Open Treatment of Medial and Lateral Epicondylitis
Patient Selection
Symptoms include pain, local tenderness, and limitations of activity.
Typically managed nonsurgically with rest and restriction
Surgical intervention is reserved for patients with persistent symptoms after 6 months of nonsurgical treatment
For lateral epicondylitis, must rule out:
Cervical radiculopathy
Radial tunnel syndrome
Posterolateral impingement
Posterolateral rotatory instability
Radiocapitellar arthrosis
For medial epicondylitis, must rule out:
Ulnar neuritis
Attenuation of the ulnar collateral ligament with instability
Flexor/pronator muscle ruptures
Preoperative Imaging
Lateral and medial epicondylitis are clinical diagnoses; use imaging to rule out other conditions
Plain radiographs can identify calcifications in 20% of patients
MRI can evaluate for intra-articular pathology, assess the collateral ligaments, or aid in determining the extent of tears in the extensor flexor or pronator origin; increased signal intensity on T2-weighted images may be seen in extensor carpi radialis brevis (ECRB) tendon origin or common flexor origin
Procedure
Room Setup/Patient Positioning
General anesthesia preferred provided patient comorbidities permit; regional anesthesia used if needed, but may not allow for postoperative neurologic examination
Supine position with surgical arm on arm board with tourniquet; hand and lower arm in stockinette
Special Instruments/Equipment/Implants
No special equipment required for open treatment of either condition
If a surgeon prefers to drill the epicondyle to stimulate a healing response, a 0.062-in Kirschner wire or a 5/64-in drill bit is needed
Surgical Technique
Lateral Epicondylitis
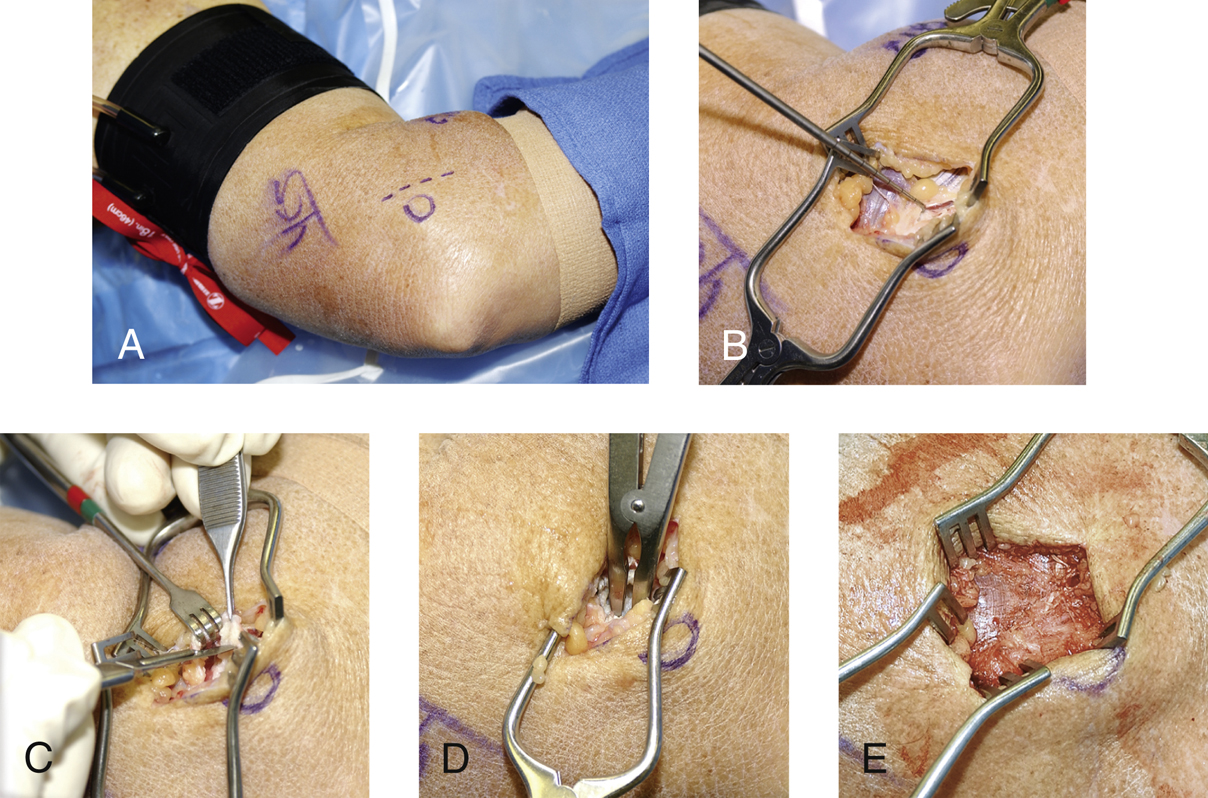
Figure 1Intraoperative photographs demonstrate open treatment of lateral epicondylitis. A, The planned incision is marked anteromedial to the palpable and outlined lateral epicondyle. B, The interface between the anterior extensor carpi radialis longus (ECRL) and the more posterior extensor digitorum communis (EDC) is identified and superficially split. C, The pathologic extensor carpi radialis brevis tendinosis tissue is resected en bloc with a scalpel. D, A rongeur is used to roughen the lateral condyle to create a healing response. E, The ECRL/EDC aponeurosis is repaired with a running No. 1 absorbable suture (not visible in this photograph). Débridement and closure of the extensor split is complete.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


