Osteonecrosis
John H. Healey
Andrea Piccioli
Osteonecrosis (ON) is defined as the death in situ of a segment of bone. Avascular necrosis (AVN), aseptic necrosis, and bone infarction are terms often used synonymously. All elements of the bone succumb: osteocytes, osteoblasts, osteoclasts, vascular elements, stroma, hematopoietic marrow, and fatty marrow. Deficient circulation is the typical cause. This can be spontaneous or post-traumatic.
Spontaneous ON usually affects middle-aged adults. Any bone can be affected, but the femoral head is the most frequently involved. Other common sites are the distal femur, proximal humerus, tibial plateau, and talus. It may be bilateral in as many as 25% of cases.
Secondary ON affects patients of ages commensurate with the underlying primary disease process: for example, 16 to 30 years for patients with sickle cell anemia and systemic lupus erythematosus (SLE); and 60 to 80 years for patients with osteoarthritis of the knee. It may occur in 25% of patients with osteoarthritis of the hip.
Post-traumatic cases follow site-specific fracture epidemiology. Fractures of the scaphoid, radial head, and femoral head/neck commonly cause ON.
Bone normally has a rich blood supply, but it varies widely. Certain sites such as the femoral head have an end-capillary circulation that is vulnerable to interruption. This accounts for it being the most common location for ON.
I. Three mechanisms
of circulatory compromise of bone are recognized and one or more may play a significant role in a given patient.
Mechanical disruption (e.g., traumatic fracture/dislocation or stress fracture).
Arterial (inflow) failure
Intrinsic vascular (e.g., vasculitis, radiation injury, and vasospasm).
Extrinsic (e.g., compression by fat hypertrophy or Gaucher’s cells).
Embolic (e.g., fat embolism, sickle cells, or nitrogen—“Caisson’s disease”).
Venous outflow failure (e.g., when venous pressure exceeds arterial pressure by any mechanism or by thrombosis). This mechanism may, in fact, be the final common pathway of the other two mechanisms.
II. ETIOLOGY
Idiopathic. This is most common and accounts for approximately 50% of cases.
Secondary
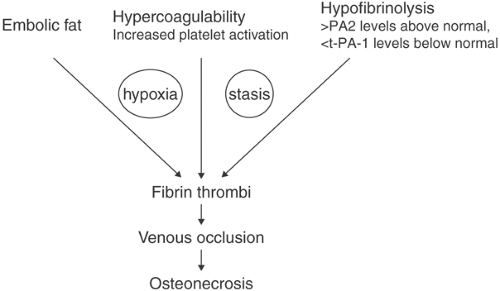
Corticosteroid. The exact cause is unclear, although fat embolism and local clotting are implicated in corticosteroid-related ON (Fig. 52-1). This is a significant cause of ON because of the use of steroids for many diseases, including SLE, rheumatoid arthritMis, inflammatory bowel disease, nephrotic syndrome, lymphoma, and other myelogenous diseases, respiratory disease,
and central nervous system disorders. In SLE, a high average daily dose (more than 16.6 mg) and pulse therapy are considered important predictors for the development of ON.
Alcohol. There is a clear dose–response relation: consumption of more than 400 mL weekly results in a tenfold greater risk for ON. Fat emboli from alcohol-induced fatty liver, increased blood cortisol levels, and altered lipid metabolism are all proposed mechanisms of ON in alcoholics.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree