Figure 3.1
Plain radiograph of olecranon fracture
3.1.3.2 Treatment and Indications for Surgery
The majority (80%) of fractures are undisplaced and can be managed with a plaster cast alone. The elbow should be immobilised for a period of 3–6 weeks, depending on the age of the child.
Indications for surgery:
Open fracture.
Fracture displacement with loss of active elbow extension.
Open reduction aims to reduce any articular surface incongruency, and reduction is held with longitudinal Kirschner wires with a supporting figure-of-eight tension band suture as required.
3.1.3.3 Follow-Up
Following operative reduction and fixation, the elbow should be protected in a cast for 4–6 weeks with encouragement of wrist and hand mobilization. Longitudinal K-wires are removed at 8–10 weeks.
3.1.3.4 Complications
Delayed union.
Nerve injury.
Elongation / spur formation resulting in limits to extension.
Loss of reduction in conservatively managed cases.
3.1.4 Radial Head and Neck Fractures
3.1.4.1 Fracture Classification
Proximal radius fractures in children more commonly affect the neck rather than the head. When the physis is involved it is most commonly a Salter Harris Type II fracture. Neck fractures are classified according to the angular deformity and displacement by Metaizeau:
Grade 1 – 0° angulation with translation.
Grade 2 – less than 30° angulation.
Grade 3 – 30 to 60° angulation.
Grade 4a – 60 to 80° angulation.
Grade 4b – greater than 80° angulation (Fig. 3.2).

Figure 3.2
Plain radiograph of radial neck fracture
3.1.4.2 Treatment and Indications for Surgery
Many radial neck fractures are undisplaced and can be managed conservatively. Up to 30° of angulation at the radial neck is acceptable (Grade 1–2). Early mobilisation with a collar and cuff sling for comfort should be encouraged. The sling can generally be discontinued after a period of 2–3 weeks, as comfort allows. A return to normal function can be anticipated although full elbow extension may take a month or two to recover.
Indications for Surgery:
More than 30° of angulation at the radial neck (Grade 3–4).
Stable closed reduction can be treated in a collar and cuff in a similar way to minimally displaced fractures. Open reduction should be avoided where possible, using a K-wire to joystick the head fragment back into place or a retrograde elastic nail or Ilizarov wire to flip the fragment back into position.
3.1.4.3 Follow-Up
If percutaneous wires are left in situ, then the elbow will require protection in a cast for 4 weeks before removal of the wire. If a retrograde IM rod has been used, then the mobilization can be initiated immediately and the rod removed at 2–3 months after the initial surgery.
3.1.4.4 Complications
Decreased range of movement (pronation > supination > extension > flexion).
Radial head overgrowth.
Premature physeal closure.
Radial head osteonecrosis.
Neurological injury (particularly the posterior interosseous nerve).
Radioulnar synostosis.
Myositis ossificans.
3.1.4.5 Synopsis
Surgical intervention is determined by extent of displacement.
Up to a quarter of patients will have a poor result regardless of treatment, complaining of reduced range of movement.
Younger patients with less initial displacement and early, closed treatment, will tend to do better.
3.1.5 Monteggia Type Injuries
3.1.5.1 Fracture Classification
Combined proximal ulnar fracture and radial head dislocation is well recognised in the paediatric population and after any forearm or elbow injury, the position of the radial head in relation to the capitellum must be determined on radiographs.
The most common classification of the Monteggia lesion is the one proposed by Bado in 1962:
Type I – anterior dislocation of radial head (70%).
Type II – posterior dislocation of radial head (6%).
Type III – lateral dislocation of radial head (23%).
Type IV – dislocation of the radial head with radial neck fracture (1%) (Fig. 3.3).

Figure 3.3
Bado type I and III Monteggia fracture
3.1.5.2 Treatment and Indications for Surgery
By definition, a Monteggia fracture has an associated radial head dislocation and therefore (after exclusion of a congenital or chronic dislocation) all Monteggia fractures require surgery to re-align the ulna and reduce the dislocation.
Closed reduction of the angulated ulnar fracture will enable stable reduction of the dislocated radial head in almost all acute Monteggia fractures. If the radial head is irreducible, then it will require open exploration to dislodge and repair an obstructing annular ligament.
Radial head instability following successful reduction will be due to recurrent angulation at the ulnar fracture site and requires stabilisation of the fracture with plating, K-wires or intramedullary rods/wires.
3.1.5.3 Follow-Up
The elbow is protected in a cast for 4–6 weeks followed by mobilisation. Wires can be removed in clinic at 4 weeks and plates or rods removed as a day case at 2–3 months.
3.1.5.4 Complications
Nerve inury (radial nerve 10–20% in Types I and III).
Myositis ossificans.
3.1.5.5 Synopsis
Associated radial head dislocation should always be ruled out with an intact radiocapitellar line on AP and lateral films in any ulnar fracture.
3.1.6 Radial and Ulnar Shaft Fractures
3.1.6.1 Fracture Classification
Fractures of the radius and ulna are generally classified by the position of the fracture – proximal, mid or distal third (Fig. 3.4). The use of general fracture classifications such as system proposed by the AO Foundation is an alternative.
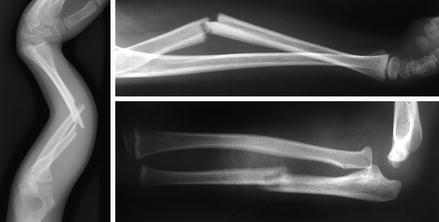
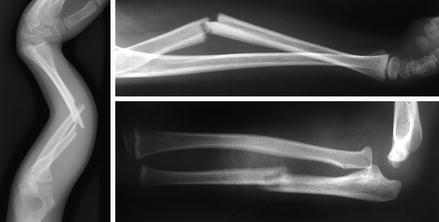
Figure 3.4
Plain radiographs of a both bone forearm fracture, an isolated radial fracture and an isolated ulna fracture
3.1.6.2 Treatment and Indications for Surgery
Acceptable deformity:
Angular deformity – 10° correction per year with degree of acceptable angulation being inversely proportional to distance from the physis.
Bayonet apposition – up to 1 cm in children <10 years old.
Rotational deformity and deformity in patients >10 years old should not be accepted.
Closed reduction in a well molded above elbow cast with the forearm in a fracture appropriate orientation provides symptomatic control and allows for a significant improvement in fracture position. The child’s age, compliance and injury extent will determine the need for general anaesthesia, sedation or gas and air with analgesia.
Indications for open surgery:
Unstable/unacceptable fracture reduction after closed reduction.
Open fracture/compartment syndrome.
Floating elbow.
Refracture with displacement.
Segmental fracture.
Age (girls >14 years old, boys >15 years old).
Routine operative/open reduction and fixation is with flexible intramedullary nails (elastic nails). These provide effective reduction control while reducing the extent of open dissection, rate of neurovascular injuries, length of surgery and complications associated with future metalwork removal. Indications for plate osteosynthesis include significant comminution or an unstable fracture configuration with potential for shortening.
3.1.6.3 Follow-Up
After a closed reduction or after an open reduction and plate osteosynthesis, an above elbow cast should be maintained for 4–6 weeks. With the cast on, finger movements should be encouraged. At 4 weeks and with radiological signs of union, it may be possible to convert to a short, below elbow cast for the final 2 weeks. After stabilisation, a cast is not strictly required as the fractures are well stabilised but in practice, a short below elbow cast for 2 weeks is used to provide some pain relief. With a short cast, elbow and finger movements should be encouraged. Plates and elastic nails should be removed once the fractures have solidly united and typically this is after 4–6 months. If at the time of the initial operation the end of the elastic nail has not been buried, then it will need to be removed earlier at about 6 weeks and some additional protection may be required.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








