Osteotomy of the Proximal Phalanx of the Hallux (Akin Procedure)
G. Andrew Murphy
David R. Richardson
The Akin procedure is a medial closing wedge osteotomy of the proximal phalanx originally for the correction of hallux valgus. Described by Akin in 1925 (1), the procedure involves a closing wedge resection of the proximal phalanx combined with removal of the medial eminence and the medial base of the proximal phalanx. Since Akin’s original description, a number of modifications to the procedure have been described (2, 3, 4, 5 and 6). It has been combined with various other osteotomies such as distal chevron osteotomy, proximal closing wedge osteotomy, scarf osteotomy, and proximal metatarsal osteotomy with cuneiform osteotomy. It is less commonly performed as the primary operation for correction of hallux valgus deformity (2,7,8).
INDICATIONS AND CONTRAINDICATIONS
As an isolated primary procedure, the Akin procedure is indicated for:
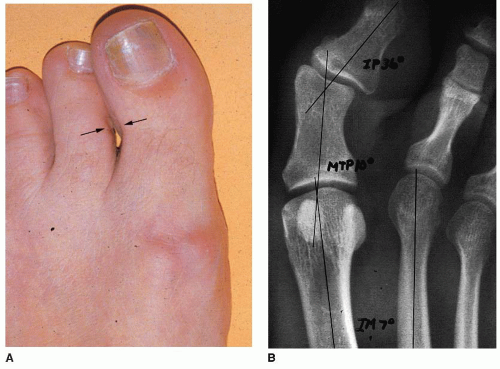
Hallux valgus interphalangeus (Fig. 3.1)
Additional valgus correction after joint realignment procedures (Fig. 3.2)
Relief of second toe contact with limited hallux valgus deformity (hallux valgus angle [HVA] ≤25°, intermetatarsal angle [IMA] ≤13° or second toe varus)
Recurrent or residual hallux valgus after correction (see Fig. 3.2)
Secondary procedure to extend the indications for other osteotomies (e.g., elevated distal metatarsal articular angle [DMAA] with a congruent joint) (Fig. 3.3) Akin procedure is contraindicated in patients with
Infection
Neuropathy, unless used to treat or prevent second to ulceration
Peripheral vascular disease sufficient to impair healing
Open physis of the proximal phalanx (skeletally immature patients)
Metatarsophalangeal (MTP) arthritis with valgus (as primary treatment) The procedure also should be used with caution in a patient with incongruent hallux valgus, a round metatarsal head, and an unstable MTP joint because of the risk of progression or recurrence of the deformity.
PREOPERATIVE PLANNING
An integral part of preoperative preparation is a thorough physical examination and radiographic evaluation of the deformity.
 FIGURE 3.2 Patient with recurrent or residual hallux valgus. A and B: Preoperative photo and radiograph. |
With the patient standing, the clinician should assess
Valgus deformity (MTP joint and interphalangeal [IP] joint)
Size of the medial eminence
Height of the arch
Impingement on the second toe (see Fig. 3.1)
Presence of dorsal osteophytes
Relative lengths of the hallux and second toe
Nail deformity
With the patient sitting, the clinician should evaluate
Range of motion of the MTP joint with the ankle flexed and at neutral
Dynamic pronation of the toe with passive extension, which may indicate intrinsic malalignment
Flexibility of the MTP, IP, and first tarsometatarsal (TMT) joints
Whether the valgus deformity is passively correctable.
Interdigital corns
Neurovascular status of the foot and leg
Radiographic evaluation should include standing anteroposterior, lateral, oblique, and sesamoid views to evaluate
Joint congruency
Joint arthrosis
Distal metatarsal articular angle (Fig. 3.4)
Hallux valgus angle
Intermetatarsal 1-2 angle
IP joint angle
Phalangeal articular angle
Sesamoid incongruency (Fig. 3.5)
 FIGURE 3.4 Patient with hallux valgus with elevated DMAA (same patient as in Fig. 3.2). A: Preoperative anteroposterior (AP) radiograph shows laterally facing distal metatarsal articular surface. B: Intraoperative photo shows laterally facing distal metatarsal articular surface. |
Technical aspects of the procedure to be considered before surgery include determining the location of the osteotomy: base, midthird, or distal. In patients with hallux valgus interphalangeus with a high phalangeal articular angle and deformity through the phalangeal neck, the osteotomy could be made in the distal third of the phalanx, in the phalangeal neck. Osteotomy at the base of the phalanx will increase the hallux valgus correction obtained with other primary procedures in patients with an elevated DMAA or second toe impingement (see Fig. 3.4




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree