(1)
Department of Orthopedic Surgery ASAN Medical Center, University of Ulsan College of Medicine, Seoul, Korea, Republic of South Korea
Abstract
The development of surgical tools and technology has extended its territory to newer surgical fields. Good examples include computer assisted surgery and arthroscopic surgery.
10.1 Introduction
The development of surgical tools and technology has extended its territory to newer surgical fields. Good examples include computer assisted surgery and arthroscopic surgery.
The introduction of computers in arthroplasty has improved the accuracy of the operation and the use of robots has made it possible to reach the lesions where human hands cannot reach. Also, attempts have been made to reduce morbidity and to allow early mobilization by minimizing the length of the incision. Minimal incision and computer assisted surgeries have become the optional techniques of arthroplasty.
In this chapter, I would like to describe Computer Assisted Orthopedic Surgery (CAOS) and Minimally Invasive Surgery (MIS).
10.2 Computer Assisted Orthopedic Surgery
10.2.1 Overview
The prognosis of arthroplasty is affected by the patient-related factors, implant-related factors, surgical techniques and postoperative management. Among all these factors, the most important factor is the surgical techniques.
The surgical procedures that affect the prognosis include the approach, osteotomy, ligament balancing and fixation. In terms of alignment, the failure rate significantly increases if there is more than 3–4° varus or valgus malalignment and the ROM decreases by 20° even if there is just 2.5 mm of difference in the A–P position of the femoral component. Teter et al. reported that 8 % of cases showed malalignment of more than 4° when an extramedullary guide was used for the tibial osteotomy. However, this is based only on the two dimensional X-rays and a higher incidence of malalignment may be noted in the three dimensional plane. Such an error is detected in about 10 % of cases performed even by the experienced surgeons, since the performance of an operation largely depends on the judgment of the eye and experience of the surgeon. Computer assisted surgical techniques were developed in order to minimize the errors that can develop with the conventional techniques. Of course, even with the use of computers, surgical errors can occur during the placement of cutting blocks, the actual performance of osteotomy or fixation of prosthesis, etc. Although the occurrence of errors varies according to the type of computer system, computer assisted surgery aims to achieve malalignment of less than 1° and malpositioning of less than 1 mm through the use of a navigation system for osteotomy and balancing.
Currently, it is believed that alignment in the coronal plane is accurate when the navigation system is used. In the sagittal plane, however it is difficult to assess the accuracy as there is still no definite theory regarding the sagittal axis. CAOS tends to cause slight hyperextension compared to that with the conventional technique because the center of motion does not coincide with the center of mechanical axis in sagittal plane. There are still problems to be solved with respect to the rotational alignment. Currently, computer assisted surgical techniques are used not only for osteotomy but also for soft tissue balancing using a tensioner or distractor.
The benefit of computer assisted surgery in the artificial joint is that it is accurate and highly reproducible. As the medullary guide is not needed, bleeding and the risk of embolism are reduced and there is an improvement in the documentation that helps in the research.
The drawbacks of this technique are that a longer operation time is required and it is expensive. Computer assisted systems can also give rise to errors. The causes of errors include registration errors (error in, error out), and problems not related to the computer system but related to the surgical techniques, e.g., change of position of the cutting block during drilling, incorrect use of ligament alignment jig, incorrect osteotomy due to a wide slot or flexible cutting blade, or improper cementing for fixation, etc. Also, a learning curve is involved for using this technique, and the surgeons who have a poor understanding with the conventional techniques are likely to make errors.
10.2.2 History
Computer assisted surgery was first used in a neurosurgical operation for the brain and spine in the 1980s for determining the accurate location at which the operation was to be performed.
In orthopedic surgery, it was first used by Kaiura in 1986 to determine the center of the femoral head with the robot by applying the kinematic registration technique through the preoperative CT scan. In the 1990s, it was introduced in TKA after accurate pointing of the important landmarks was possible. Soon afterwards, fluoroscopy was used to obtain images during the operation until Saragaglia et al. developed a navigation system using the OrthoPilot for imageless surgery in 1997.
10.2.3 Type
There are various types of computer assisted surgery systems produced by different manufacturers, but Picard classified them according to the performance and the method used to obtain the image. In terms of performance, there are active, semi-active, and passive types of computer assisted surgery systems, and in terms of the method used to obtain the images, there are image-free, preoperative image-based, and intraoperative image-based types. When all these systems are taken into account in combination, theoretically there can be nine types (3 × 3), but not all these combinations do actually exist.
10.2.3.1 Classification According to the Performance
Active System
Active type uses computer systems in all or part of the preparation and operative procedure and the robot system is included in this type. In the robot system, the robot performs the surgery instead of the surgeon and the accuracy is very high. It was used limitedly in the early stage of computer assisted surgery, but it has been transformed into the modern robot assisted surgery since the development of the navigation system.
The robot can perform osteotomy and soft tissue release without any injury to the ligaments, nerves or vessels. Robot systems include the Robodoc and Caspar systems, and these systems perform concise, clear, accurate and effective three-dimensional operations (Fig. 10.1). Also, some of the surgical procedures such as intramedullary drilling can be avoided just like in the navigation surgery. It helps in cementless prosthesis due to an accurate osteotomy as it mills the surface without sawing.
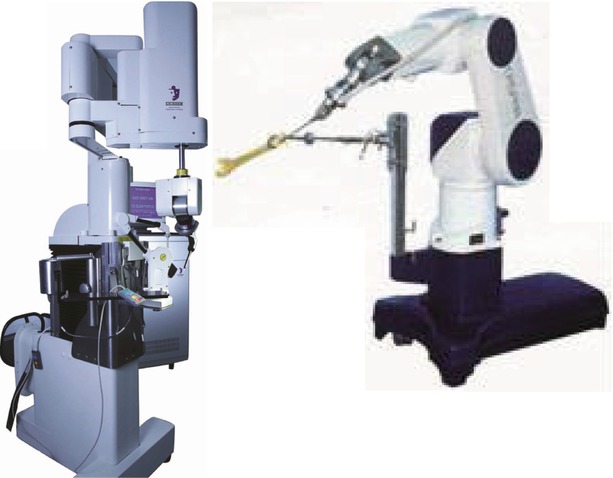
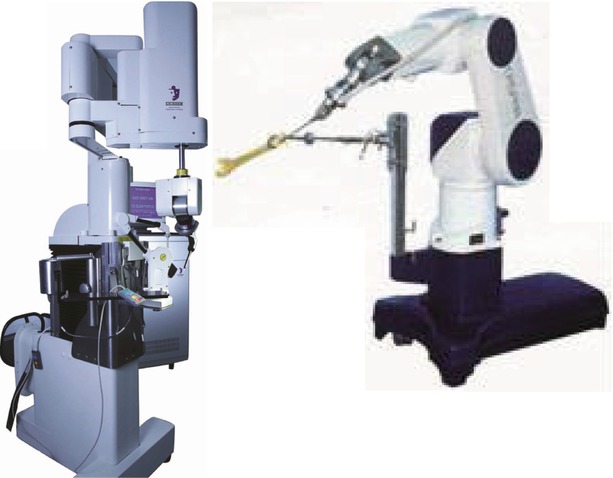
Fig. 10.1
ROBODOC (Integraged surgical systems, Davis, CA) and CASPAR systems (U.R.S.-ortho GmbH & Co. KG, Rastatt, Germany)
Robot assisted surgery comprises of the pin type or the pinless type and preoperative CT is required for both types. In the pin type, a stab wound is made under local anesthesia before the operation and a self-tapping screw is fixed onto the pelvic bone, femur and tibia. These screws act as indicators of spatial orientation of the patient’s real bone for three dimensional verification. In the more recently developed pinless type, the process of inserting the pins before surgery is bypassed. Patient information based on the CT images including the position of the joint, size of the tibia and femur, and degree of deformity is stored in the computer, which enables to perform cyber surgery and to plan the operation. During the operation, the robot and the knee should be securely fixed to prevent micro-motion. The actual shape of the patient’s joint and bone is matched with the information already stored in the computer using a probe attached to the robotic system. This process of registration and verification is the most important step in robotic surgery. Once the registration is completed, the robot mills the bone finely and accurately with an error of less than 0.25 mm as planned during the preoperative cyber surgery, and then the pre-selected prosthesis is inserted to complete the operation (Fig. 10.2).
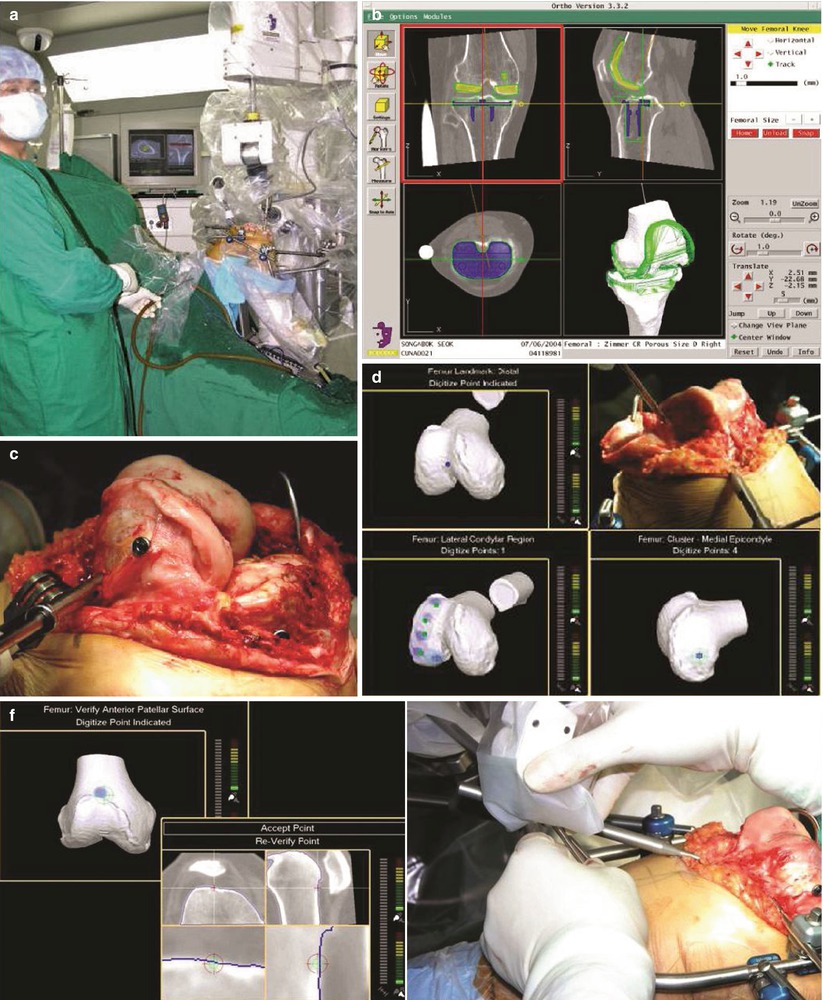
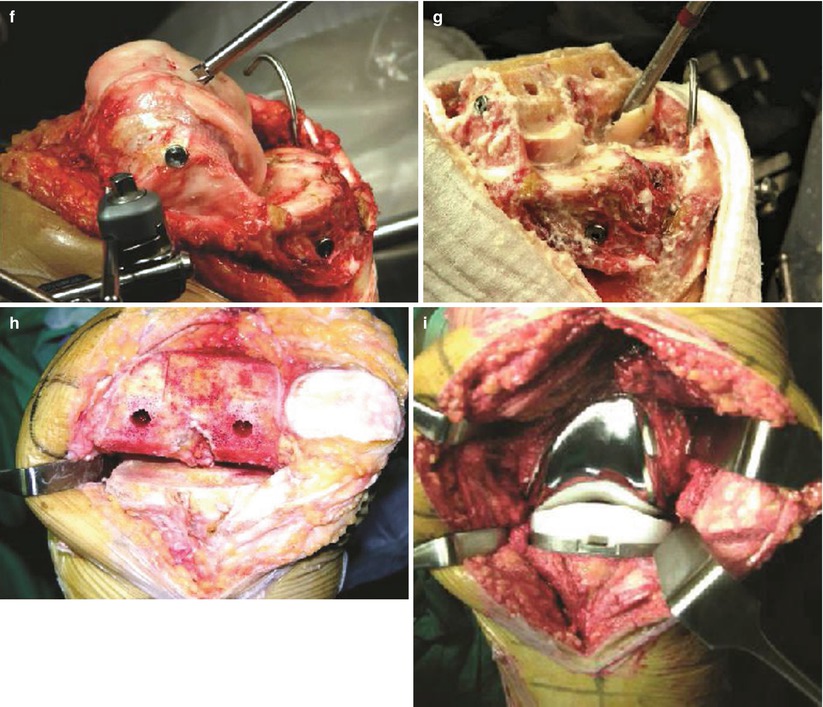
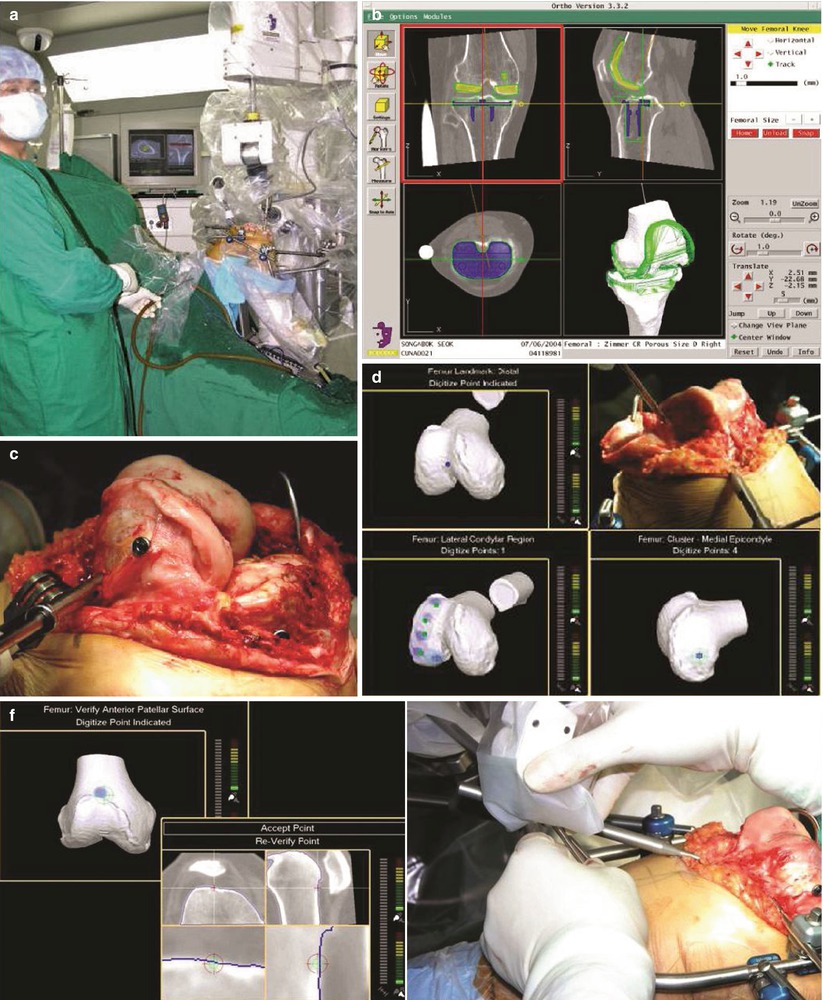
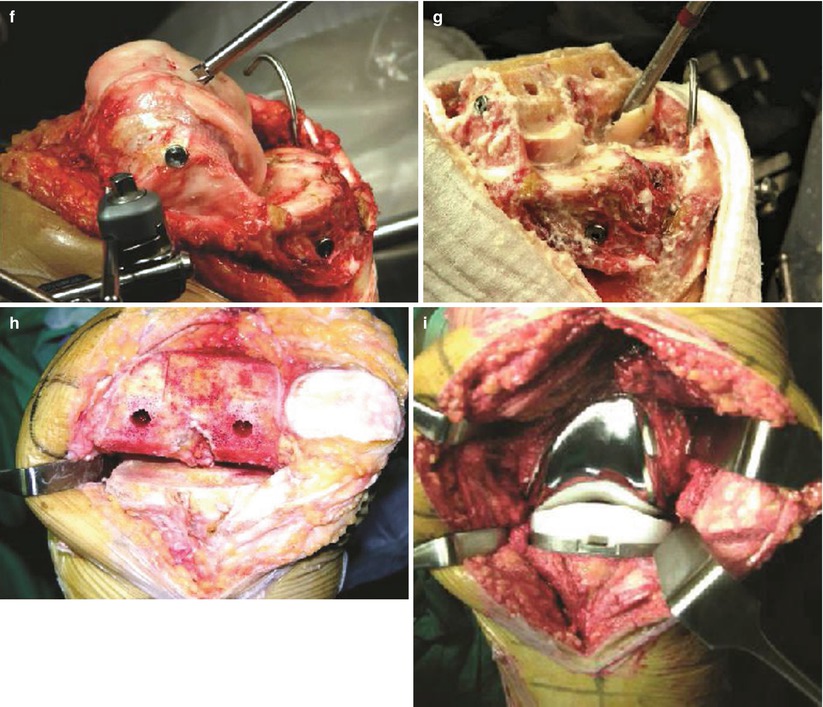
Fig. 10.2
Operative procedures of pinless Robodoc system. (a) Robodoc system, (b) planning through the preoperative cyber surgery, (c) exposing the joint and inserting the screw into the femur, (d) registration process, (e) verification process, (f) immediately before milling the bone, (g) milling process, (h) after milling the bone, (i) after inserting the prosthesis
However, the robot system requires preoperative imaging and registration, it is bulky, it may hinder the normal operation process, and it is too time-consuming and expensive. A learning curve is also needed for using the robot system.
Saragaglia et al. reported that accuracy with less than 3° outliers can be achieved in 75 % of patients when the computer was not used, in 84 % of patients when the computer was used and in more than 95 % of patients when the robot system was used. Park and Lee reported the comparison between the robot system and the conventional method, which suggested that the robot system was clearly useful in terms of preoperative planning, accuracy and postoperative alignment, but the incidence of complications such as fracture or peroneal nerve palsy was higher in the early period of this technique.
Semi-active System
Surgery is performed by both the surgeon and the robot; the robot guides the surgeon and controls the surgeon when osteotomy exceeds the normal range, or the surgeon can move the robot’s arms. The Acrobot can be classified into the active system or the semi-active system and it also requires preoperative imaging and registration during surgery.
Passive System
Surgery is performed solely by the surgeon. The passive system includes the navigation system and the patient specific instrument (PSI) or the patient-specific templating system. The navigation system is used to guide the operation and it is more recommended by the US FDA.
In arthroplasty, navigation refers to registering the patient information in the computer in order to guide the performance of an accurate operation. Kinematic registration by joint motion detects the center of the joint and a probe is used for surface registration of the size and shape of the bone. This process simulates the real shape of the patient’s bone based on the registered information in order to secure accurate positioning of surgical instruments for osteotomy.
The patient-specific templating system, which is still in its toddler stage, uses preoperative CT or MRI. MRI has the theoretical advantages of detecting the cartilage and of being a radiation free imaging modality. However, MRI images have more segmentation difficulties than CT images, which may be the cause of malpositioning of the template. There are two methods of patient-specific templating system: one is the pin placement technique and the other is the cutting guide technique. In the pin placement technique, a preoperative CT or MRI is used to create the positioning guide in order to locate the position of the pin for osteotomy and the same conventional cutting jig is used (Fig. 10.3 ). In the cutting guide technique, the surgeon uses the custom made guides to perform the osteotomy without using the conventional cutting guide. There are two aligning method in PSI system: one is kinematic alignment and the other is mechanical alignment method. Mechanical alignment method needs detecting the center of hip, knee and ankle joint on CT or MRI to restore mechanical alignment. The MRI or CT of the joint is needed and release of collateral ligaments and retinacular ligament are not performed in kinematic alignment system. The concept of kinematic alignment, is quite different from that of conventional mechanical alignment. The purpose of kinematic alignment is to restore pre-arthritic state to improve clinical result. In case of mechanical alignment method, just similar to conventional instrument method, Nunley et al. experienced more varus outliers than the kinematic alignment method. During the operation, osteophytes should not be removed because they may be used as a reference for positioning the cutting guides. The femoral guides are usually used first to make more space for the tibial cutting guide. So, aligning the joint along the mechanical axis is just a reference. This is described in details under Sect. 4.4.


Fig. 10.3
Patient-specific templating system (Biomet, Warsaw IN)
The advantage of the patient-specific templating system is that the technique is relatively easier to use, less invasive, time saving and accurate. The drawback of this system is that a longer time is required to create the positioning guide, it does not usually provide the intraoperative measurements, lack of information for soft tissue balancing, more chances of poor positioning of the guides due to an MRI alignment error, and the surgeon should abandon the system in case the operation goes wrong. While the navigation system is universally used for all patients, the patient-specific templating system is based on the skeletal information of each patient.
10.2.3.2 Classification According to the Method of Obtaining Images
Image-Based System (CT Scan or Fluoroscopy)
Image-based navigation system is used for osteotomy based on the information acquired from CT scan or fluoroscopy. In this system, either the information from the preoperative CT scan is registered or fluoroscopy is used during the operation to acquire the information (Fig. 10.4).
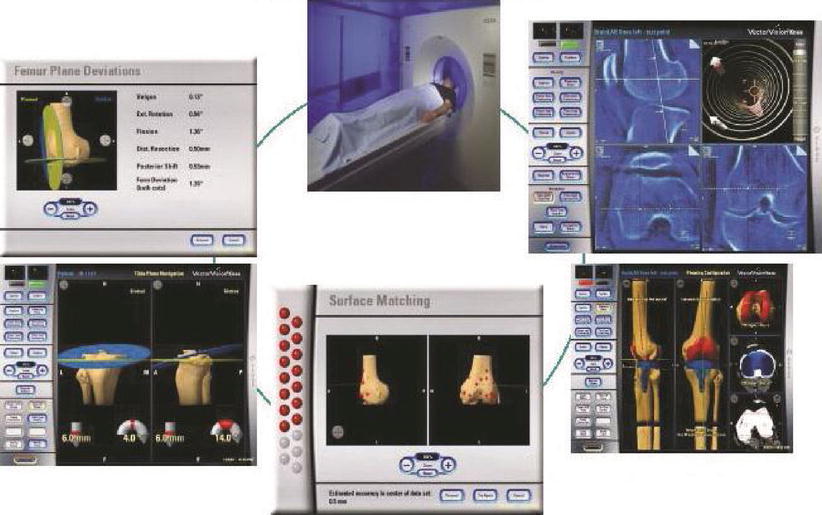
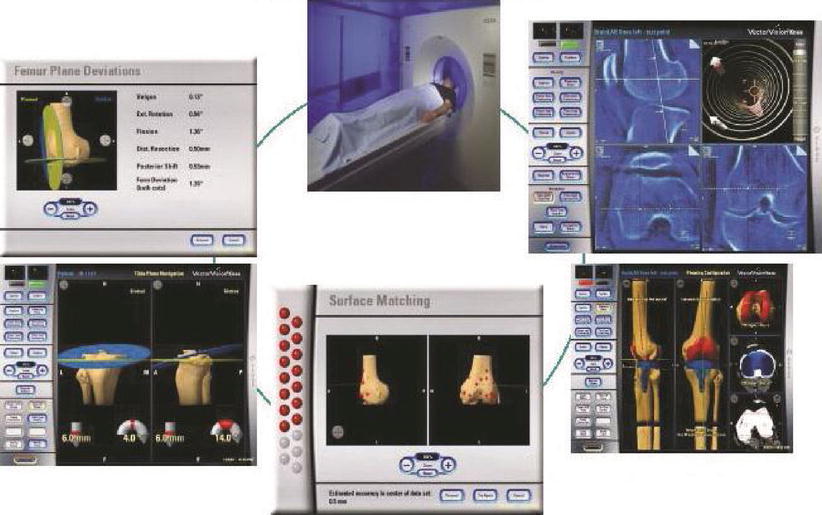
Fig. 10.4
Preoperative acquisition of skeletal information for image-based navigation system (Brainlab, Feldkirchen, Germany)
During the registration, the information acquired from the CT scan or fluoroscopy is stored in the computer system, and the kinematic information of the joint motion and bony information are matched with the input data (kinematic registration) (Fig. 10.5).
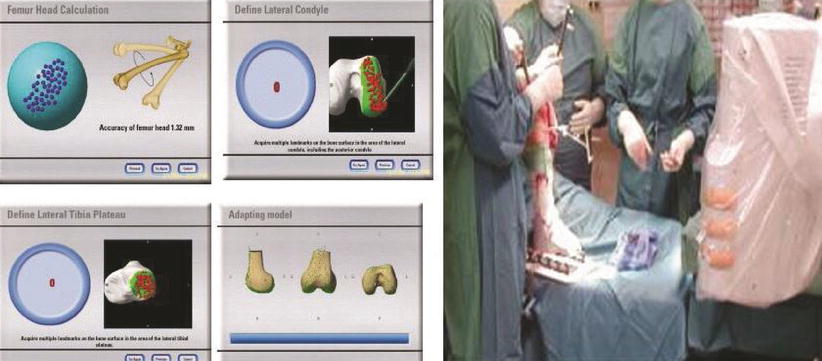
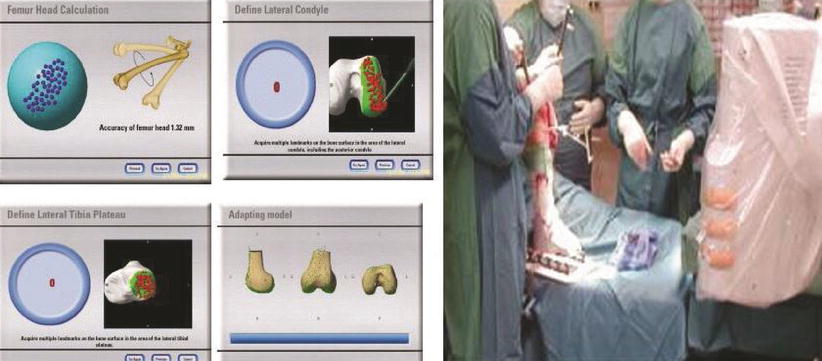
Fig. 10.5
Registration for image based navigation (Brainlab, Feldkirchen, Germany)
Kinematic registration is followed by surface registration which is obtained from the probe during the operation, and these are used to determine the position and direction of the cutting guide in real time for an accurate osteotomy. Therefore, registration is the most important step and the software is also as important as the hardware. If the registration is incorrect, the operation becomes inaccurate. The causes of incorrect registration are the presence of borderline blurs and when segmentation of images occurs. The operation also tends to be inaccurate when the soft tissues impinge between the probe and the bone, when the probe points to a different site because the bone is not perfectly spherical, the cortical screw that fixes the rigid body moves and the computer hardware and software are inaccurate.
The method of using fluoroscopy is the automatic registration system through fluoroscopy during the operation. This method is not convenient to perform the TKA as it requires the use of fluoroscopy. It is more helpful to insert pins in fracture surgery than in arthroplasty.
Image-Free System
Image-based system helps in the preoperative planning and postoperative evaluation, but it has been replaced by the image-free system because the image-based system is more time-consuming and it requires more effort since the acquisition of images before or during the operation is required.
Image-free system does not need preoperative CT imaging or intraoperative fluoroscopy and it incorporates the standard cutting blocks and cutting guides from a preexisting instrument. Currently, the image-free method for acquiring critical anatomic information has proved to be the most effective method for performing TKA. In this system, the standard skeletal structure is used as a basis to track and register the shape, position and axis of patient’s anatomy during the operation, and an osteotomy is guided by the navigation system. It identifies critical anatomic landmarks through both kinematic and surface registration.
For this method, a tracking camera and tracking marker (tracker) are required and this tracker is attached to the bone by a pin or a clamp (rigid body), which is fixed at more than three sites. Other trackers are attached to the surgical equipments and probe to guide the operation. Also, the accuracy can be verified before performing the osteotomy in order to correct malalignment. This system includes an optical system using the infrared light and an electromagnetic system using the electromagnets, and the method using the ultrasound is also being developed.
Optical System
Optical system comprises of an active type and a passive type; the active type has LEDs (light-emitting diodes) attached to the rigid body to emit infrared rays onto the camera and the passive type has reflecting spheres on the rigid body to reflect the light emitted from the LEDs onto the camera. By altering the degree of reflection from sphere to sphere, each set of information is received from each reflecting sphere without any confusion. Therefore in the active type, a cable or battery is required and in the passive type, there is a need to clean the reflecting spheres.
Operation begins by exposing the knee joint, attaching the LEDs (light-emitting diodes) to the rigid body which is fixed onto the bone using special cortical screws and to the surgical tools. The hip joint, knee joint, and ankle joint are moved in that order to detect the center of the three joints and to calculate the three-dimensional motion for measuring the mechanical axis (kinematic registration). The camera (optical localizer: Fig. 10.6) connected to the computer monitor receives the infrared rays emitted from the LEDs attached to the rigid body. When the probe points towards the bony and articular landmarks during the operation, the infrared rays emitted from the LEDs attached to the probe are recorded (surface registration) to acquire the information needed for the operation i.e. the position and direction of the femur and the tibia.
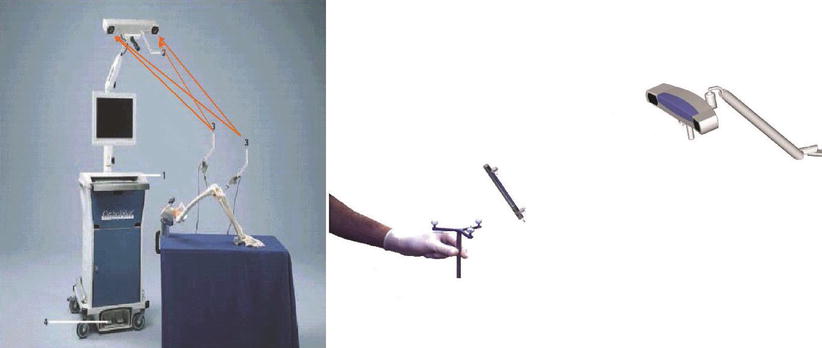
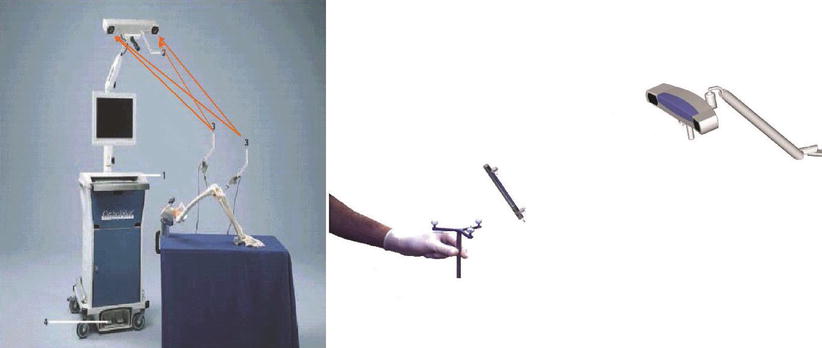
Fig. 10.6
Image-free optical navigation system (Otrhopilot; Aesculap, Tuttlingen, Germany)
Based on this registration, the most ideal osteotomy line and direction are monitored in real time.
When a tensioner is applied to check the tension of the medial and lateral collateral ligaments, the medial/lateral joint space of the knee joint in extension and flexion can be seen on the monitor as numerical values, which is used for ligament balancing (Fig. 10.7). The degree of external rotation can be adjusted according to the extension and flexion gap while performing anterior-posterior osteotomy of the distal femur. Also, the ideal size and position of the prosthesis can be determined so as to perform arthroplasty that is appropriate for each patient.
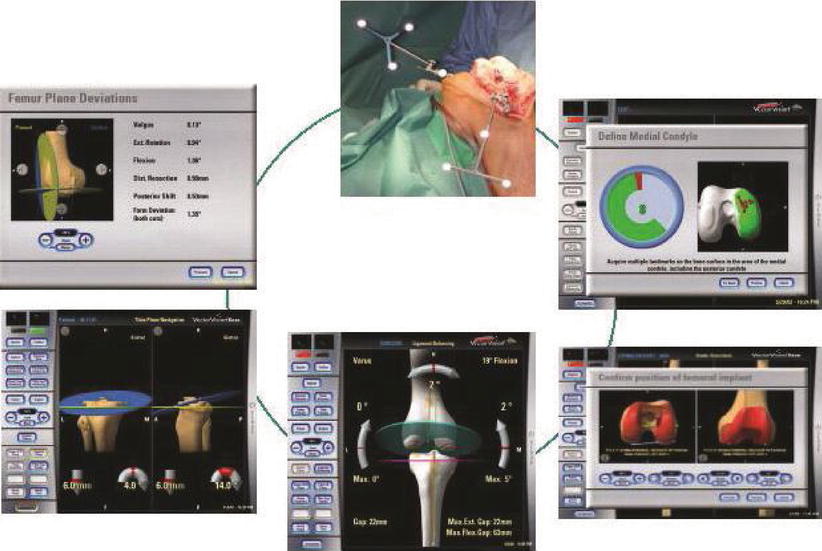
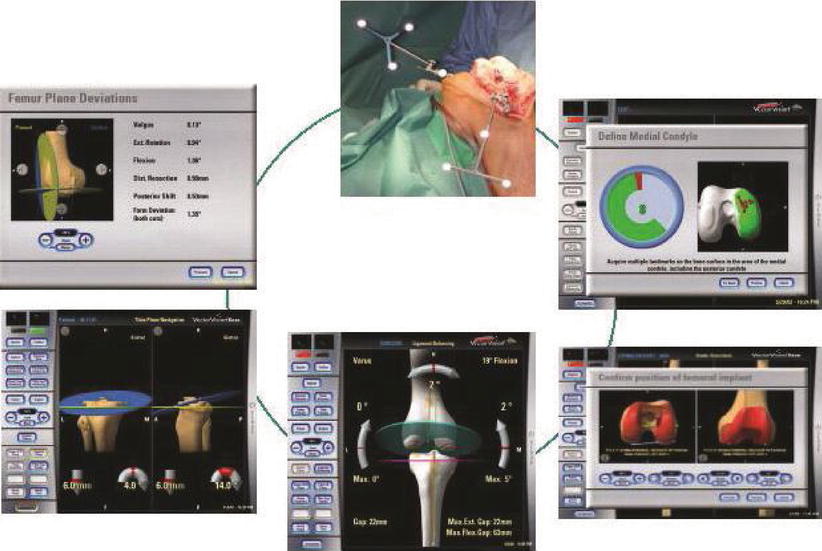
Fig. 10.7
Image-free navigation on the screen
The benefit of the optical system is that it is fast and accurate, and the drawbacks are that the position of the surgeon and the assistants must be selected carefully such that the camera should not interfere the visual field, and the results of surgery can be affected by illumination of the operation room.
Electromagnetic Computer System (EMC)
The navigation system that was used in the early stage had limitation of camera’s visual field and it could only ensure up to 180° of visual field. And the tracker was fixed far away from the operation site using a pin, which caused sterilization problems, soft tissue damage or tethering, and projection of large tools. To overcome these drawbacks, the EMC was developed to obtain non-line-of-sight signal which can pass through the soft tissues and is not related to the visual field.
Electromagnetic computer system (EMC) uses a localizer that creates a weak intensity magnetic field to generate microvoltage and a sensor to detect its intensity. The magnetic field is created by the localizer that can use either direct or alternating current, but alternating current can create a more consistent magnetic field. The localizer has three or more generator coils and the number of coils affects the performance level of the system. More number of coils contribute to more accurate and more diverse functions, but this requires a larger capacity computer. The sensor at a distance from the magnetic field can receive and transmit the information to the computer (Fig. 10.8). This system requires dynamic reference frames (DRFs) to be attached near the operation field, which serve as the tracker.


Fig. 10.8
Electromagnetic computer system (TREON; Medtronic, New York)
This system was first applied in pediatric neurosurgery and otorhinolaryngology due to instability of signals, metallic interference and slow response to positional change. Currently, it has become an additional option for the navigation system in the orthopedic field after increase in the number of generator coils which can be attached to the soft tissues.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








