Osteochondritis dissecans (OCD) of the knee is a common entity in both adults and children. Its incidence has historically been estimated to be between 0.02% and 0.03% based on knee radiographs, and 1.2% based on knee arthroscopy (
5,
11,
27). More recent investigators have reported much higher frequencies (
1,
21). Osteochondritis dissecans occurs twice as often in males as in females. Osteochondritis dissecans is most common in the medial femoral condyle, followed by the lateral femoral condyle; its occurrence in the patella is rare. It primarily affects young athletic individuals and can significantly impair knee function and activity and lead to long-term disability (
10).
The etiology of OCD is controversial and remains unclear. Theories include ischemia, repetitive microtrauma, familial predisposition, endocrine imbalance, epiphyseal abnormalities, accessory centers of ossification, growth disorders, osteochondral fracture, repetitive microtrauma with subsequent interruption of interosseous blood supply to the subchondral area of the epiphysis, anatomic variations in the knee, and congenitally abnormal subchondral bone.
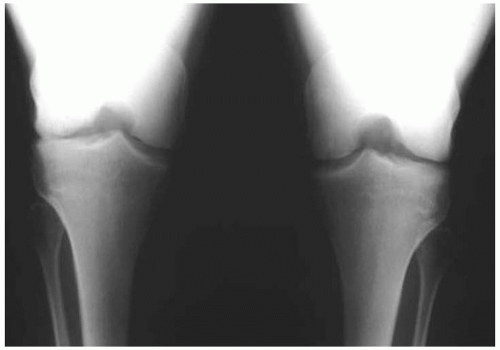
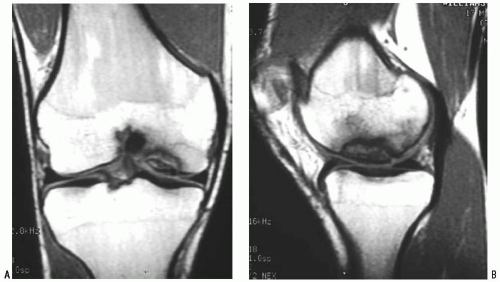
It is important to distinguish OCD from acute osteochondral fracture (
Fig. 34-1). In addition, an OCD lesion that has separated from a vascular bony bed should be distinguished from one that has separated from an avascular bony bed (osteonecrosis). Osteochondritis dissecans is more common in adolescents and young adults than is osteonecrosis.
Several classification schemes for OCD have been proposed. Bradley and Dandy (
5) developed a classification for the knee and limited the term OCD to expanding concentric lesions of the medial femoral condyle that appear during the second decade of life and progress to concave, steep-sided defects. Cahill and Berg (
6) proposed a classification scheme based on the appearance of the lesion on scintigraphy. Dipaola et al (
12) classified lesions according to their appearance on magnetic resonance imaging (MRI) and associated specific findings with the potential for fragment detachment. Guhl (
19) developed an intraoperative classification based on cartilage integrity and fragment stability noted at the time of arthroscopy.
Although the natural history of these lesions has not been conclusively defined, current evidence suggests that they persist and can lead to further cartilage degradation (
32). Primary prognostic factors, in addition to the age of the patient, include progression, size, stability, amount of subchondral bone present, and location of the lesion, especially as it relates to weight bearing. Lateral femoral condylar lesions tend to be more posterior, larger, less stable, and more fragmented than medial lesions.
Although nonoperative treatment has a limited role in patients with symptomatic osteochondral lesions, multiple forms of nonoperative treatment have been described, including periods of immobilization, activity modification, and non-weight bearing. Prolonged immobilization should be avoided because joint motion affects articular cartilage attrition. Cahill et al (
7) noted a 50% failure rate with conservative treatment in a juvenile population with OCD.
A number of operative procedures have been devised for treatment of OCD, ranging from simple debridement to autograft/allograft or chondrocyte implantation (
Table 34-1). Arthroscopy is preferable to arthrotomy; however, it may be necessary to convert an arthroscopic procedure to an arthroscopic-assisted mini arthrotomy to obtain adequate fixation of an unstable lesion.
INDICATIONS/CONTRAINDICATIONS
See
Table 34-1 for surgical treatment options and their indications.
There are few contraindications to surgical treatment of OCD. Contraindications to specific surgical techniques may include the size of the lesion, with some procedures suited for only small (<2 cm2) lesions; the activity demands of the patient (high vs. low demand), and the age of the patient (osteochondral allo- and autografts, autologous chondrocyte implantation usually not indicated in patients with open physes). The location of the lesion also may be a contraindication to a particular technique. Patient willingness to comply with postoperative weight-bearing restrictions also must be considered.