Open Reduction and Internal Fixation of Calcaneal Fractures
Patient Selection
Indications
Calcaneus fractures occur from high-energy trauma; result in complex three-dimensional patterns
Position of foot at impact, extent of force, and bone quality influence fracture pattern, comminution
Surgical management indicated for displaced intra-articular fractures involving posterior facet
Contraindications
Use nonsurgical management for patients with nondisplaced intra-articular fractures, severe peripheral vascular disease, type I diabetes, and severe medical comorbidities, and for elderly patients who are minimal ambulators
Manage fractures with associated severe blistering, edema, or large open wounds later as calcaneal malunion
Preoperative Imaging
Plain Radiography
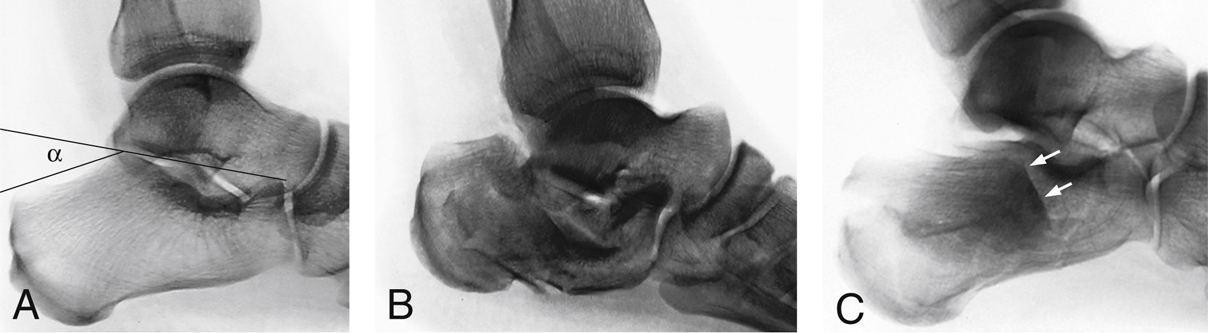
Figure 1Lateral hindfoot radiographs demonstrate radiographic signs used to assess for a calcaneal fracture. A, A normal tuber angle of Böhler (angle α) is seen in this uninjured foot. B, View of a calcaneal fracture demonstrates a decreased angle of Böhler. Also note the marked loss of calcaneal height with relative horizontalization of the talus. C, View of a calcaneal fracture shows impaction of the superolateral fragment, which manifests as a double-density sign (arrows).
AP foot, lateral hindfoot, Harris heel view, mortise ankle views
Calcaneus fractures most easily identified on lateral view of hindfoot (Figure 1)
Loss of height in posterior facet seen with intra-articular fracture
Decreased Böhler angle, increased crucial angle of Gissane seen in fractures separating posterior facet from sustentaculum and depressed
Harris heel view shows loss of calcaneal height, increased width, varus angulation of tuberosity fragment
Computed Tomography
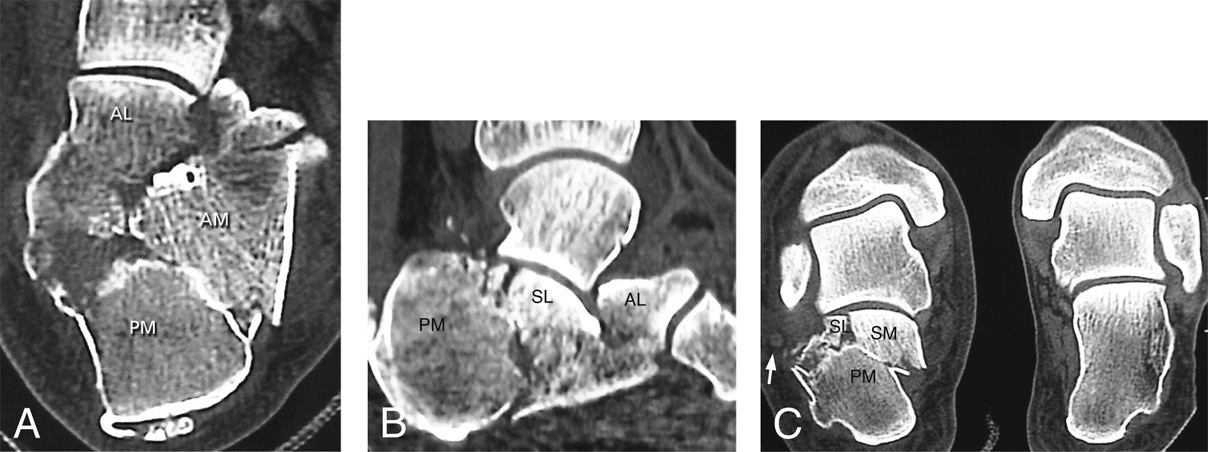
Figure 2Axial (A), sagittal (B), and semicoronal (C) CT images delineate typical calcaneal fracture fragments. In the semicoronal image of the injured side (left image of C), note the potential impingement of the expanded lateral wall against the peroneal tendons (arrow). AL = anterolateral, AM = anterior main, PM = posterior main, SL = superolateral, SM = superomedial.
Indicated if plain radiographs reveal intra-articular extension of calcaneal fracture (Figure 2)
Coronal and sagittal reformats help characterize fracture pattern, displacement, joint depression
Preoperative planning, review of radiographs, and CT are essential
Pathoanatomy
In displaced intra-articular calcaneal fracture, loss of calcaneal height results in shortened, widened heel with varus tuberosity malalignment
This height loss leads to decreased Böhler angle, ultimate loss of ankle dorsiflexion (Figure 1)
As superolateral fragment is impacted plantarward, lateral wall explodes laterally; may trap peroneal tendons against lateral malleolus, limiting subtalar motion
Anterior process displaces superiorly, limiting subtalar motion by impinging against lateral process of talus
Procedure
Resolution of Soft-Tissue Swelling
Perform surgery within first 3 weeks after injury, before consolidation but following resolution of soft-tissue swelling
Initial splint immobilization and limb elevation, later transitioning to compression stocking and fracture boot
Full resolution of edema demonstrated by wrinkle test
Room Setup/Patient Positioning

Figure 3Illustration shows intraoperative positioning for the extensile lateral approach for open reduction and internal fixation of a calcaneal fracture. Note the scissor positioning of the surgical and nonsurgical limbs and the operating platform, which facilitate intraoperative fluoroscopy.
For isolated injuries, lateral decubitus position on beanbag; for bilateral injuries, prone position
Scissor legs; flex surgical limb at knee, angle toward distal, posterior corner of table
Adequately pad contralateral limb; create “platform” with blankets, foam for surgical limb (Figure 3)
Special Instruments/Equipment/Implants
Dental picks, freer elevators, sharp and blunt periosteal elevators, Schanz pins, lamina spreaders
Low-profile, anatomic plates with locking and nonlocking options are available

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


