Fig. 7.1
Arthroscopic view of cartilage lesion with palpable defect
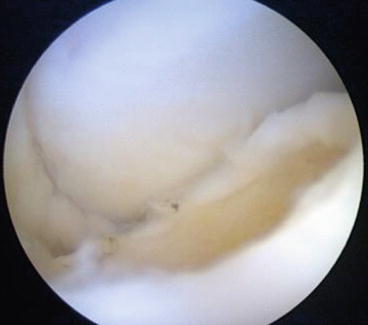
Fig. 7.2
Articular bone bed after curettage of cartilage injury

Fig. 7.3
After performing microfractures with bleeding bone bed
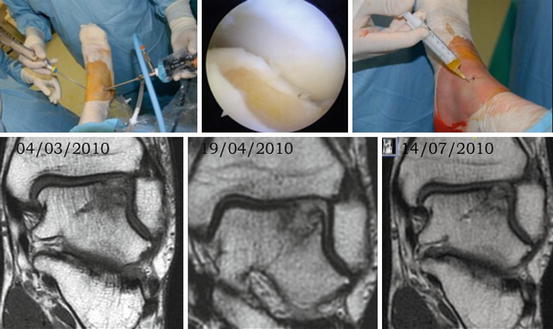
Fig. 7.4
The superior images show the arthroscopic access with the two anterior portals. The central image shows the talar articular surface without cartilage defect and the bone bed. The superior right image shows the application of PRGF-Endoret at the end of the surgery in the joint space. The inferior images show the changes of an osteochondral lesion over a 4-month period treated arthroscopically with curettage, microfractures, and application of PRGF-Endoret. The patient presented at the final follow-up with the MRI, without pain, and had recovered full mobility having returned to normal daily life activities including running and contact sports
Clinical improvements have been reported in different studies on cartilage lesions with the use of plasma rich in growth factors (PRGF) [47, 48]. When working with PRGF, the methodology described by its author should be followed with regard to its preparation and application to ensure traceability [46] and thus render the results comparable to the various studies published. As indicated by Taylor, when obtaining PRP, taking different paths leads to the preparation of different products, with the huge possibility of getting different results [49].
Giannini presents favorable results in a 4-year follow-up with improvements in AOFAS scores and objectified by MRI T2 mapping sequences. Patients were treated in one surgical procedure with bone marrow-derived cell transplantation [7]. The study with meta-analysis by Niemeyer evaluated 16 publications with autologous chondrocyte implantation wherein he concluded that although clinical outcome as described in the studies available seems promising (with regard to a lack of controlled studies), a superiority or inferiority to other techniques such as osteochondral transplantation or microfracturing cannot be estimated [23]. Paul et al. presented a series treated by talar osteochondral transplantation where they found that patients modify their postoperative sports activities, and they noted a reduction of participation in high-impact and contact sports [25].
7.6 Conclusions
The series described here is composed of a highly homogeneous population of federated soccer players of similar age. Treatment by arthroscopy and debridement is not extremely aggressive and provides good results in terms of functional recovery. Based on the review of the literature, there are insufficient works with high levels of evidence that recommend a specific type of treatment in cases of osteochondritis of the talus. However, based on the accumulated experience gained at Mutualitat de Futbolistes which provides medical assistance to more than 140,000 athletes with more than 22,000 injuries per year, ankle osteochondritis (if symptomatic) is initially treated conservatively by physiotherapy and with biological techniques such as the infiltration of plasma rich in growth factors. If conservative treatment fails, surgical techniques are indicated with ankle arthroscopy and curettage of the lesion down to healthy bone and the application of articular PRGF-Endoret®.
References
1.
2.
Badekas T, Takvorian M, Souras N (2013) Treatment principles for osteochondral lesions in foot and ankle. Int Orthop 37(9):1697–1706CrossRefPubMedCentralPubMed
3.
4.
5.
Caylor MT, Pearsall AW 4th (2002) Fresh osteochondral grafting in the treatment of osteochondritis dissecans of the talus. J South Orthop Assoc 11(1):33–37PubMed
6.
7.
8.
9.
10.
11.
Grady J, Hughes D (2006) Arthroscopic management of talar dome lesions using a transmalleolar approach. J Am Podiatr Med Assoc 96(3):260–263CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







