Open Reduction and Internal Fixation of Proximal Humerus Fractures
Mark T. Dillon
Stephen Torres
Mohit Gilotra
David L. Glaser
DEFINITION
Proximal humerus fractures may involve the surgical neck, the greater tuberosity, and/or the lesser tuberosity.
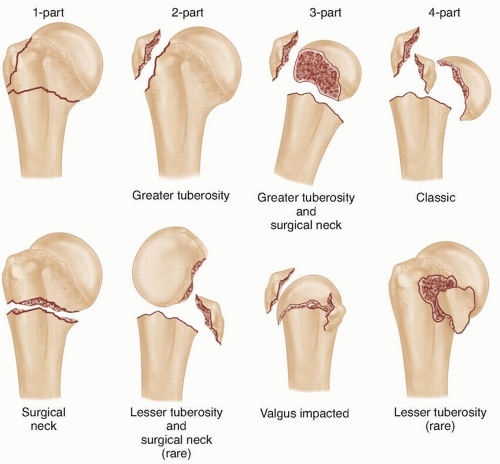
The Neer classification, which is most commonly used, categorizes fractures based on the number of displaced parts (FIG 1). This classification system involves four segments: the articular surface, the greater tuberosity, the lesser tuberosity, and the humeral shaft. Fracture fragments displaced 1 cm or angulated 45 degrees are considered a displaced part.22, 23
The AO/ASIF (Arbeitsgemeinschaft für Osteosynthesefragen-Association for the Study of Internal Fixation) broadly classifies fractures into three types: type 1, unifocal extra-articular; type 2, bifocal extra-articular; and type 3, intra-articular.
Each type is then further divided into groups and subgroups.21
This system places more emphasis on the vascular supply to the humerus, with intra-articular fracture patterns having the highest risk of avascular necrosis.31
Studies have demonstrated that interobserver reliability for both classification systems is not high.1, 28, 29
Although not included in Neer’s original classification, valgus impacted fractures are a unique entity that is important to recognize.
Four-part fractures in which the humeral articular surface is impacted on the shaft segment in a valgus position, leading to an increase in the angle between the humeral shaft and the articular surface
Often minimally displaced owing to an intact rotat or cuff5
Have a lower incidence of avascular necrosis because the blood supply to the head is less likely to be disrupted
ANATOMY
The osseous anatomy of the proximal humerus consists of the greater tuberosity, the lesser tuberosity, and the articular surface.
The subscapularis inserts onto the lesser tuberosity, whereas the supraspinatus, infraspinatus, and teres minor insert onto the greater tuberosity.
Knowledge of deforming forces associated with humerus fracture allows the surgeon to better treat proximal humerus fractures by both operative and nonoperative means.
In a two-part surgical neck fracture, the pectoralis major pulls the humeral shaft anteromedial.
In a two-part greater tuberosity fracture, the pull of the supraspinatus, infraspinatus, and teres minor tendons displaces the greater tuberosity superiorly and/or posteriorly.
With a three-part fracture involving the lesser tuberosity, the attachment site of these tendons into the greater tuberosity is intact, and the articular surface of the humeral head rotates externally to face anteriorly.
Three-part fractures involving the greater tuberosity result in unopposed subscapularis function, and the humeral articular surface rotates posteriorly.
Four-part fractures result in displacement of the shaft and both tuberosities, leaving a free head fragment with little soft tissue attachment.
An understanding of the vascular anatomy is crucial to treat fractures of the proximal humerus effectively and to predict potential risk of avascular necrosis.
The proximal humerus receives its blood supply from two branches of the axillary artery: the anterior and posterior circumflex humeral arteries.
Historically, the main blood supply to the humeral head has been thought to be the anterolateral ascending (arcuate) branch of the anterior circumflex artery10; however, there is new evidence to suggest the primary supply is from the posterior circumflex humeral artery.12
The arcuate branch runs just lateral to the tendon of the long head of the biceps in the bicipital groove, enters the humeral head, and becomes interosseous proximally at the transition between the bicipital groove and greater tuberosity and supplies the medial aspect of the humeral head.12
The posterior circumflex humeral artery branches from the axillary artery, travels through the quadrangular space with the axillary nerve, winds superolaterally around the posterior aspect of the humerus, and supplies the superior, lateral, and inferior aspects of the humeral head.12
The relationship of the arteries to the humerus is important when assessing risk of avascular necrosis as certain fracture patterns put these vessels at increased risk. Fractures with extension into the dorsomedial metaphysis and disruption of the medial calcar have significantly higher rates of ischemia then those that leave these areas intact.11
PATHOGENESIS
In older patients, proximal humerus fractures usually result from a ground-level, low-energy fall.
In contrast, younger patients sustain proximal humerus fractures as the result of higher energy mechanisms such as an automobile collision or a sports-related injury (eg, extreme sports).
The presence of an associated glenohumeral dislocation can also be present and must be determined at the time of initial evaluation.
PATIENT HISTORY AND PHYSICAL FINDINGS
History should include the mechanism of injury, social situation, and preexisting shoulder symptoms, which could indicate rotator cuff pathology or arthritis.
On presentation, patients with proximal humerus fractures complain of pain in the shoulder that is made worse with attempted movement.
Visual inspection can reveal ecchymosis and swelling of the arm and palpation generally elicits diffuse pain.
Assessment of the range of motion (ROM) may be difficult due to pain but is important to help determine the stability of the fracture. If the shaft and the proximal portion move as a unit when taken through internal and external rotation, the fracture usually is stable. If however, they do not and crepitus is felt, the fracture is unstable.
If there is an associated dislocation, it may be possible to palpate the humeral head as an anterior fullness.
A thorough neurovascular examination is performed to determine the presence of associated injuries.
Patients younger than 50 years are more prone to nerve injuries. One study demonstrated nerve injury, usually of the axillary nerve, in nearly 40% of patients in this age group who sustained shoulder dislocations or surgical neck fractures.2
Major vascular injury is very rare in these fractures; however, a high index of suspicion should be present when evaluating fractures with significant medial displacement. The axillary artery can be injured in these instances and diminished radial and ulnar pulses should alert the surgeon to this possibility.13
IMAGING AND OTHER DIAGNOSTIC STUDIES
Initial imaging studies consist of anteroposterior, scapular Y, and axillary views.
Additional views also may include internal and external rotation views if the fracture pattern is stable. Internal rotation views help to visualize the lesser tuberosity, whereas external rotation shows the greater tuberosity. West Point axillary view may be useful for fracture of the anterior glenoid rim and a Stryker notch view for a Hill-Sachs lesion.
Traction views also may prove helpful if tolerated by the patient.
A computed tomography (CT) scan may be helpful if radiographs do not demonstrate the fracture pattern adequately.
Studies have shown that the addition of a CT scan improves intraobserver reproducibility only minimally and does not affect interobserver reliability.1
However, CT scanning may prove valuable in determining the method of fixation as well as identifying associated injuries such as Hill-Sachs fractures and bony Bankart lesions.
Indications for magnetic resonance imaging (MRI) are limited, although it may prove useful if there is any concern regarding soft tissue injuries, including the glenoid labrum and rotator cuff.
DIFFERENTIAL DIAGNOSIS
Glenohumeral dislocation
Scapula fracture
Clavicle fracture
Humeral shaft fracture
Neurovascular injury
Neuropathic arthropathy
NONOPERATIVE MANAGEMENT
Historically, conservative treatment usually is recommended for fractures with less than 1 cm of displacement and 45 degrees of angulation.22 About 85% of proximal humerus fractures can be treated nonoperatively.20 With newer fixation devices, however, indications for surgical management have been expanded.
There is less tolerance for displacement in isolated greater tuberosity fractures. It has been suggested that more than 5 mm of displacement leads to poor functional results.19
Neer’s original description called for fixation of greater tuberosity fractures when there was more than 1 cm of displacement.22
Some authors believe that greater tuberosity displacement of greater than 5 mm may lead to impingement.
McLaughlin19 first suggested that patients in whom a greater tuberosity healed with residual displacement of more than 5 mm had long-standing pain with poor function. Displacement of less than 5 mm does not appear to warrant surgery.
Platzer et al26 looked at minimally displaced fractures of the greater tuberosity and found no statistical significance with varying degrees of displacement less than 5 mm.
For proximal humerus fractures not involving the humeral shaft, patients initially are immobilized in a simple sling.
When pain improves and the fracture moves as a unit, passive ROM is started. Patients begin with pendulum exercises, usually 2 to 3 weeks after injury, then progress to ROM in all planes.
Between 6 and 10 weeks, the fracture usually has healed enough that strengthening exercises may be started.18
When treating proximal humerus fractures conservatively, physical therapy is important to initiate as soon as possible. Koval et al15 showed significant improvement with onepart fractures when physical therapy was initiated before 2 weeks.
Several studies have shown that nonoperative management can lead to acceptable results with proximal humerus fractures.27, 30, 32
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree