Osteosynthesis for Nonunion of the Distal Humerus
Joaquin Sanchez-Sotelo
INTRODUCTION
In spite of improved techniques and implants for treating the acute fracture, we continue to see the ununited distal humeral fracture. These patients pose some of the most challenging surgical obstacles to the surgeon. There is relatively little discussion of the problem in the literature with most information coming from Mayo (1,2 and 3) and Massachusetts General Hospital (4,5).
INDICATIONS/CONTRAINDICATIONS
Indications
Painful nonunion
Loss of functional motion
Patient with salvageable articulation
Contraindications
Destroyed articulation
Active or subacute sepsis
Severe osteoporosis
Elderly, inactive patient
Note: Elbow replacement is an excellent option for the patient with the above-described features (see Chapter 37).
PREOPERATIVE PLANNING
The Patient: This is a salvage procedure. The patient must be clear that this surgery has a high complication rate. Furthermore, replacement must be offered as an alternative in the older patient.
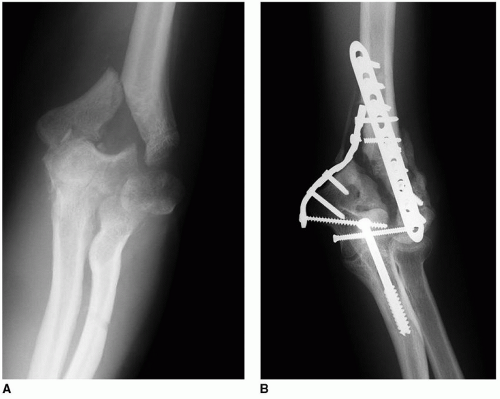
The Fracture: There are two basic kinds of distal humeral nonunion. The most simple is that of an intact articular surface as with a supracondylar nonunion. The next most complicated one is one in which the trochlea is intact with a large fragment to allow rigid fixation. The most difficult is the patient with a distorted articulation and fragment resorption (Fig. 10-1).
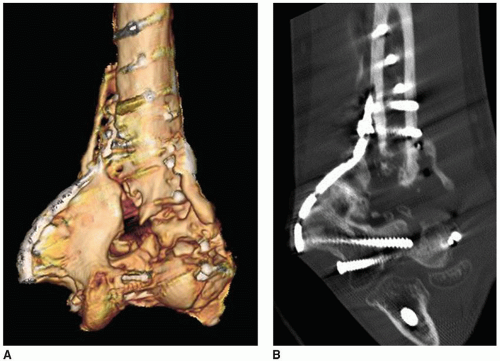
Imaging: For the nonunion patient, a CT scan and reconstruction are very helpful. This is especially so in those in whom the nonunion involves the articular surface (Fig. 10-2).
Implants: Be sure precontoured plates are available, as these are especially helpful to serve as a template for proper fragment orientation.
Bone Graft: Both cancellous and structural allografts should be available (author’s preference). Alternatively, autograft donor sites must be considered and prepped if these will potentially be used.
SURGICAL TECHNIQUE
The patient is placed with the arm brought across the chest. Alternatively, if the surgeon is familiar with treating acute fractures in the lateral decubitus position, the position most familiar to the surgeon for acute fractures could be employed for the management of nonunion.
Surgical Incision
In virtually every instance, there will be a previous incision almost always posteriorly. It should be reentered. If the original incision is displaced medially or more commonly laterally, then a more posterior incision is placed as widely as possible from the earlier incision. If a second incision is performed, ideally, the prior incision should be several years old.
Ulnar Nerve
The dissection initially carries through the subcutaneous tissue to the triceps fascia. The medial flap is elevated, and the ulnar nerve is identified proximally at the medial aspect of the triceps. Careful preoperative assessment should determine whether or not the nerve has been translocated and whether or not symptoms are present. If symptomatic, the nerve should be decompressed. If the nerve is asymptomatic, it is sufficient to identify the location of the nerve without formally exposing it unless it is in the surgical field.
Exposure of the Articulation
Triceps Sparing In nonunions that have large, more proximal fragments, a triceps-sparing approach might be considered, especially if the articulation is well healed. The triceps is elevated from the posterior humerus, and the medial and lateral columns are further exposed. The articular fragment must be accurately positioned on the distal humerus. Distortion is usually present, so the accuracy of this step should be checked by intraoperative imaging. The distal humerus and articular fragment are carefully prepared to assure the accuracy of the relationship of the two fragments.
Olecranon Osteotomy




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree