Open Reduction and Internal Fixation of Clavicle Fractures
Introduction
Clavicle fractures account for 2.6% to 5% of adult fractures
Historically, nonsurgical management was standard, but with improved surgical techniques, growing evidence shows that surgical management may be beneficial in select patients
Classification
Clavicle fractures are classified based on their location and the degree of comminution and angulation
Allman classification system
Proximal (2% to 3%)
Midshaft (70% to 80%, high-energy, younger patient population)
Distal (21%)
Patient Selection
Indications
Open fracture
Floating shoulder
Impending skin necrosis
Associated neurovascular injuries
Multiply injured trauma patients
Improved outcomes associated with shortening greater than 15 to 20 mm, with 100% displacement, or with comminution
Contraindications
Nondisplaced or minimally displaced fractures in older, sicker patients
Low-demand patient or unfit to undergo surgery
If nonsurgical management pursued, use a sling and course of non–weight bearing
Preoperative Imaging
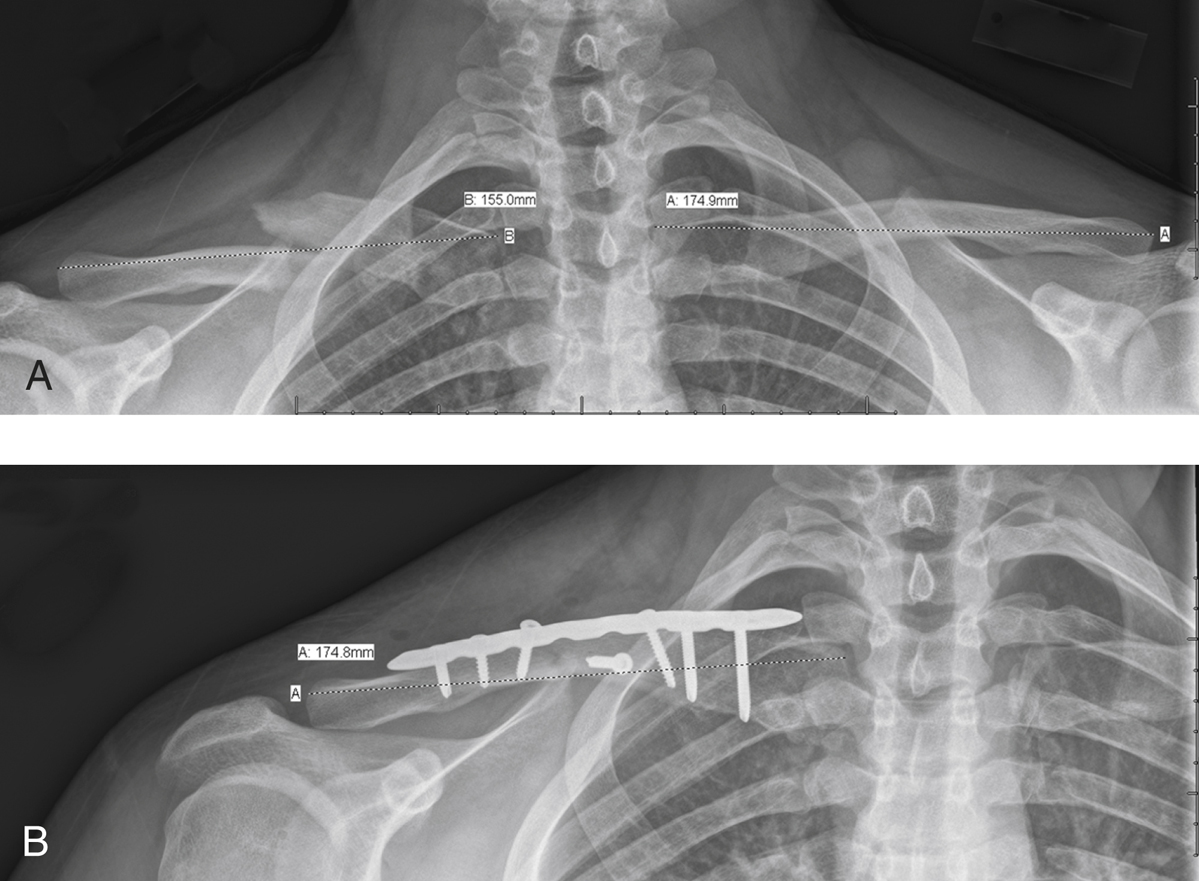
Figure 1AP radiographs of a patient with a right midshaft clavicle fracture. A, Preoperative radiograph demonstrates 2 cm of shortening. B, Postoperative radiograph shows that clavicle length symmetric to the uninjured left side is restored with plate fixation. An interfragmentary screw and a contoured clavicle fracture plate were used.
Orthogonal views of the clavicle
AP chest views (Figure 1) to rule out chest injury (eg, rib fractures, hemothorax, pneumothorax)
Apical oblique view—Shoulder tilted 45° anterior, and radiograph beam 20° cephalad
Abduction lordotic view—X-ray directed 25° cephalad with shoulder abducted above 135°; useful to assess healing postoperatively
Preoperative CT can help to evaluate nonunion and medial fractures extending to the sternoclavicular joint
Procedure for Midshaft Clavicle Fracture
Room Setup/Patient Positioning

Figure 2Photograph shows a patient with a pneumatically controlled arm positioner in place for left shoulder surgery.
Supine or modified beach-chair position on radiolucent table with intraoperative fluoroscopy available
Bump placed at medial portion of scapula
Arm in pneumatic arm positioner (Figure 2)
Palpate and mark the acromion borders, coracoid, triangular soft spot in acromion; acromioclavicular (AC) joint is anterior to soft spot and lateral to coracoid; palpate S-shaped clavicle
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


