbing). Thus, neurologic examination and a detailed pain interview are arguably the central aspects of SCI pain assessment. However, medical examination should also include general physical, musculoskeletal, laboratory (radiologic, electrophysiologic) and mental status testing. Information should be gathered regarding a patient’s family, psychosocial, and medical histories. A pain history should be taken to understand the characteristics of the pain at onset, circumstances surrounding onset, past treatments, and the course of pain to the present date. The interview should elicit a detailed pain description by the patient, in terms of pain location, distribution, quality, intensity, periodicity, and duration. Factors aggravating or relieving pain should be noted, eg, movement, pressure, heat-cold, or stress. Pain description is accompanied by physical examination of the pain through inspection and palpation of the painful region. Physical examination should also assess for allodynia, hyperalgesia, or hyperesthesia in painful regions using appropriate brush, pinch, pin-prick, or scratch tests. A physical therapist is ideally involved in SCI pain assessment to determine biomechanical origins of pain, such as gait, postural, or seating abnormalities.
Self-report measures
Pain assessment should always include reliable and valid self-report measures that reflect the biopsychosocial nature of pain. Self-report measures compliment information derived from interview and supply essential data for evaluating the course of pain over time and response to treatment. The numerical rating scale (NRS; 0-10) of pain intensity is by far the most commonly used measure of pain. A number of studies have established the NRS as a reliable and valid measure of pain intensity. Moreover, NRS pain intensity scores may be classified into mild, moderate, and severe categories . Beyond pain intensity it is important for assessment to capture the multidimensional nature of pain in terms of interference with daily activities. Specifically, the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials group (IMMPACT; ) recommended that measures of pain severity, physical functioning, and emotional functioning be included in all clinical trials of chronic pain interventions. The impact of pain on physical functioning may be captured by pain interference measures: the Graded Chronic Pain Disability scale , the Brief Pain Inventory , and the Multidimensional Pain Inventory (MPI; ) have all shown adequate reliability and validity in SCI populations . The impact of pain on emotional functioning may be assessed by a measure of depressive symptoms such as the Beck Depression Inventory (BDI; ) or a broader measure of mood disturbance such as the Profile of Mood states . The Patient Health Questionnaire may be an especially useful tool, because it produces a score reflecting depression symptom severity based on questions matching the nine diagnostic criteria that make up the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV; ) criteria for major depression. Furthermore, the Patient Health Questionnaire (PHQ-9) has support for its validity in the SCI population .
Psychological assessment
Self-report measures of pain experiences should be accompanied by a clinical interview and additional testing that systematically evaluates psychological concomitants of pain. An interview should address mental health history, substance use/misuse history, and aspects of psychosocial history not previously pursued by other team members. Similarly, current mental health concerns and treatments, psychiatric diagnoses, drug and alcohol use patterns, and psychosocial stressors should all be appraised. The Minnesota Multiphasic Personality Inventory (MMPI; ) has been used for standardized assessment of longstanding patterns of affect, thought, and behavior among persons with SCI . Neuropsychological testing may be indicated to explore questions of cognitive functioning, particularly in the presence of high injury levels or other risk factors for brain injury.
Psychological aspects of spinal cord injury pain
Absent from most classification systems is the concept of a pain type that is purely psychological in origin. Rather, psychological factors such as mood, thoughts, and social interactions may be considered to have a bidirectional relationship with all types of pain, with particularly important roles in the development of chronic pain and pain-related functional disability . As noted earlier in this chapter, most if not all persons with SCI endure pain on a daily basis for years, and yet only a minority experience clinically meaningful pain-related functional disability. Understanding the differential impact of pain on functioning across individuals is an important goal for research, with direct bearing on allocation of health care resources and the design of more effective interventions. With this aim in mind, numerous investigators have examined what demographic, medical, or SCI-related factors might predict variability in the functional impact of pain. Consistent predictors of pain-related disability have not emerged from these studies, as noted in past reviews that span decades of research . One explanation for the inconsistent findings relates to methodologic problems across studies, such as small sample sizes, cross-sectional designs, and variability in how pain-related disability is defined and measured. Alternatively, consistent findings may be elusive if variability in pain-related disability is largely accounted for by psychological factors. For example, a well-replicated finding in both cross-sectional and longitudinal studies is that psychological factors, such as mood or cognitions, are better predictors of pain interference than injury-related factors such as level, completeness, or etiology of injury .
These findings have stimulated research and theorizing regarding explanatory models of psychological factors and pain-related disability. Prominent in this research have been theories emphasizing the role of maladaptive cognitive processes, such as catastrophizing, in the development and maintenance of functional disability related to pain. Catastrophizing refers to exaggerated negative expectations or interpretations of an experience, such as pain . The degree to which one catastrophizes (“I cannot stand this pain! It will never get better!”) is thought to be associated with the impact of pain on outcomes such as functioning and well-being. Strong associations between catastrophizing and functioning have been observed across diverse patient groups while controlling for possible confounds such as pain severity, illness severity, or personality . Consistent with research among other populations, catastrophizing has been shown to be a potent predictor of pain-related functional disability among persons with SCI . Catastrophizing is thought to play a mediating role between pain and functioning in most models. For example, painful stimuli may serve to activate “pain schemas,” or memory stores of knowledge related to pain, that support cognitive-processing biases such as catastrophizing . Biases in cognitive processing may involve enhanced memory for, or attention toward, negatively valenced illness-related information . The effect of cognitive processing biases such as catastrophizing may be to heighten the threat value of pain and highlight inadequacies in personal coping resources, with ultimate impact on activity levels and function ( Fig. 1 ; ).
The impact of pain on psychological adjustment is also important to describe. Cross-sectional, correlational studies consistently show associations between pain and various indicators of psychosocial adjustment after SCI . While this evidence supports causal hypotheses regarding the effect of pain on psychosocial adjustment of persons with SCI, it may be just as likely that psychosocial adjustment is influencing pain. However, prospective studies suggest that pain may precede conditions reflective of psychosocial maladjustment, such as clinical depression .
Assessment of spinal cord injury pain
Medical assessment
Pain assessment procedures that have been detailed elsewhere are reviewed here. Assessment of pain in persons with SCI should begin with classification of the pain according to mechanism to suggest the most appropriate first-line treatment strategies. Most classification systems rely on neurologic level determined by examination and verbal descriptions of pain locations (eg, above, at, or below level) and pain qualities (eg, burning, aching, stabbing). Thus, neurologic examination and a detailed pain interview are arguably the central aspects of SCI pain assessment. However, medical examination should also include general physical, musculoskeletal, laboratory (radiologic, electrophysiologic) and mental status testing. Information should be gathered regarding a patient’s family, psychosocial, and medical histories. A pain history should be taken to understand the characteristics of the pain at onset, circumstances surrounding onset, past treatments, and the course of pain to the present date. The interview should elicit a detailed pain description by the patient, in terms of pain location, distribution, quality, intensity, periodicity, and duration. Factors aggravating or relieving pain should be noted, eg, movement, pressure, heat-cold, or stress. Pain description is accompanied by physical examination of the pain through inspection and palpation of the painful region. Physical examination should also assess for allodynia, hyperalgesia, or hyperesthesia in painful regions using appropriate brush, pinch, pin-prick, or scratch tests. A physical therapist is ideally involved in SCI pain assessment to determine biomechanical origins of pain, such as gait, postural, or seating abnormalities.
Self-report measures
Pain assessment should always include reliable and valid self-report measures that reflect the biopsychosocial nature of pain. Self-report measures compliment information derived from interview and supply essential data for evaluating the course of pain over time and response to treatment. The numerical rating scale (NRS; 0-10) of pain intensity is by far the most commonly used measure of pain. A number of studies have established the NRS as a reliable and valid measure of pain intensity. Moreover, NRS pain intensity scores may be classified into mild, moderate, and severe categories . Beyond pain intensity it is important for assessment to capture the multidimensional nature of pain in terms of interference with daily activities. Specifically, the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials group (IMMPACT; ) recommended that measures of pain severity, physical functioning, and emotional functioning be included in all clinical trials of chronic pain interventions. The impact of pain on physical functioning may be captured by pain interference measures: the Graded Chronic Pain Disability scale , the Brief Pain Inventory , and the Multidimensional Pain Inventory (MPI; ) have all shown adequate reliability and validity in SCI populations . The impact of pain on emotional functioning may be assessed by a measure of depressive symptoms such as the Beck Depression Inventory (BDI; ) or a broader measure of mood disturbance such as the Profile of Mood states . The Patient Health Questionnaire may be an especially useful tool, because it produces a score reflecting depression symptom severity based on questions matching the nine diagnostic criteria that make up the Diagnostic and Statistical Manual of Mental Disorders, 4th Edition (DSM-IV; ) criteria for major depression. Furthermore, the Patient Health Questionnaire (PHQ-9) has support for its validity in the SCI population .
Psychological assessment
Self-report measures of pain experiences should be accompanied by a clinical interview and additional testing that systematically evaluates psychological concomitants of pain. An interview should address mental health history, substance use/misuse history, and aspects of psychosocial history not previously pursued by other team members. Similarly, current mental health concerns and treatments, psychiatric diagnoses, drug and alcohol use patterns, and psychosocial stressors should all be appraised. The Minnesota Multiphasic Personality Inventory (MMPI; ) has been used for standardized assessment of longstanding patterns of affect, thought, and behavior among persons with SCI . Neuropsychological testing may be indicated to explore questions of cognitive functioning, particularly in the presence of high injury levels or other risk factors for brain injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





