Fig. 8.1
Transchondral lesion “flap” softened cartilage being probed (a), separating flap (b), excising flap with shaver (c), and removing flap with grasper (d)
Osteochondral lesions are also classified with other various systems. Often radiographic findings are used to assess lesions. Hepple et al described their magnetic resonance imaging (MRI) staging system of talar dome injury. Stages 1–4 consist of progressively worse injury to the chondral surface. Specifically Stage 1 is a lesion only within the articular cartilage. Stage 2 injuries represent bony trabecular compression with (2A) or without (2B) surrounding bony edema. Stages 3 and 4 describe increasing degrees of osteochondral fragment separation (Fig. 8.2). These injuries can be treated with microfracture. Stage 5 indicates subchondral cysts and avascular bone (Fig. 8.3). These type of lesions are often treated with bone grafting, either autogenous or allograft.7
Fig. 8.2
AP T1 MRI (a) and lateral T2 (b) showing lateral transchondral lesion. Debridement of same lateral transchondral lesion (c), after debridement (d), introduction of microfracture pick (e), placement of microfracture pick (f), after performing microfracture: note bleeding (g)
Fig. 8.3
Osteochondral lesions with cystic and avascular bone. AP T1 (a) and lateral T1 (b)
Other classification systems have been described often to help base treatment. Scranton and McDermott added a fifth stage to Berndt and Hardy’s system for lesions having an intact cartilage cap, but cystic underlying bone. “Bone bruises” occur with ankle injuries and are visible via MRI in up to 39% of cases. Asymptomatic lesions can occasionally be seen, but may not require treatment, though the incidence of this is not well studied. Chondral injuries are visible arthroscopically in 66% of acutely arthroscoped ankles.8 Ferkel and Cheng created a specific arthroscopic classification system for chondral injuries having six grades (A-F) ranging from smooth cartilage (A), rough (B), fibrillated/fissured (C), flap or exposed bone (D), loose undisplaced fragment (E), or displaced fragment (F).6
The talo-tibial articulation is very critical. It has less room for derangement as 1 mm of displacement can create load imbalance due to toss of talar contact of 30–40%. This subsequent malalignment leads to premature wear, and is common with lateral ankle sprains. This can induce chondral and osteochondral injury.9
Recent literature has increased significantly in the past decade as to the results of treatment of talar lesions. Nonsurgical treatment can be attempted and may be successful for early chondral injuries and true “bone bruises” (i.e., micro-trabecular fractures), which generally consists of a period of non-weightbearing and immobilization. There is no uniform nonsurgical treatment regimen for talar injuries, partly due to variability in classification. Unfortunately, just as the preoperative classification and nomenclature vary, so does the postoperative assessment scoring systems. When dealing with athletic patients, one has to take into consideration “down-time” and return to activity (RTA) time frames. In general, treatment of osteochondral lesions has a longer RTA than chondral lesions.3
Surgical treatment is recommended for most talar articular lesions that are deep, large, involve bony defects, and/or are displaced. Osteotomy may be required in many cases to gain access to talar lesions. In fact, recent studies have shown accessibility of talar osteochondral lesions can be limited, and which osteotomies may be needed.10–13 Lesion location traditionally has been classified as antero-lateral and poster-medial on the talar dome. This recently has been refuted by studies. Central lateral and medial locations are actually the most common, whereas the classic locations are actually less common. Elias et al reviewed 428 MRI studies of ankle with talar dome injuries. Mid-medial lesions were the most common occurring 227 times (53%) while true posterior medial lesions only occurred 58 times (14%). Central lateral defects were the second most common lesion, making up 26% of the cohort.14 Osteotomy may be needed to gain access to central lesions. In addition to medial malleolar and fibular osteotomies to gain access to medial and lateral lesions respectively, other oblique osteotomies may be preferred (Fig. 8.4).10–15 Recent study of postero-lateral lesion access has shown fibular osteotomy gives significantly increased access.10 Another study on accessibility showed a unique anterior tibial wedge osteotomy gives good access for central and medial lesions.11




Fig. 8.4
OCDs requiring osteotomies. Medial malleolar (a–c), central pyramidal (d) and lateral malleolar (e, f)
Procedures for large osteochondral deficits could also require either fresh allograft or a second surgery for articular cartilage re-implantation, which has even longer RTA.15–17 Microfracture and drilling are typical first-line treatment for chondral defects and smaller osteochondral lesions.18–22 Furthermore, long-term evaluation of the traditional debridement and drilling of “osteochondral” lesions has shown that 35% of patients note deterioration over time.23 This gives credence to bone grafting procedures for true osteochondral defects. Authors have shown favorable results from autogenous bone graft without cartilage transfer.3,24 Retrograde drilling with insertion of bone graft for lesions with intact articular cartilage has shown favorable results as well.20,25 Other treatment methods such as cartilage re-implantation and osteochondral allograft have been studied, but due to increased morbidity and cost are not recommended as first-line treatment.15–18
8.1 Treatment Protocols
Based on current research outcomes and RTA, the author recommends the following protocols.
8.1.1 Transchondral Talar Lesions
Typical treatment of transchondral talar lesions (TLTs) involves debridement and microfracture of the lesion when there is full-thickness cartilage loss (Fig. 8.5). Generally this is done arthroscopically visualizing with either a 2.7- or 4.0-mm 30° arthroscope. Standard antero-lateral and antero-media portals are created. Other accessory portals are used as needed. Transmalleolar drilling can be performed either with image-guidance or directly through visualization of an osteochondral trephine hole opposite the lesion for medial defects.26 Details of this procedure are found elsewhere in this text. If the cartilage lesion is a large viable flap, fixation to the talus can be performed. This is often performed with bio-fixatives. In cases where the cartilage appears to be grossly intact under direct inspection, retrograde drilling can be performed. This is done under image and arthroscopic control (Fig. 8.6). Newer arthroscopic equipment allows for easier performance of these techniques in the ankle (Fig. 8.7). Postoperatively, patients are kept non-weightbearing for a minimum of three to six weeks, using a below-knee cast boot unless an osteotomy was performed. In those cases, patients are kept non-weightbearing for six weeks, with the first three weeks in a cast. After weightbearing is initiated, patients are maintained in the boot until 6–12 weeks post-surgery. (The longer time frame is for those undergoing osteotomy.) Physical therapy is initiated at 6–10 weeks post-surgery. Return to sports typically takes three or more months.
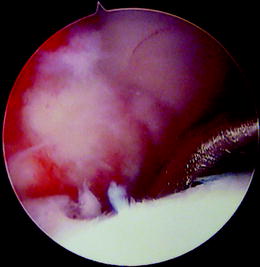

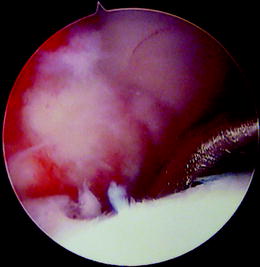
Fig. 8.5
Microfracture pick for a transchondral lesion
Fig. 8.6
MRI of a lesion (a) requiring retrograde drilling via image (b, c)

Fig. 8.7
Radiolucent guide (Arthrex, Inc., Naples, FL USA) to assist with retrograde drilling and bone grafting (Courtesy Arthrex, Inc., used with permission)
Difficult TLT cases are those lesions that involve a large portion of the talar surface area, bipolar lesions and corner lesions. Initial treatment can include above proposed methods. However, if lesions do not yield asymptomatic relief, other options described below may be needed.
8.1.2 Osteochondral Lesions of the Talus
True osteochondral lesions of the talus involve bone loss. The supporting surface of the talus is stressed more due to this loss of structure. Research supports the theory that replacing the bone both with (i.e., OATS or osteochondral autologous/allograft transfer) and without cartilage provides good relief.3,25 Based on Ferkel et al’s long-term study which showed drilling and currettement alone of osteochondral lesions yields favorable results only 72% of the time, supports the need for bone replacement.24 The author prefers to perform autologous morselized bone graft to these defects. Osteotomy may be needed to gain access, along with metallic fixation for postoperative stabilization. (Ideally titanium screws and plates are used so as to allow for additional MRI evaluation.) After curettage of the lesion, often via open arthrotomy, autogenous bone is harvested from the medial malleolus (for medial lesions), lateral calcaneus (lateral lesions), or ipsilateral iliac crest (large lesions), and tamped into the defect (Fig. 8.8). In some cases, retrograde drilling and bone grafting can be performed. Bone can be tamped into place when articular cartilage is intact but bone void exists (Fig. 8.6). Longer-term study is needed of these techniques but short-term results of retrograde drilling for talar osteochondral defects (OCDs) appear promising and have the benefit of preserving the cartilage surface.27










