2.1.1.3 Fracture Classification
Allman, in 1967, classified clavicle fractures into three groups based upon anatomical location. Groups I and III were further subdivided by Craig and Neer but the initial anatomical classification is sufficient for describing paediatric fractures.
Group I – middle third (most common) (Fig. 2.1).

Figure 2.1
Plain radiograph of clavicle fracture, showing a middle third fracture
Group II – lateral third (distal to coracoclavicular ligaments).
Group III – proximal (medial) third.
2.1.1.4 Treatment and Indications for Surgery
The majority of clavicle fractures can be treated conservatively in a sling for 2–4 weeks, depending on the child’s age, followed by mobilization.
Indications for surgery include:
Open fractures.
Tenting of overlying skin which threatens soft tissue envelope.
Plexus or vessel impingement, clinically or on imaging.
Open surgery aims to reduce the fracture fragments back into their periosteal sleeve with repair of the ruptured periosteum. This will usually result in a stable reduction and fixation is rarely required.
Medial sternoclavicular joint dislocation or a displaced Salter Harris (SH) I or II fracture should be assessed on CT and undergo closed reduction under general anaesthetic. Unstable reductions can be augmented by open capsular repair.
2.1.1.5 Follow-Up
Fracture clinic review can be carried out at 1 week and 4 weeks post-injury with clinical assessment and mobilization as the shoulder becomes more comfortable. Repeat X-rays are often not required.
Some institutions still use figure of eight bandages to encourage return to full length and alignment as the fracture callus matures. If this is the case, then the child should be reviewed weekly to ensure that no compression complications are developing as result of the bandage position.
2.1.1.6 Complications
Neurovascular compromise.
Mal-union.
Non-union (this is rare and has never been documented in a child under the age of 12 years).
Pulmonary injury.
2.1.1.7 Synopsis
Common childhood fractures with a long tradition of successful conservative treatment with sling immobilization.
Care should be taken with medial injuries as there is a recognized risk of compression of associated structures and therefore more often require reduction in theatre.
2.1.2 Acromio-Clavicular & Sterno-Clavicular Dislocations
Acromio-clavicular (AC) joint disruptions are rare, and when present occur in children over the age of 13. It is important to differentiate between a true AC joint disruption and a fracture. The distal clavicle physis does not ossify till adolescence and so SH I type injuries may be commonly mistaken for AC joint disruptions. They are treated much the same as adults.
Sterno-clavicular (SC) joint disruption is rarer than AC disruptions and similar diagnostic difficulties arise as the ossification centre at the medial end does not appear until about 16, fusing at around 25 (Fig. 2.2).
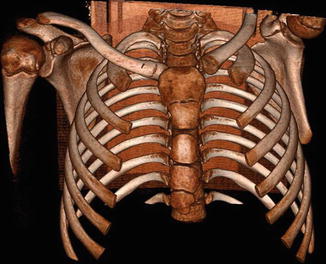
Figure 2.2
CT reconstructions in 3D showing a sternoclavicular dislocation
2.1.3 Proximal Humerus Fractures
2.1.3.1 Epidemiology
These relatively uncommon injuries occur with an incidence of 1–2 in 1000 and account for approximately 5% of paediatric fractures. They occur most commonly in the adolescent involved in sporting activity through a direct or indirect blow and can involve the after metaphysis (Fig. 2.3), physis or both. The metaphysis is the most commonly affected area in 5–12 year olds due to the rapid growth in this area and the structural weakness in this growing bone. Birth injuries of the proximal humerus are physeal fractures and are often misdiagnosed as glenohumeral dislocations. Ultrasound is useful to confirm a located glenohumeral joint and no fracture treatment is required beyond bandage for analgesia.


Figure 2.3
Proximal humerus fracture
2.1.3.2 Diagnosis
The older child will present with a consistent traumatic history and the arm held in internal rotation to offload the deforming force of pectoralis major on the distal fragment. Range of movement will be limited by pain. Associated injuries including glenohumeral dislocation and neurological injury should be sought. They can be ruled out with a full set of anteroposterior, lateral or Y view and axial X-ray views and detailed neurological examination.
2.1.3.3 Fracture Classification
Proximal epiphyseal humeral fractures were classified by Neer and Horowiz in 1965 and describe the extent of fracture displacement:
Grade I – up to 5 mm displacement.
Grade II – up to one third displacement.
Grade III – up to two thirds displacement.
Grade IV – greater than two thirds displacement.
2.1.3.4 Treatment and Indications for Surgery
Eighty percent of humeral growth occurs at the proximal humerus. This results in massive potential for remodeling. Combined with a large range of movement at the glenohumeral joint, good outcomes can be expected for what may appear to be significant displacement or angulation.
Acceptable displacement:
Age 1 to 4 – 70° of angulation and any amount of displacement.
Age 5 to 12 – 40–45° of angulation and up to 50% of metaphyseal width translation.
Age >12 – 15–20° of angulation and translation of up to one third of metaphyseal width.
Closed reduction under anaesthetic in theatre is indicated for displacements beyond these ranges.
Indications for surgery include:
Open fractures.
Associated neurovascular compromise.
Salter Harris III or IV fractures with displacement.
Irreducible fracture dislocations.
Displaced lesser tuberosity fractures.
Fixation in unstable fractures is maintained with percutaneous smooth Kirschner wires for epiphyseal and high metaphyseal fractures and intramedullary rods for more distal fractures.
2.1.3.5 Follow-Up
In patients up to the age of 5 years, a sling can be used for 5–7 days followed by review in fracture clinic and mobilization. In the over 5 s, the sling can be maintained for 2–3 weeks followed by fracture clinic review and mobilization.
Reduced range of movement associated with stiffness or deformity in the paediatric patient will resolve with time and remodelling in the vast majority of cases. If there is functional deficiency at the 4–6 week review, then further review at 3–6 months for repeat examination will often reveal resolution of their symptoms.
2.1.3.6 Complications
Proximal humeral varus.
Limb length inequality.
Loss of motion.
Inferior glenohumeral subluxation.
Osteonecrosis.
Nerve injury.
Growth arrest.
2.1.3.7 Synopsis
Neer Grade I and II injuries almost invariably do well with conservative measures due to their remodeling potential.
Grade III and IV injuries may have some residual angulation or shortening but even these are well tolerated.
2.2 Fractures Around the Elbow
2.2.1 Supracondylar Fractures
2.2.1.1 Epidemiology
Supracondylar fractures account for 60% of all elbow fractures and 30% of all paediatric extremity fractures. The peak age of occurrence is 5–7 years with a male to female ratio of 3:2. Nerve injury occurs in 7% and vascular injury in 1%. Ninety percent are extension type fracture pattern.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








