Chapter 20 Osteoporosis
KEY POINTS
 Only 25% of people suffering a hip fracture regain their previous level of independence and up to 20% die within 6 months.
Only 25% of people suffering a hip fracture regain their previous level of independence and up to 20% die within 6 months.INTRODUCTION
Osteoporosis is a condition in which gradually decreasing bone mass and deteriorating bone structure leads to increased bone fragility and increased risk for fractures, particularly of the wrist, hip and spine (WHO 1994). This process progresses without symptoms until fractures occur or kyphosis becomes apparent. Thus osteoporosis is often described as a silent menace.
Once fractures and deformities have occurred, pain may become a prominent problem and a challenge for people with osteoporosis and everyone involved with their care. Such established osteoporosis is a major cause of morbidity, mortality and reduced quality of life (Lips et al 2005).
INCIDENCE
Osteoporosis affects one in three women and one in twelve men over the age of 50 years (Barlow 1994). The incidence of osteoporotic fractures rises with increasing age. In particular, the incidence of hip fractures rises sharply beyond the age of 65 years in both men and women (Cooper & Melton 1992). Of people surviving to 80 years of age, one in three women and one in five men will suffer a hip fracture. Each year in the UK there are about 60,000 hip fractures, 50,000 wrist fractures and 40,000 clinically diagnosed vertebral fractures (Compston et al 1995, Donaldson et al 1990). The annual NHS cost for managing these is estimated to be in excess of £2.1 billion pounds per year (Cooper 1993). As only 25% of people suffering a hip fracture regain their previous level of independence and up to 20% die within six months, the cost to society is much greater (Jensen & Tondevold 1979).
Interventions to reduce fracture risk have been shown to be clinically and cost effective and should be implemented for those at greatest risk. Women are as likely to suffer an osteoporotic fracture in their lifetime as they are coronary heart disease and the cost effectiveness for interventions are similar for both diseases (Johnell et al 2005).
AETIOLOGY
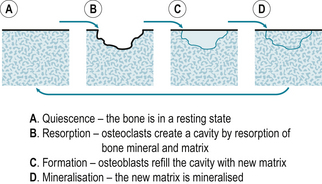
Bone undergoes a repetitive cycle of remodelling. Osteoclasts break down the bone (resorption) and osteoblasts rebuild it (formation) (Fig. 20.1). Throughout childhood bone formation exceeds resorption and bone mass increases. Peak bone mass is achieved by the age of 20 to 30 years and plateaus for approximately 10 years before declining gradually by about 1% per year. During the menopause the rate of bone loss is greater as bone resorption exceeds formation.
Adult bone mass may be lower than average due to impaired acquisition during childhood or a greater than average rate of bone loss later in life. Impaired peak bone mass acquisition accounts for approximately two thirds of the variance in bone mass seen at any age. Genetic factors have the greatest influence on this (Nguyen et al 2003). Suppressed oestrogen, testosterone or growth hormone production and environmental factors such as poor dietary calcium intake and lack of exercise also delay or diminish bone mass acquisition during childhood and adolescence.
Beyond the age of 40 years, hormonal and environmental factors, rather than genetic factors, have the greatest impact on the rate of bone loss (Seeman 2002). A combination of oestrogen deprivation, calcium and vitamin D deficiency and secondary hyperparathyroidism account for the rapid loss seen in postmenopausal women (Cummings et al 1995). Many other epidemiological factors have been identified (Box 20.1). However, the impact of each factor, or combinations of factors, on an individual requires further clarification.
DIAGNOSIS
As osteoporosis causes no symptoms until fractures or kyphosis occur, it may remain undiagnosed for many years. Whilst the strongest predictive factors for sustaining osteoporotic fractures are a previous fracture and a low bone mass measurement (Bouxesin 2003, Cummings et al 1995), diagnosis may predate fractures if individuals and health care professionals routinely consider the risks for osteoporosis, fractures and falls. A variety of tools, such as paper or electronic questionnaires, are available to facilitate the identification of patients at risk (Kanis et al 2002, Kanis & Gluer 2000).
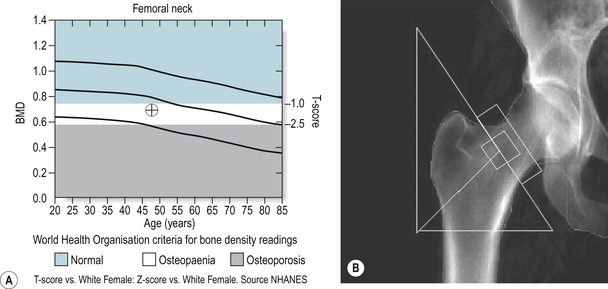
The gold standard method for diagnosis is to measure bone mass, or bone mineral density (BMD), using dual energy x-ray absorptiometry (DEXA). DEXA scans are quick, comfortable and relatively cheap to perform and involve minimal radiation exposure (equivalent to about a days background radiation) (Fig. 20.2). DEXA results correlate strongly with fracture risk (Kanis & Gluer 2000) but other bone qualities such as elasticity and architecture, not measurable with DEXA, also contribute.
Bone density readings of the hip and spine are given as the number of standard deviations below the mean peak bone mass of a 20 to 30 year old woman (T-score), the standard deviations below the age matched mean (Z-score) (Fig. 20.3A,B) and as a reading of g/cm2. A woman has normal bone density if her T-score is no lower than 1 standard deviation below the young adult mean (T-score higher than –1). Osteopaenia (mild thinning of the bones) is present if density lies between 1 to 2.5 standard deviations below the young adult mean. Readings representing osteoporosis are more than 2.5 standard deviations below the young adult mean (T-score below –2.5) and established osteoporosis is present if at least one fragility fracture has occurred at this low level (WHO 1994). If the Z-score is low, bone density is lower than expected for the patient’s age and other risk factors or underlying disease must be considered. The same criteria are used for men but further work is required to determine the relationship between these scores and fracture risk.
DIFFERENTIAL DIAGNOSIS
Low bone density can be assumed to be due to osteoporosis only if other causes have been excluded (Box 20.2). For this reason screening blood tests for metabolic, endocrine and malignant disease are often performed in patients with low bone density. Typically, these tests include full blood count, erythrocyte sedimentation rate (ESR), urea and electrolytes, liver function, bone biochemistry, thyroid function, testosterone and gonadotrophins (in men) and perhaps parathyroid hormone and vitamin D levels (depending on the history and other findings). Serum immunoglobulins and electrophoresis and urinary Bence-Jones proteins should be measured if myeloma is suspected.
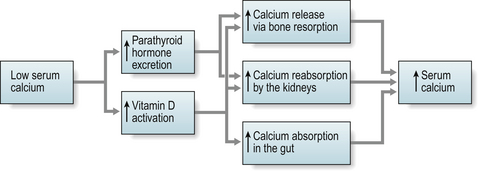
Calcium and vitamin D deficiency can occur in specific populations e.g. those from the Indian sub continent including teenage girls, and is common amongst older people, particularly those in long-term nursing or residential care. This is often due to poor dietary intake, lack of adequate sunlight exposure, reduced intestinal absorption or renal impairment and leads to impaired mineralisation of bone, known as osteomalacia. The bones become soft, prone to fracture and appear less dense on DEXA. Blood tests may show low/normal calcium, high/normal alkaline phosphatase, low phosphate, and a high parathyroid hormone level (secondary hyperparathyroidism) (Fig. 20.4).
An elevated serum corrected calcium level should raise suspicion of underlying malignancy (primary or metastatic), myeloma or primary hyperparathyroidism due to a parathyroid adenoma.
CLINICAL PRESENTATION
Patients may express concern that they have osteoporosis because they have heard or read about it, entered the menopause early (before 42 years), taken steroid therapy or have a family history of osteoporosis or fractures. The incidental finding of radiological osteopaenia, meaning a fainter appearance of the bones on a plain x-ray, also raises suspicion, but does not confirm the presence of osteoporosis. However patients mostly present with a low trauma fracture (e.g. fall from own body height), sudden severe back pain from a vertebral fracture, or the development of kyphosis and loss of height due to asymptomatic vertebral fractures. Only about a third of vertebral fractures come to medical attention (Gallacher et al 2000, Gehlbach et al 2000).
The vast majority of patients who present with their first or subsequent low trauma fractures are not assessed for osteoporosis (RCP 2007). Years later, women who have sustained wrist fractures go on to suffer hip fractures which are associated with high morbidity and mortality rates. Patients with severe osteoporosis may also suffer vertebral, pelvic or rib fractures spontaneously or from minimal trauma such as coughing or rolling over in bed.
CLINICAL EVALUATION
HISTORY
A detailed medical history is essential to assess a patient’s risks for osteoporosis (Box 20.1), falls and fractures and to consider the possibility of underlying metabolic bone disease or malignancy (Box 20.2). Patients at greatest risk for suffering an osteoporotic fracture are those who have already fractured and those with known low bone mass. For instance, the relative risk for sustaining a new vertebral fracture is more than doubled for a patient with a previous vertebral fracture and quadrupled if the patient also has low bone density. A woman who has just sustained a vertebral fracture has a one in five chance of sustaining another within one year (Lindsay et al 2001).
Fracture liaison services have been shown to improve identification of high-risk patients (McClellan et al 2003). Without these services in place, less than 10% of high-risk patients attending fracture clinics are identified, diagnosed or treated for osteoporosis (RCP 2007). As many fractures occur following falls, patients’ risks for falls must also be assessed in detail and referrals made to physiotherapists or specialist falls clinics as appropriate. Reduction of the risk for falls among the older age group requires a comprehensive multidisciplinary falls risk evaluation and multifactorial intervention (NICE 2004).
EXAMINATION
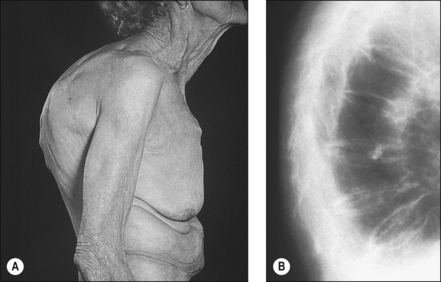
Whilst some fractures may be painfully obvious others may be detected only after careful examination and investigation. Thoracic kyphosis (Fig. 20.5A,B) may develop gradually as one vertebra after another fractures (or is compressed) or more suddenly if one or more severe wedge fractures occur. The development of the Dowager’s hump is a well recognised but late sign of osteoporosis. As this becomes more pronounced, the lower ribs impinge on the iliac crests and the abdomen protrudes. An exaggerated cervical lordosis is apparent when the patient attempts to look straight ahead. Evidence of a previous wrist fracture may also be seen such as the classical dinner fork deformity of a Colle’s fracture. A shortened externally rotated leg is highly suggestive of a fractured neck of femur.
In addition to examination of the locomotor system it is imperative that patients suspected of suffering with osteoporosis also undergo a full medical examination to elicit signs of any underlying cause for their low bone density (Box 20.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree