As our understanding of the pathoanatomy of glenohumeral instability has improved, surgical techniques for the treatment of anterior instability have progressed. Many stabilization procedures are now successfully performed arthroscopically; open capsular shift, however, continues to play an important role in the management of instability in certain patients, providing an accurate and selective means of capsular plication. When performed with proper surgical technique, shoulder range of motion can be preserved with low recurrence rates and high subjective satisfaction, making the open capsular shift a durable and effective option in the modern management of shoulder instability.
Open shoulder stabilization is a proven means of preventing recurrent instability, reliably restoring function and quality of life to near preinjury levels. Although open repair has produced consistently favorable results, arthroscopic management has recently gained popularity as techniques have evolved and surgeons have acquired increased experience. Most instability surgery can now be successfully performed with an arthroscopic approach, and recent results have been comparable to historic treatment with open capsulolabral repair. In spite of these advances in arthroscopic technique, there is still an essential role for open capsular shift in the management of anterior instability; the choice of surgical treatment should therefore be based on surgeon experience and individual patient pathology. The goal of this article is to review the indications, technique, and clinical results of open capsular shift, specifically addressing the cases in which open stabilization shift remains the treatment of choice.
Rationale for repair
The rationale for open shoulder stabilization is based on knowledge of the pathoanatomy associated with anterior instability. Advances in our understanding of shoulder anatomy and biomechanics have led to improvements in procedure selection, as well as an evolution in the techniques used for stabilization.
Historically, the essential lesion of shoulder instability was described as an avulsion of the anterior-inferior glenoid labrum. Recurrent instability has since been attributed to concomitant capsular deformation at the time of dislocation. In fact, biomechanical studies have demonstrated that complete dislocation cannot occur after the creation of a Bankart lesion unless capsular disruption is also present. It is now recognized that the primary pathology of instability encompasses labral detachment, along with a capsular abnormality, which may include macroscopic capsular rupture, capsular deformation or stretch, capsular redundancy or laxity, periosteal capsular stripping, or any combination of these. Subsequent to the primary capsulolabral disruption, there is loss of tension on the glenohumeral ligaments with resultant instability.
The goal of any surgical stabilization procedure is to address the specific pathology of a patient with recurrent subluxation or dislocation. Surgical intervention is therefore aimed at addressing the labral avulsion, as well as the exact type of capsular abnormality present. When these two primary pathologic features of instability are not addressed, higher rates of failure have been reported. Failure to address capsular laxity has also been suggested as a potential explanation for the higher reported recurrence rates after arthroscopic stabilization. Open capsular shift effectively addresses both labral disruption and capsular abnormalities, restoring the native static stabilizers of the shoulder joint.
Indications
Surgical intervention is generally recommended for those patients who continue to experience pain or instability in spite of adequate nonoperative treatment. More specifically, the choice of stabilization procedure should be based on the pathology of the patient, the preferences of the patient, and the experience of the surgeon. Patient history and activity or sport requirements are also important considerations in the selection of surgical approach. There is significant overlap between the relative indications for open and arthroscopic stabilization and, therefore, the choice of approach must be individualized. In many cases, both arthroscopic and open repair can be successful, as long as (1) both labral injury and capsular disruption are addressed, and (2) surgeon technical expertise allows for either.
Arthroscopic instability treatment has recently gained popularity, as it is minimally invasive, avoids release of the subscapularis, poses limited morbidity to the patient, and provides an improved ability to identify and treat associated pathologic conditions. Most indications for arthroscopic stabilization, however, are relative and not absolute. Ideal candidates have a history of traumatic instability with a documented labral or capsular detachment, without significant capsular laxity or deficiency. Arthroscopic management is also indicated in patients who wish to avoid the increased morbidity of open stabilization, and is relatively indicated in patients with concomitant intra-articular abnormalities. In high-performance overhead athletes, arthroscopic management may offer a faster return to activity and decreased loss of external rotation. Recent literature has presented conflicting evidence on postoperative range of motion following instability repair; some reports have demonstrated equivalent external rotation after open and arthroscopic treatment, making this indication somewhat controversial.
In spite of advances in the arthroscopic management of instability, numerous relative contraindications exist. Among these are humeral avulsions of the glenohumeral ligaments (HAGL), capsular ruptures, revision stabilization procedures in which capsular deficiency is a concern, and prior failed thermal capsulorrhaphy procedures. Generally speaking, arthroscopic treatment is relatively contraindicated in all cases in which there is concern for severely compromised tissue quality. More importantly, it is absolutely contraindicated if the surgeon does not have the expertise or advanced equipment necessary for this technically demanding procedure. The surgeon should always be prepared to convert an arthroscopic procedure to a traditional open capsular shift if deemed necessary to treat the specific pathology, and reduce the risk for postoperative recurrence of instability.
Although arthroscopic repair may enable faster recovery and avoid the morbidity of open surgery, open capsular shift remains effective in treating a wide spectrum of symptomatic instability patients. Furthermore, it may be specifically indicated over arthroscopic treatment in certain patient populations. Open treatment is generally indicated for revision of failed prior open or arthroscopic stabilization procedures, cases of significant glenoid or humeral bone loss, capsular deficiency or midsubstance rupture, and chronic irreparable deficiency of the rotator cuff, specifically the subscapularis. It is absolutely indicated in irreducible or open dislocations, and in cases when arthroscopic techniques cannot appropriately address the pathology present. Atraumatic and multidirectional instability present another compelling indication for open capsular shift, with favorable subjective and objective results demonstrated at mid- and long-term follow-up. With few exceptions, open surgery is also relatively indicated for humeral avulsions of the glenohumeral ligaments.
Recently, Balg and Boileau investigated the risk factors for redislocation after arthroscopic repair, in an attempt to develop a simple method for identifying patients who would be better served by open stabilization. The investigators identified 131 consecutive patients who underwent arthroscopic treatment for recurrent anterior instability with suture anchors. Risk factors for postoperative instability included: age less than 20 at the time of surgery, involvement in competitive or contact sport, shoulder hyperlaxity, and bony defects of the humerus or glenoid. Each of these factors should be carefully considered during preoperative evaluation and procedure selection.
Some advocate the selection of open repair based on specific findings at the time of surgery, after examination under anesthesia and assessment of the pathology present during diagnostic arthroscopy. The presence of marked anterior or multidirectional laxity on physical examination, or the absence of a discrete Bankart lesion and well-defined inferior glenohumeral ligament (IGHL), are thought to make arthroscopic management less advisable. Cole and colleagues reported the results of 63 surgical patients with traumatic anterior instability, in whom the decision on arthroscopic Bankart repair versus open capsular shift made after examination under anesthesia and diagnostic arthroscopy. Thirty-nine patients had pure anterior translation with a discrete Bankart lesion; 24 had anterior and inferior translation, along with capsular laxity seen at the time of arthroscopy. The former group was managed with arthroscopic Bankart repair, while the latter was managed with open anterior-inferior capsular shift. At a mean of 54 months postoperatively, there were no significant differences between the groups in Rowe, American Shoulder and Elbow Surgeons (ASES), or SF-36 scores. With the exception of a slight loss of forward elevation in the capsular shift group, measured losses in range of motion between the groups were minimal. Overall, 75% of the patients in each group returned to their preinjury activity levels with minimal or no limitations. The investigators concluded that favorable results can be achieved if the choice of surgical management is made based on the pathologic findings present at the time of surgery.
Patients with attenuated anterior ligamentous structures are ideal candidates for open stabilization; this severe capsular deficiency is often seen in a revision setting following previous failed open or arthroscopic repair. Tauber and colleagues performed a retrospective review of 41 patients with recurrent instability, highlighting the indication for open treatment in revision instability repair. At the time of revision surgery, a bony defect was present in 56% of patients, an enlarged or overstretched capsule in 22%, and a laterally torn capsule in 5%. Each of these pathologic findings has not traditionally been considered as amenable to arthroscopic management. Furthermore, only 17% of patients had typical Bankart lesions with good capsular tissue quality that might otherwise be considered for arthroscopic repair. In the revision setting, open treatment may better address the capsular insufficiency, or multiple causes of instability in these complex individuals.
It has been suggested that all patients who require absolute stability, or those who present an excessively high risk for postoperative dislocation, are indicated for open stabilization. Recently, this indication has become more controversial. Some argue that collision athletes present a clear indication for open surgery, given the favorable results and minimal recurrence rates shown in the literature. Others contend that with good patient selection and modern surgical techniques, arthroscopic treatment can offer similar results.
Cho and colleagues compared the results of arthroscopic stabilization in 29 collision and noncollision athletes, finding that arthroscopic treatment reliably restored shoulder function and range of motion, with consistent return to sports activity. An overall 17.2% rate of recurrent instability was reported, however, with five patients (28.6%) in the collision group versus one patient (6.7%) in the noncollision group. More recently, Rhee and colleagues compared open and arthroscopic stabilization in 48 shoulders of 46 collision athletes, 16 who underwent arthroscopic stabilization and 32 with open repairs. At a mean follow-up of 72 months, visual analog scale (VAS), Rowe, and Constant scores improved in all patients, with no significant difference in scores between the two repair groups. There was, however, a 25% rate of recurrent instability in the arthroscopic group, compared with a 12.5% rate in the open group. Given the higher failure rate after arthroscopic repair, the investigators concluded that open stabilization was a more reliable method for the management of anterior shoulder instability in collision athletes.
Indications
Surgical intervention is generally recommended for those patients who continue to experience pain or instability in spite of adequate nonoperative treatment. More specifically, the choice of stabilization procedure should be based on the pathology of the patient, the preferences of the patient, and the experience of the surgeon. Patient history and activity or sport requirements are also important considerations in the selection of surgical approach. There is significant overlap between the relative indications for open and arthroscopic stabilization and, therefore, the choice of approach must be individualized. In many cases, both arthroscopic and open repair can be successful, as long as (1) both labral injury and capsular disruption are addressed, and (2) surgeon technical expertise allows for either.
Arthroscopic instability treatment has recently gained popularity, as it is minimally invasive, avoids release of the subscapularis, poses limited morbidity to the patient, and provides an improved ability to identify and treat associated pathologic conditions. Most indications for arthroscopic stabilization, however, are relative and not absolute. Ideal candidates have a history of traumatic instability with a documented labral or capsular detachment, without significant capsular laxity or deficiency. Arthroscopic management is also indicated in patients who wish to avoid the increased morbidity of open stabilization, and is relatively indicated in patients with concomitant intra-articular abnormalities. In high-performance overhead athletes, arthroscopic management may offer a faster return to activity and decreased loss of external rotation. Recent literature has presented conflicting evidence on postoperative range of motion following instability repair; some reports have demonstrated equivalent external rotation after open and arthroscopic treatment, making this indication somewhat controversial.
In spite of advances in the arthroscopic management of instability, numerous relative contraindications exist. Among these are humeral avulsions of the glenohumeral ligaments (HAGL), capsular ruptures, revision stabilization procedures in which capsular deficiency is a concern, and prior failed thermal capsulorrhaphy procedures. Generally speaking, arthroscopic treatment is relatively contraindicated in all cases in which there is concern for severely compromised tissue quality. More importantly, it is absolutely contraindicated if the surgeon does not have the expertise or advanced equipment necessary for this technically demanding procedure. The surgeon should always be prepared to convert an arthroscopic procedure to a traditional open capsular shift if deemed necessary to treat the specific pathology, and reduce the risk for postoperative recurrence of instability.
Although arthroscopic repair may enable faster recovery and avoid the morbidity of open surgery, open capsular shift remains effective in treating a wide spectrum of symptomatic instability patients. Furthermore, it may be specifically indicated over arthroscopic treatment in certain patient populations. Open treatment is generally indicated for revision of failed prior open or arthroscopic stabilization procedures, cases of significant glenoid or humeral bone loss, capsular deficiency or midsubstance rupture, and chronic irreparable deficiency of the rotator cuff, specifically the subscapularis. It is absolutely indicated in irreducible or open dislocations, and in cases when arthroscopic techniques cannot appropriately address the pathology present. Atraumatic and multidirectional instability present another compelling indication for open capsular shift, with favorable subjective and objective results demonstrated at mid- and long-term follow-up. With few exceptions, open surgery is also relatively indicated for humeral avulsions of the glenohumeral ligaments.
Recently, Balg and Boileau investigated the risk factors for redislocation after arthroscopic repair, in an attempt to develop a simple method for identifying patients who would be better served by open stabilization. The investigators identified 131 consecutive patients who underwent arthroscopic treatment for recurrent anterior instability with suture anchors. Risk factors for postoperative instability included: age less than 20 at the time of surgery, involvement in competitive or contact sport, shoulder hyperlaxity, and bony defects of the humerus or glenoid. Each of these factors should be carefully considered during preoperative evaluation and procedure selection.
Some advocate the selection of open repair based on specific findings at the time of surgery, after examination under anesthesia and assessment of the pathology present during diagnostic arthroscopy. The presence of marked anterior or multidirectional laxity on physical examination, or the absence of a discrete Bankart lesion and well-defined inferior glenohumeral ligament (IGHL), are thought to make arthroscopic management less advisable. Cole and colleagues reported the results of 63 surgical patients with traumatic anterior instability, in whom the decision on arthroscopic Bankart repair versus open capsular shift made after examination under anesthesia and diagnostic arthroscopy. Thirty-nine patients had pure anterior translation with a discrete Bankart lesion; 24 had anterior and inferior translation, along with capsular laxity seen at the time of arthroscopy. The former group was managed with arthroscopic Bankart repair, while the latter was managed with open anterior-inferior capsular shift. At a mean of 54 months postoperatively, there were no significant differences between the groups in Rowe, American Shoulder and Elbow Surgeons (ASES), or SF-36 scores. With the exception of a slight loss of forward elevation in the capsular shift group, measured losses in range of motion between the groups were minimal. Overall, 75% of the patients in each group returned to their preinjury activity levels with minimal or no limitations. The investigators concluded that favorable results can be achieved if the choice of surgical management is made based on the pathologic findings present at the time of surgery.
Patients with attenuated anterior ligamentous structures are ideal candidates for open stabilization; this severe capsular deficiency is often seen in a revision setting following previous failed open or arthroscopic repair. Tauber and colleagues performed a retrospective review of 41 patients with recurrent instability, highlighting the indication for open treatment in revision instability repair. At the time of revision surgery, a bony defect was present in 56% of patients, an enlarged or overstretched capsule in 22%, and a laterally torn capsule in 5%. Each of these pathologic findings has not traditionally been considered as amenable to arthroscopic management. Furthermore, only 17% of patients had typical Bankart lesions with good capsular tissue quality that might otherwise be considered for arthroscopic repair. In the revision setting, open treatment may better address the capsular insufficiency, or multiple causes of instability in these complex individuals.
It has been suggested that all patients who require absolute stability, or those who present an excessively high risk for postoperative dislocation, are indicated for open stabilization. Recently, this indication has become more controversial. Some argue that collision athletes present a clear indication for open surgery, given the favorable results and minimal recurrence rates shown in the literature. Others contend that with good patient selection and modern surgical techniques, arthroscopic treatment can offer similar results.
Cho and colleagues compared the results of arthroscopic stabilization in 29 collision and noncollision athletes, finding that arthroscopic treatment reliably restored shoulder function and range of motion, with consistent return to sports activity. An overall 17.2% rate of recurrent instability was reported, however, with five patients (28.6%) in the collision group versus one patient (6.7%) in the noncollision group. More recently, Rhee and colleagues compared open and arthroscopic stabilization in 48 shoulders of 46 collision athletes, 16 who underwent arthroscopic stabilization and 32 with open repairs. At a mean follow-up of 72 months, visual analog scale (VAS), Rowe, and Constant scores improved in all patients, with no significant difference in scores between the two repair groups. There was, however, a 25% rate of recurrent instability in the arthroscopic group, compared with a 12.5% rate in the open group. Given the higher failure rate after arthroscopic repair, the investigators concluded that open stabilization was a more reliable method for the management of anterior shoulder instability in collision athletes.
Open capsular shift
Historically, Rowe and colleagues popularized the classic Bankart repair as an anatomic technique of restoring shoulder stability. Results were excellent, with only a 3.5% recurrence rate over 30 years. Later, the open capsular shift was proposed by Neer and Foster as a treatment for multidirectional instability. The procedure was designed to reduce capsular volume and subsequently restore tension in the glenohumeral ligaments, through a superior shift of the inferior capsule. The procedure allows the surgeon to adjust the degree of shift depending on the direction and extent of capsular laxity. Most modern techniques for the management of instability are modifications of previously described procedures, involving a combination of Bankart repair and capsular shift, with a selective determination of ligamentous tension. The concept of a selective shift is based on an understanding that the capsuloligamentous structures of the shoulder act predictably as checkreins to translation based on arm position. Selective restoration of ligamentous tension is, therefore, able to restrict anterior and inferior translation in a position of apprehension.
The anterior-inferior capsular shift uses a T-capsulorrhaphy to decrease the volume of the joint capsule, thereby restoring tension on the glenohumeral ligaments. The decreased capsular volume increases responsiveness of the intra-articular pressure to downward loading, decreasing the amount of inferior displacement expected with any given load. The shift allows tightening of the capsule in two directions, both superior-inferior and medial-lateral. To preserve external rotation, however, over-tightening in the medial-lateral direction must be avoided. A careful titration of the shift will stabilize the joint without compromising external rotation and maximum forward elevation, thus avoiding overconstraint.
The technique for capsular shift presented in this article is favored by the senior author because of its anatomic reattachment of the displaced labrum, in addition to a capsular plication. The key pathologic elements of instability are addressed with this procedure, enabling an effective correction of most forms of anterior and multidirectional instability.
Surgical Technique
The procedure is performed with the patient in a modified beach chair position, with the head of the bed elevated to 30°. Through an axillary incision, the deltopectoral interval is identified. The cephalic vein is preserved and retracted laterally with the deltoid. If needed to obtain additional inferior exposure, the upper 0.5 to 1 cm of the pectoralis major insertion can be released and tagged for later repair. Superiorly the coracoid is identified, and the clavipectoral fascia is incised just lateral to the strap muscles. Deep retractors are placed, taking care to avoid injury to the musculocutaneous nerve. For improved superior exposure, a small crescent of the coracoacromial ligament can be excised at its anterolateral edge.
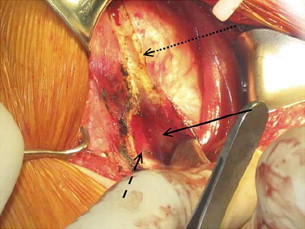
A complete anterior bursectomy is performed to expose the subscapularis muscle and its borders. The tendon is then incised 1 cm medial to its insertion onto the lesser tuberosity. The subscapularis is detached from the underlying joint capsule, which can be technically difficult owing to attachments between the capsule and tendon at its superior border. The plane between muscle and capsule should therefore be identified inferiorly by blunt dissection ( Fig. 1 ). Working from inferior to superior, an elevator and Mayo scissors can be used to tease the muscle from the capsule. During this dissection, the axillary nerve should be identified and protected; adduction and external rotation of the arm will move the nerve farther from the site of dissection. The subscapularis is tagged for later repair.