Osteochondral Autograft “Plug” Transfer
F. Alan Barber
William M. Weiss
DEFINITION
Osteochondral autograft “plug” transfer is a technique for treating full-thickness, localized articular cartilage lesions with or without subchondral bone loss in a nonarthritic joint.
Cylinders or “plugs” of healthy cartilage, with their associated tidemark and subchondral bone, are harvested from one location in the joint and press-fit into same-length recipient holes previously prepared in the lesion to restore the bone and articular surface contour.
Multiple plugs may be transferred to the same region, depending on the defect size.
ANATOMY
Articular cartilage has a complex structure and plays a vital role in normal and athletic activity. It transmits load uniformly across the joint and provides a smooth, low-friction, gliding surface.
Articular cartilage is a smooth, viscoelastic, hypocellular structure with a low coefficient of friction (estimated to be 20% of the friction seen with ice on ice) and the ability to withstand significant recurring compressive loads.
The articular surfaces of diarthrodial joints are covered with hyaline cartilage.
Hyaline cartilage is composed of sparsely distributed chondrocytes in a large extracellular matrix made up of about 80% water and 20% collagen.
Collagen fibers provide form and tensile strength; water gives it substance.
Type II collagen accounts for 95% of the total collagen present. The cellular component (chondrocytes) synthesizes and degrades proteoglycans and is the metabolically active portion of this structure.
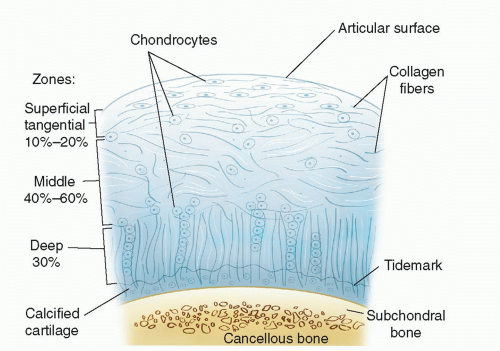
Articular cartilage has four distinct zones: a superficial (tangential) zone, a middle (transitional) zone, a deep (radial) zone, and the calcified zone (FIG 1).
The superficial zone collagen fibers are oriented parallel to the joint surface and resist both compressive and shear forces. This zone is the thinnest and is sometimes called the gliding zone.
The surface layer, known as the lamina splendens, is cell free and consists mainly of randomly oriented flat bundles of fine collagen fibrils.
Under that layer are more densely packed collagen fibers interspersed with elongated, oval chondrocytes oriented parallel to the articular surface.
This superficial zone acts as a barrier, limiting the penetration of large molecules into the deeper zone and preventing the loss of molecules from the cartilage into the synovial fluid.
The middle (transitional) zone collagen fibers are parallel to the plane of joint motion and resist compressive forces.
This zone has more proteoglycans and less water and collagen than the superficial zone.
The chondrocytes are more spherical with more cellular structures, suggesting a matrix synthesis function.
The deep (radial) zone fibers are perpendicular to the surface and resist both compressive and shear forces.
The collagen bundles are arranged in a formation known as the arcades of Benninghoff, in which the round chondrocytes are arranged in columns perpendicular to the joint surface.
The tidemark is located at the base of the deep zone and resists shear stress. It represents a zone of transition from the deep zone to the zone of calcified cartilage.
The calcified zone acts as an anchor between the articular cartilage and the subchondral bone.
It is the deepest zone and is a thin layer of calcified cartilage creating a boundary with the underlying subchondral bone.
The cells in this zone usually are smaller and are surrounded by a cartilaginous matrix.
PATHOGENESIS
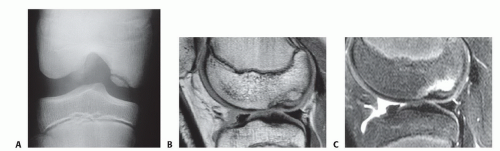
Chondral damage can result from a variety of mechanisms, including a pivoting twisting fall, significant direct impacts on the knee, anterior cruciate ligament (ACL) tears, or a patellar dislocation (FIG 2).
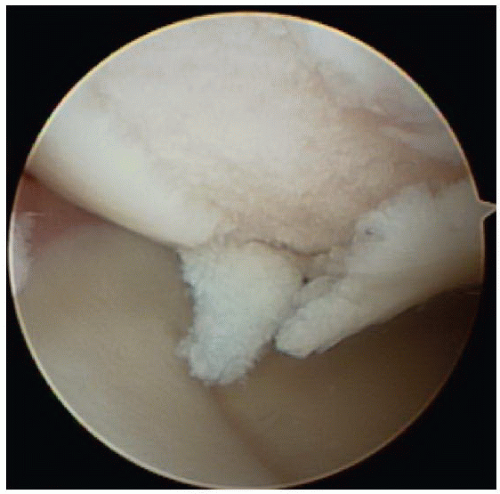
FIG 2 • Chondral damage can result from a variety of mechanisms, including a pivoting twisting fall or significant direct impacts on the knee.
ACL injuries may lead to instability and cause direct contusions to the articular surfaces and localized, full-thickness articular cartilage defects.
Osteochondritis dissecans (OCD) involves the separation of subchondral bone and cartilage from surrounding healthy tissues.
It most commonly occurs in the lateral aspect of the medial femoral condyle.
Traumatic osteochondral lesions include acute bone and cartilage loss due to fracture, crushing, or shear injuries.
Sometimes, even without a clearly remembered traumatic event, the patient develops pain with weight bearing.
NATURAL HISTORY
Cartilage biopsy samples overlying bone bruises have shown degeneration, necrosis of the chondrocytes, and a loss of proteoglycan.
An experimental model suggests that a severe bone bruise and its associated chondral necrosis are precursors to degenerative changes.22
Instability secondary to ACL loss has been shown to contribute to the onset of osteoarthritis after ACL tears.23
Articular cartilage has limited regeneration potential.
PATIENT HISTORY AND PHYSICAL FINDINGS
Full-thickness articular cartilage lesions are associated with various mechanisms of injury, including pivoting, twisting falls, direct impacts, and patellar instability.
Full-thickness chondral lesions are often clinically silent and should be suspected in the setting of any traumatic hemarthrosis, especially with a ligament disruption.
Reports of pain localized to one compartment, a persistent dull aching pain worsening after activity, and pain most noticeable when falling asleep are common.
Running, stair climbing, rising from a chair, and squatting may aggravate the symptoms, as does sitting for a prolonged period.
Physical findings include joint line tenderness, effusion, crepitus, grinding, or catching.
OCD has no exclusive physical findings. In the past, the Wilson sign was thought to be diagnostic of medial femoral OCD. This sign consists of producing pain by internally rotating the tibia during knee extension between 90 and 30 degrees of flexion and then relieving that pain by externally rotating the tibia. However, currently, Wilson sign is felt to be of little diagnostic value.
Effusion is nonspecific but suggests intra-articular pathology.
Pain on direct palpation of the femoral condyles may indicate cartilage damage.
Decreased range of motion is nonspecific but often indicates pathology.
The Lachman test detects ACL instability that may lead to cartilage injury.
Malalignment of the tibia to the femur when standing may lead to abnormal chondral wear.
A positive patellar apprehension test signals damage to the medial patellofemoral ligament.
IMAGING AND OTHER DIAGNOSTIC STUDIES
A standard radiographic knee evaluation should be performed.
This includes standing anteroposterior (AP) views in full extension to identify angular changes and to compare joint space height.
A 45-degree flexion posteroanterior (PA) weight-bearing view may identify subtle joint space narrowing.
A non-weight-bearing lateral view obtained in 45-degree flexion in which the posterior femoral condyles overlap, an axial view of both patellae to help evaluate the patellar alignment, and an AP knee flexion view to outline the femoral intercondylar notch also should be obtained.
OCD lesions are most commonly found in the lateral aspect of the medial femoral condyle (FIG 3A) and are best demonstrated on an AP knee flexion view.
Long-leg hip-to-ankle films accurately determine varus or valgus alignment.
Proper magnetic resonance imaging (MRI) protocols have high sensitivity and specificity.
MRI has evolved into a proven tool to evaluate chondral surfaces and detect full- and partial-thickness lesions that may be clinically silent (FIG 3B,C).
Clinically proven cartilage-sensitive sequences include T1-weighted gradient echo with fat suppression and fast spin echo sequences with and without fat suppression.
Many newer sequences offer promise but have not yet been validated.24
MRI can be an effective tool in managing OCD.
A high T2 signal retrograde to the OCD lesion is commonly seen.
MRI is reliably sensitive to juvenile OCD lesions and a good predictor of low-grade, stable lesions. However, MRI predictability for high-grade, unstable juvenile OCD lesions is less reliable.
Combined single-photon emission and conventional computerized tomography (SPECT/CT) may hold future value as alternative diagnostic imaging modality for symptomatic patients who have previously undergone treatment for osteochondral lesions.
DIFFERENTIAL DIAGNOSIS
Partial- or full-thickness cartilage lesion
Osteonecrosis
OCD
Meniscal tear
Ligament injuries
NONOPERATIVE MANAGEMENT
Nonoperative treatment for full-thickness, discrete chondral lesions consists of physical therapy, anti-inflammatory medication, and activity modification to avoid high-impact or patella-destabilizing activities.
Patellar stabilizing braces for patellofemoral instability and load-shifting braces that unload the injured compartment are options.
Unloading the compartment can also be accomplished with shoe inserts that provide an appropriate heel and sole wedge.
These efforts are more effective for medial femoral condyle lesions than lateral ones.
It is important to ensure that the patient understands that full-thickness lesions have little spontaneous healing capacity and that further degeneration is likely.
SURGICAL MANAGEMENT
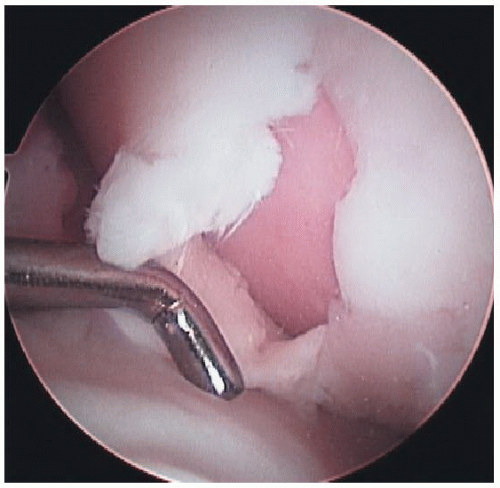
The indications for osteochondral autograft plug transplantation include discrete, isolated, full-thickness articular cartilage lesions with good articular cartilage margins between 1.0 and 2.5 cm2 (FIG 4).
Acceptable results with larger defects have been reported but not consistently.
If the depth of subchondral bone loss exceeds 6 mm, it will be necessary to lengthen the harvested plug accordingly to make up for the increased loss and effectively bone grafting the defect.
Contraindications include opposing full-thickness articular cartilage damage (“kissing” lesions), multiple-compartment full-thickness lesions, significant angular changes, history of joint infection, intra-articular fracture, and rheumatoid arthritis.
This technique is most commonly performed on the femoral condyle; however, osteochondral autograft transplantation of the trochlea, patella, tibial plateau, humerus, elbow, talus, and lunate has been reported.
The COR Osteochondral Repair System (DePuy Mitek, Inc., Raynham, MA) allows for the no-impact harvesting of a precisely sized osteochondral autograft plug and the low-impact transplantation of the plug into a precisely drilled recipient site in the defect. The technique illustrated here uses this system.
Key to the success of osteochondral autograft plug transfers is a perpendicular orientation of the plug in the recipient site. The COR osteochondral repair system has a unique perpendicularity guide which aligns the Harvester and then the inserter in the correct position.
Other systems exist, including the Osteochondral Autograft Transfer System (OATS; Arthrex, Naples, FL) and Mosaicplasty (Smith & Nephew Endoscopy, Andover, MA).
Significant technical differences exist in these systems.
Preoperative Planning
The success of this procedure depends on maintaining viable chondrocytes. Various studies confirm that greater pressure on the articular cartilage cells leads to cell death. Several technical issues are related to greater transplanted cell death. These include high-impact pressure during insertion, proud grafts which are not advanced to the level of the adjacent native articular cartilage, and sunken grafts depressed 2 mm or more compared to the adjacent articular cartilage.
The ideal technique optimizes graft position and stability, provides for consistent graft length harvesting, and minimizes the forces required to insert the grafts.
Other procedures can be performed at the same time as osteochondral autograft plug transfer, including meniscal repair, osteotomies, and ligament reconstruction.
Improved results in unstable knees occur with concomitant ACL reconstruction.20
Any ligament instability or malalignment should be corrected at the time of autografting to avoid increased failure rates.
Radiograph and MRI studies should augment the arthroscopic assessment of the lesion to confirm the decision whether an arthroscopic or open approach is required.
Perpendicular placement of the harvester and drill to the articular surface is required.
The COR transfer system has a unique “perpendicularity” guide which enhances the perpendicular harvest of the donor graft as well as the perpendicular orientation of the drilled recipient site.
If the potential use of allograft material is suspected, it should be available in the operating room before surgery begins.
Although allograft tissue avoids the issue of harvest site morbidity, it is offset by the risks of transmitted disease and decreased chondrocyte viability19 and results in significantly increased cost.
Positioning
Osteochondral autograft transfer in the knee is performed with the patient supine and the operative knee in an arthroscopic leg holder flexed off the table.
It is crucial to confirm that the knee can be flexed adequately to access the lesion before operative preparation and draping. This may require placing the leg holder more proximal than usual. The ability to flex the knee to at least 100 degrees is preferred.
The contralateral leg should be well padded and positioned out of the operative field.
It may be necessary to drape the operative leg free of a leg holder to obtain enough knee flexion to access the lesion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree