Fig. 1.1
Operating room dedicated for arthroscopic intervention, equipped with arthroscopic tower, anesthetic device, operating table with “leg holder” device which allows patient position with the knee in variable flexion. The arthroscopic tower incorporates equipement for data archiving

Fig. 1.2
Typical camera, light source, shaver and electro frequency

Fig. 1.3
Optical piece (telescope) at 30°, 4 mm (Hopkins). Forceps, pointed probes and arthroscopic punches
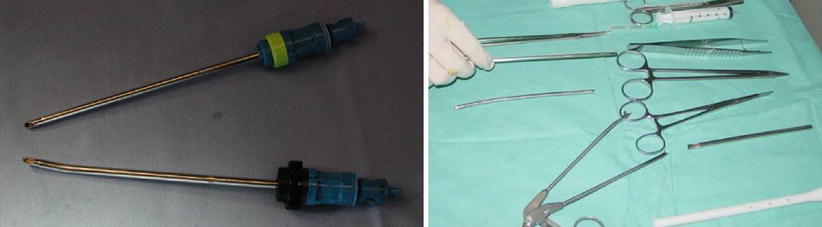
Fig. 1.4
Shaver pieces for soft tissue and miscellaneous instruments (No. 11 scalpel blade)
1.1.3 Positioning
Positioning has to fulfill the following requirements: Accessibility of all joint compartments – the position should permit access to all joint compartments. It should also provide easy access for establishing the arthroscopic and instrument portals; convenience, option for converting to open surgery – if the surgeon decides intraoperatively to proceed with a more complex arthroscopic reconstruction or with open surgery, this should be possible without a change of setup or time-consuming repositioning of the leg. For example, if the leg must be moved to apposition of 90° knee flexion, this should be possible without breaching sterility; simple devices – the device used to hold or position the leg for arthroscopy should be simple and economical. The simpler the positioning device, the faster it can be mounted on the operating table and the shorter the learning curve for operating room personnel; free tourniquet access – there should be unrestricted access to perform surgery with the deflated tourniquet in place and for inflating the tourniquet as needed during the operation. Either a straight-leg of flexed-leg position may be used.
The straight leg position for arthroscopic surgery meets all the requirements for a simple, fast, and secure technique. A simple side post is mounted on the operating table on the lateral side of the thigh. The side post is positioned about a handwidth proximal to the base of the patella. One advantage of this position is that allows the surgeon to be seated during the procedure. Sitting is not only comfortable but is also convenient for applying varus/valgus stresses to open the joint compartments, allowing the surgeon to concentrate on manual manipulation of the arthroscope and operating instruments.
Flexed–Knee Position. In this position the knee is flexed 90° in a padded leg holder. This provides a medial fulcrum so that both varus and valgus stresses can be applied to the knee joint. This positioning technique is disadvantageous in that extra equipment is needed (leg holder), and that the surgeon must stand during the procedure in order to apply varus/valgus stresses to the joint. It is more difficult to control these forces than in the straight-leg position.
Tourniquet. Tourniquet control and limb exsanguinations are controversial issues in arthroscopic surgery. A bloodless field provides the best intraarticular image quality. All surgical manipulation in the knee joint can be done without significant image clouding, and troublesome bleeding is eliminated. IF surgery is performed without a tourniquet, bleeding can seriously obscure vision. This not means, however, that tourniquet inflation or exsanguinations is necessary for every arthroscopic surgery. A discriminating approach is required. The pneumatic tourniquet is placed on the proximal third of the thigh or the junction of the proximal and middle thirds. The shorter and thicker the thigh, the more proximal the tourniquet should be placed, especially if an ACL reconstruction is planned. IF an Arthroscopy is performed with the knee flexed in a leg holder, the tourniquet placement should be coordinated with the position of the leg holder. The tourniquet should be applied just prior to induction of general anesthesia, regardless of whether it will or will not be inflated during the surgical procedure.
All the equipment necessary for the arthroscopy can be arranged separately positioned in a logical order around the operating table, but it is more efficient to place all the devices on a dedicated arthroscopy cart or trolley. The equipment should be arranged in a way that the surgeon can see all important control devices and can quickly detect any malfunctions or faulty settings. The monitor should be at the surgeon’s eye level, so its placement will depend on whether the surgeon works in a sitting or standing position (Fig. 1.5).


Fig. 1.5
Patient positioned on the operating table during sterile draping
In tight joints or cases where difficult surgical conditions are anticipated, whether in the knee or in other joints, optimum muscle relaxation is essential, which can only be accomplished by general anesthesia. It is more easily controlled in terms of onset and muscle relaxation. Even in ambulatory settings, general anesthesia is better for achieving rapid and complete post procedure recovery. Ultra short–acting anesthetics with a short half life are excellent choice under these circumstances.
Spinal or epidural anesthesia can be used for arthroscopic surgery. Spinal anesthesia has a more predictable onset of action, but there is a potential for adverse circulatory effects and for postoperative spinal headache and bladder dysfunction.
Local anesthesia can be administrated by the surgeon himself although a standby anesthesiologist should be available. The preoperative preparations are the same as for other anesthetic techniques. Because local anesthesia does not produce muscle relaxation, difficulties may be encountered in the visualizing the posterior horn of the medial meniscus, for example, or in tight joints. Although local anesthesia is acceptable in theory for most arthroscopic surgeries, it is recommended only for selective cases.
Technique: Infiltration with local anesthetic – once the optimum site for the arthroscope portal has been selected, it can be infiltrated with a local anesthetic (bupivacaine 0.25 %) containing 1:200,000 epinephrine. Approximately 5 ml of solution is sufficient. The injection needle can be advanced into the joint cavity without injecting a large amount of local anesthetic into the joint. An important advantage of local anesthetic is that it prevents minor bleeding from the arthroscope portal in a non – bloodless field. It also numbs the pain – sensitive synovial membrane, so that the patients rarely complain of postoperative pain in the area of the arthroscope portal.
1.1.4 ACL Reconstruction
After anesthesia is performed, the patient is positioned supine on the table with the leg part removed and the feet hanging down. The unoperated leg is placed in a proclivity holder. Alternatively, a normal table can be used. The thigh is placed in the leg holder over the Tourniquet band. Over the patient we use a Mayo table to support the instruments during surgery. It is mandatory that the knee be flexed to over 120° in order to drill the femoral tunnel. Alternatively, flexible reamers can be used [3]. A standard HD arthroscopy tower and ACL instrument set (reamers, guides and graft bench) are prepared (see Sect. 3.5.2.1). We use a shaver, reamer, chair and a second Mayo table compared to when performing arthroscopy alone. We do not routinely use a fluid pump (Fig. 1.6).


Fig. 1.6
Application of the leg holder on the thigh so that the knee can be flexed over 120°. A standard setup for ACL reconstruction with 2 back tables, the surgeon sited, helped by a scrub technician and a resident in training
1.2 Normal Anatomy
1.2.1 The Menisci
The menisci are two semilunar biconcave disks that reside within the medial and lateral tibio-femoral joints. They are fibro cartilaginous C-shape disc interposed between femoral and tibial condyles with strong attachments to bone and poor vascularization throughout its inner 2/3. Once thought as a vestige of leg muscle, they are now considered a vital structure with various functions: chondroprotection through weight distribution by enlarging the contact area between the femur and the tibia, weight bearing, joint stabilization, joint lubrication, articular cartilage nutrition, and proprioception [4].
1.2.1.1 Medial Meniscus
The medialmeniscus is somewhat semicircular in appearance. It is approximately 3.5 cm in length in the anteroposterior dimension and considerably wider posterior than it is anterior. Its radius of curvature varies, giving it greater length in the sagittal plane than in the coronal plane. The anterior horn is attached to the tibial plateau in the area of the anterior intercondylar fossa, 6–7 mm in front of the ACL insertion. An intermeniscal, or “transverse” ligament is present in 64 % of individuals; this connects the anterior horn (posterior fibers) of the medialmeniscus and the anterior horn (anterior fibers) of the lateral meniscus. The posterior horn attaches to the posterior intercondylar fossa between the attachments of the lateral meniscus and the posterior cruciate ligament (PCL). The medialmeniscus is continuously attached to the joint capsule along the entire periphery. The coronary ligament represents the tibial portion of this capsular attachment. At its midpoint, the medialmeniscus is firmly attached to the femur and tibia through a robust thickening in the capsule known as the deep medial collateral ligament [5].
The medial meniscus’ posterior horn is smaller (28.5 mm2) than the anterior horn (61.4 mm2) but has a more stable implantation area. The anterior horn has a variable implantation area on the tibial plateau and is more prone to avulsions than the posterior horn. The types of anterior horn attachment have been described by Berlet and Fowler [6]. In cadaveric studies it has been shown that the posterior horn of the medial meniscus can be attached to the PCL’s insertion while the anterior horn relates to the insertion of the ACL by means of an intermeniscal ligament or other soft tissues. The remaining large portion of the meniscus is attached to the joint capsule and the capsular ligaments. The body of the medial meniscus is also attached to the deep medial collateral ligament, which is a thickening of the medial capsular attachments that reaches from the tibia to the femur (Figs. 1.7 and 1.8).
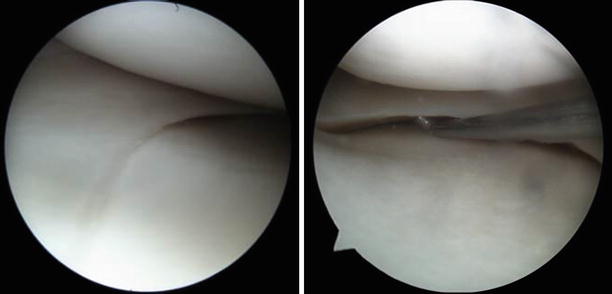
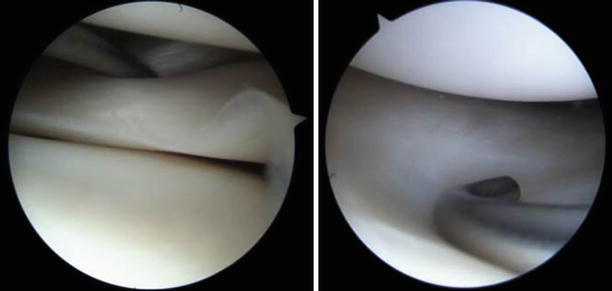
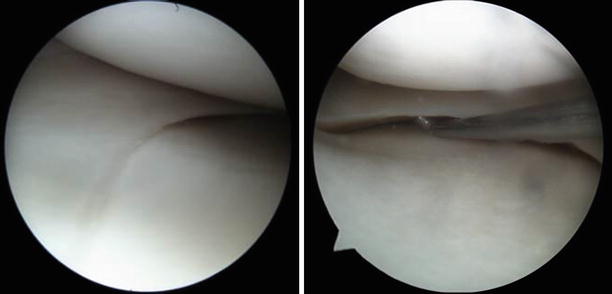
Fig. 1.7
Arthroscopic views of a normal medial meniscus through the antero medial and lateral portals respectively
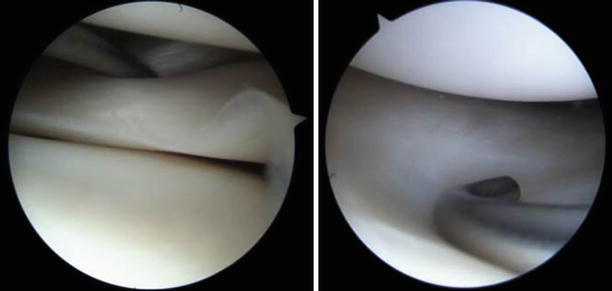
Fig. 1.8
View of a normal lateral meniscus. The physiological lack of capsular adherences can be noticed surrounding the intra-articular portion of the popliteal tendon. An anatomic variation of the lateral meniscus – discoid meniscus, checked for inconsistencies with a probe
1.2.1.2 Lateral Meniscus
The lateral meniscus covers a larger portion of the tibial surface than does the medialmeniscus. Its radius of curvature remains fairly constant, giving the lateral meniscus an almost circular appearance. The anterior horn is attached anterior to the intercondylar eminence, just posterior and lateral to the ACL attachment with which it partially blends. The posterior horn attaches posterior to the intercondylar eminence.
In 50 % of individuals, anterior fibers of the posterior enthesis extend to the lateral aspect of the medial femoral condyle, forming the anterior meniscofemoral ligament (ligament of Humphry). In 76 % of cases, the posterior fibers of the posterior horn cross posterior to the PCL and attach to the intercondylar fossa of the medial femoral condyle, forming the posterior meniscofemoral ligament (ligament of Wrisberg). The lateral meniscus has only a loose peripheral attachment to the capsule, which is interrupted by the popliteus tendon. Lateral meniscal variants, including the most recognized discoid meniscus, have a reported prevalence as high as 16.6 % [7].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








