Chapter 4 Open fractures
internal fixation
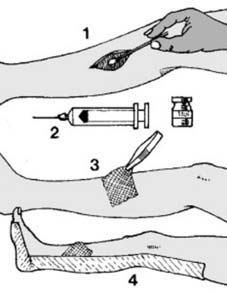
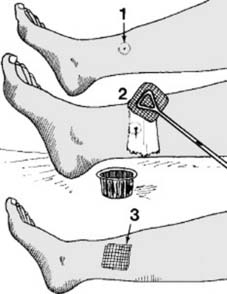
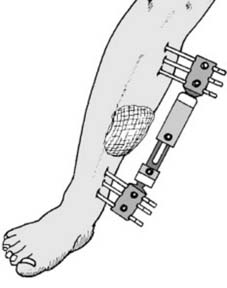
1 Open fractures: immediate care: When the case first presents, ensure that the following procedures are carried out in every case: (1) Take a bacteriology swab from the wound. (2) Commence a short course of appropriate antibiotics (see p. 50). (3) Cover the wound with care, using sterile dressings (to reduce the risks of secondary (hospital) infection). (4) Apply temporary splintage (e.g. a plaster back shell, or if appropriate, an inflatable splint).
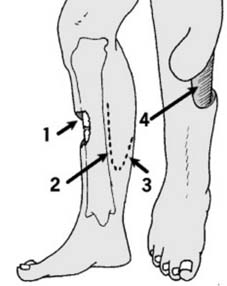
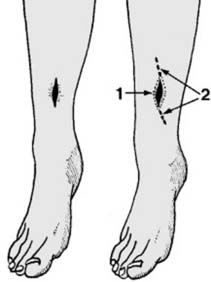
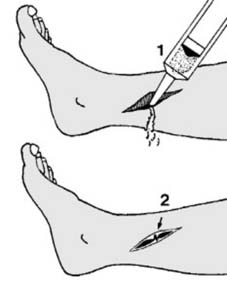
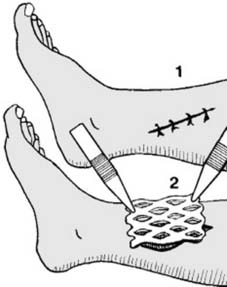
7 Type III ctd: If bone is exposed, the aim should be to get it covered within 5 days, to reduce the risks of secondary infection, and the initial application of a negative pressure dressing is usually advised. Split skin grafts will only survive if applied to a vascular bed, so that they cannot be used over open joints, bone devoid of periosteum, and tendons without paratenon. Thought must be given to future access (e.g. for bone grafting should union fail). In these circumstances other methods of cover must be employed. These should only be undertaken by a surgeon experienced in plastic surgical techniques, and consultation with a plastic surgeon prior to the initial procedure, with later transfer to a Plastic Surgical Unit is highly desirable.
8. Type III ctd: Other plastic surgical techniques include the following:
11 PRINCIPLES OF INTERNAL FIXATION AND COMMON FIXATION METHODS
When it is intended to implant materials for the treatment of fractures, the following criteria must be satisfied:
Fixation devices and systems
Fractures vary enormously in pattern; bones vary in their size, texture and strength. To cope with even the most common situations and be a match for every subtle variation of circumstance requires an impressive range of devices and instruments for their insertion. The design of fixation devices has in the past been somewhat haphazard, and aimed at the treatment either of one fracture or the solution of a single fixation problem. There have been attempts to produce integrated systems of fracture fixation: sets of devices which can contend with any fracture situation. The most outstanding system, now firmly established, is that developed by the Association for the Study of Internal Fixation [ASIF or AO (Arbeitgemeinschaft für Osteosynthesefragen)]. (This group of general and orthopaedic surgeons was founded in 1956 by Maurice E. Müller to research certain concepts propounded by Robert Danis.) As a result of their work, apart from the development of a series of screws, plates and other devices, and the corresponding instrumentation, the Association is responsible for some change in emphasis in the philosophy of fracture treatment. They feel that the common aim, a return to full function in the shortest time, can often best be achieved by the use of internal fixation devices, of such strength and design that external splintage can frequently be discarded permitting immediate joint freedom, early weight bearing, short-term hospitalisation, and early return to work and other activities. These ideals are often achieved, but it must be stressed that optimum results cannot be obtained without the necessary technical knowledge of the system and a degree of mechanical aptitude, both of which can be acquired by appropriate training and experience.
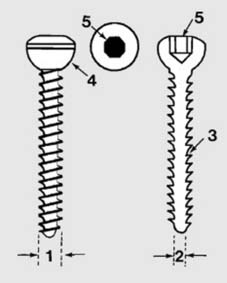
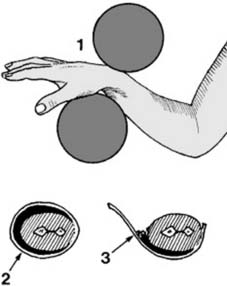
12 Principles of internal fixation and common devices: Cortical bone screws (a): The AO cortical bone screw enjoys widespread use and is probably the commonest of all internal fixation devices. The standard screw has an outside diameter of 4.5 mm (1) and a core diameter of 3.0 mm (2). The thread form is a modified buttress (3), of 1.75 mm pitch (circa 15 TPI). The large head has a hemispherical undersurface (4) and contains a hexagon socket (5) which is used for its insertion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree