Open Reduction and Internal Fixation of Fracture-Dislocations of the Elbow with Complex Instability
Niloofar Dehghan
Michael D. McKee
DEFINITION
Simple dislocations of the elbow can most often be treated successfully with closed means: reduction and short-term immobilization followed by early motion.
Fracture-dislocations of the elbow are more troublesome in that they often require operative intervention.
Fractures associated with elbow dislocations often involve the radial head and coronoid. An elbow dislocation associated with fractures of the radial head and coronoid is termed the terrible triad.
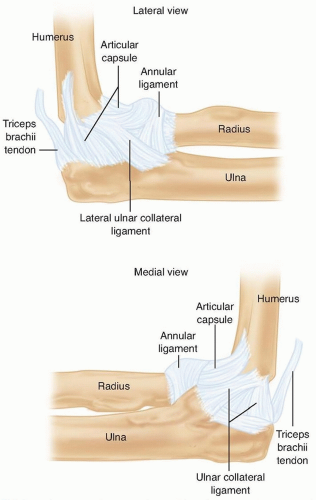
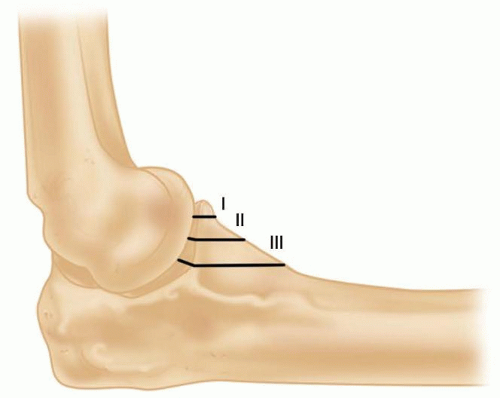
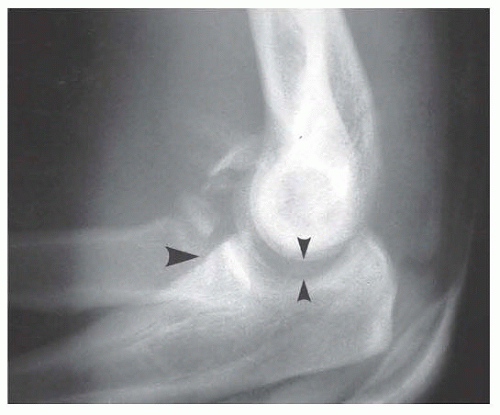
FIG 1 • The MCL and LCL complexes of the elbow. Note their points of attachment on the distal humerus and proximal ulna.
The principle of treating fracture-dislocations of the elbow is to provide sufficient stability through reconstruction of bony and ligamentous restraints such that early motion (within
2 weeks postoperatively) can be instituted without recurrent instability.
Failure to achieve this will result in either recurrent instability or severe stiffness after prolonged immobilization.
ANATOMY
Posterolateral dislocations of the elbow are associated with disruption of the medial collateral ligament (MCL) and lateral collateral ligament (LCL).
The MCL is the primary stabilizer to valgus stress (FIG 1).
The LCL is the primary stabilizer to posterolateral rotatory instability. Most often, the LCL disruption is proximally from the lateral epicondyle of the humerus, which creates a characteristic bare spot. Less commonly, the ligament may rupture midsubstance.7 Secondary restraints on the lateral side that may also be disrupted are the common extensor origin and the posterolateral capsule.
Radial head fractures have been classified by Mason:
Type I: small or marginal fracture with minimal displacement
Type II: marginal fracture with displacement
Type III: comminuted fractures of the head and neck5
Type IV: radial head fracture associated with elbow dislocation (Johnson modification)
Type I: tip fractures (not avulsions)
Type II: less than 50% of the coronoid
Type III: more than 50% of the coronoid
The insertion of the MCL is at the base of the coronoid and it may be involved in type III fractures.1
Anteromedial facet fractures of the coronoid are a different entity and are caused by a primary varus force.3
The medial facet is important for varus stability of the elbow, just distal to this is the sublime tubercle, the insertion point of MCL.
Anteromedial facet fractures may lead to varus posteromedial instability, and disruption of the LCL (from the varus force) is often seen. However, there is also potential for valgus instability if the fractured fragment is large enough to include the MCL insertion.
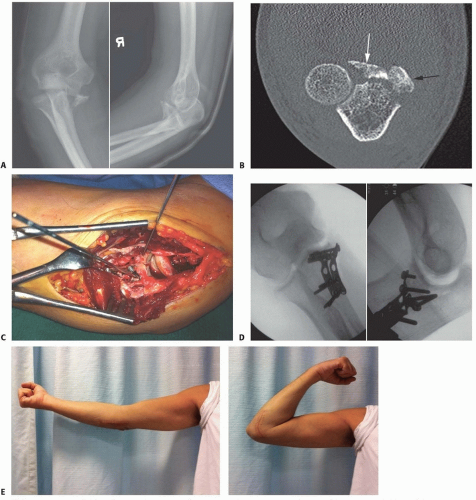
These fractures are unstable and in general are best treated with open reduction internal fixation with use of a medial plate in a buttress fashion (FIG 3).
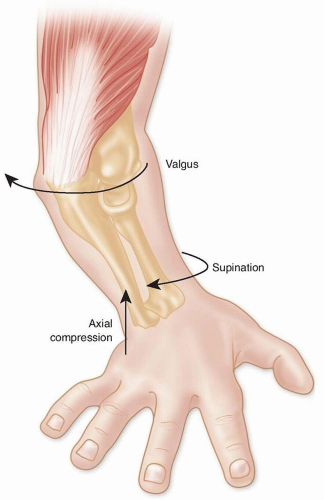
PATHOGENESIS
Fracture-dislocations of the elbow occur during falls onto an outstretched hand, falls from a height, motor vehicle accidents, or other high-energy trauma (FIG 4).
Typically, there is a hyperextension and valgus or varus stress applied to the pronated arm.
NATURAL HISTORY
Elbow dislocations with associated coronoid or radial head fractures have a poor natural history. These injuries are commonly treated with open reduction and surgical fixation, as redislocation or subluxation is likely with closed treatment.
Treatment of the radial head fracture by excision alone in the context of an elbow dislocation has a high rate of failure due to recurrent instability and should be avoided.
Problems of recurrent instability, arthrosis, and severe stiffness lead to poor functional results.12
PATIENT HISTORY AND PHYSICAL FINDINGS
Fracture-dislocations of the elbow are acute and traumatic, so the history should be straightforward.
It is not unusual for these injuries to occur with high-energy trauma, so a diligent search for other musculoskeletal and systemic injuries must accompany evaluation of the elbow. The ipsilateral shoulder and wrist should be evaluated.
The evaluation and documentation of peripheral nerve and vascular function in the injured extremity is critical and should be performed before and after reduction maneuvers.
IMAGING AND OTHER DIAGNOSTIC STUDIES
High-quality plain radiographs in the anteroposterior (AP) and lateral plane should be obtained before and after closed reduction.
Cast material can obscure bony detail after closed reduction.
If there is any evidence of forearm or wrist pain associated with the elbow injury, these should be imaged as well.
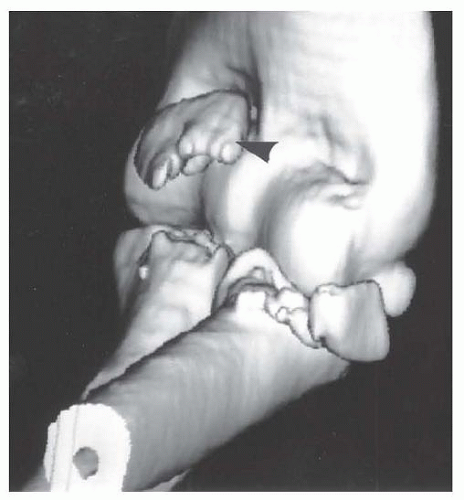
Computed tomography (CT) scans with reformatted images and three-dimensional (3-D) reconstructions are helpful in understanding the configuration of bony injuries (especially of the radial head and coronoid) and are helpful in treatment planning (FIG 5).
DIFFERENTIAL DIAGNOSIS
Radial head or neck fractures without associated dislocation
Coronoid fracture associated with posteromedial instability.
The radial head is not fractured, making diagnosis more difficult.
NONOPERATIVE MANAGEMENT
Initial treatment involves closed reduction and splinting with radiographs to confirm reduction (FIG 6).
If reduction cannot be maintained because of bone or soft tissue injury, repeated attempts at closed reduction should not be attempted. This is thought to contribute to the formation of heterotopic ossification.
In the setting of fracture-dislocation of the elbow with instability, the ability of nonoperative management to meet treatment goals is rare and surgery is indicated in almost all cases.
SURGICAL MANAGEMENT
The goals of surgery are to obtain and maintain a concentric and stable reduction of the ulnohumeral and radiocapitellar joint such that early motion within a flexion-extension arc of 30 to 130 degrees can be initiated. Early motion is key
(within 2 weeks postoperatively) to avoid elbow stiffness and resultant poor function.
Management of elbow dislocations with associated radial head and coronoid fractures should follow an established protocol (Table 1) that has produced reliable results.10
The radial head is an important secondary stabilizer of the elbow to valgus stress and posterior instability.9
It is also a longitudinal stabilizer of the forearm to proximal translation.
If fractured in this setting, it must be fixed or replaced, as radial head excision leads to recurrent instability and unacceptable results.12
Preoperative Planning
Before surgery, the surgeon must ensure that the proper equipment and implants are available.
Coronoid tip fractures are fixed with small fragment or cannulated screws of appropriate size. In the setting of small fragments (ie, type 1) that are not amendable to screw fixation, sutures through the anterior capsule around the fragment can be used instead. Large coronoid fragments such as anteromedial facet fragments should be fixed with a minifragment plate and screws in buttress fashion.
Table 1 Treatment Protocol for Elbow Dislocation with Associated Radial Head and Coronoid Fractures
Step
Action
1
Fix the coronoid fracture.
2
Fix or replace the radial head.
3
Repair the LCL.
4
Assess elbow stability within 30-130 degrees of flexion-extension with the forearm in full pronation.
5
If the elbow remains unstable, consider fixing the MCL.
6
Failing this, apply a hinged external fixator to maintain concentric reduction and allow for early motion.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree