Traumatic anterior shoulder dislocations are the most frequent type of joint dislocation and affect approximately 1.7% of the general population. The literature supports the consideration of primary stabilization in high-risk patients because of reported recurrences as high as 80% to 90% with nonoperative treatment regimens. Successful stabilization of anterior glenohumeral instability relies on not only good surgical techniques but also careful patient selection. Failure rates after open and arthroscopic stabilization have been reported to range from 2% to 8% and 4% to 13%, respectively. Recurrent shoulder instability leads to increased morbidity to the patient, increased pain, decreased activity level, prolonged time away from work and sports, and a general decrease in quality of life. This article reviews the potential pitfalls in anterior shoulder stabilization and discusses appropriate methods of addressing them in revision surgery.
Traumatic anterior shoulder dislocations are the most frequent type of joint dislocation and affect approximately 1.7% of the general population. The literature supports the consideration of primary stabilization in high-risk patients because of reported recurrences as high as 80% to 90% with nonoperative treatment regimens. Successful stabilization of anterior glenohumeral instability relies on not only good surgical techniques but also careful patient selection. Failure rates after open and arthroscopic stabilization have been reported to range from 2% to 8% and 4% to 13%, respectively. Recurrent shoulder instability leads to increased morbidity to the patient, increased pain, decreased activity level, prolonged time away from work and sports, and a general decrease in quality of life. This article reviews the potential pitfalls in anterior shoulder stabilization and discusses appropriate methods of addressing them in revision surgery.
Pathoanatomy
The stability of the glenohumeral joint relies on the balance maintained by its static and dynamic stabilizers. Dynamic components include the rotator cuff muscles, and the critical static components include the glenolabral complex and capsuloligamentous structures. The labrum increases the surface area and depth of the glenoid socket by as much as 50%, thereby improving osseous conformity. Detachment of the anteroinferior labrum with its attached inferior glenohumeral ligament complex denotes the classic Bankart lesion and is the most common pathologic finding associated with anterior shoulder instability. With recurrent episodes of instability, elongation of the anteroinferior and inferior capsule has been shown to occur, further adding to the underlying pathology of this clinical entity.
In addition to soft tissue injury, recurrent instability can facilitate progressive bony injury. Sugaya and colleagues identified an osseous Bankart lesion in 50% of patients with traumatic anterior shoulder instability. Although most of these fragments were less than 10.6% of the glenoid fossa, they also noted that an additional 40% of patients showed blunting on oblique radiographs, suggestive of mild erosion. Griffith and colleagues reported similar results, with a 41% incidence of glenoid bone loss in first-time anterior shoulder dislocators. This condition increased to 86% in recurrent dislocators, and the severity of the bone defect significantly correlated to the number of dislocations.
The clinical applicability of these findings was characterized by Itoi and colleagues, who elucidated the minimum sized defect that led to clinical instability after a Bankart repair. In a cadaveric study they showed that after a Bankart repair, the capsular structures maintained stability of the joint up to a 21% (6.8 mm) anteroinferior glenoid defect. With bony defects greater than 21%, the shoulder showed persistent instability with internal rotation, and experienced limited external rotation after Bankart repair ( Fig. 1 ).
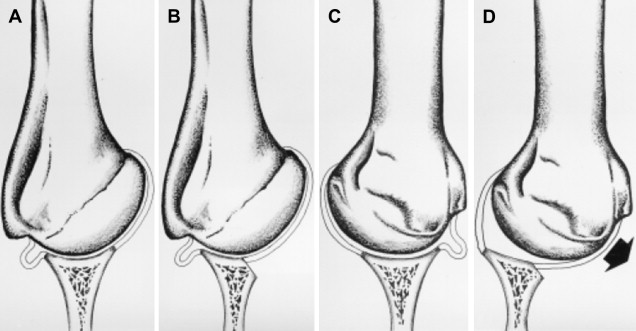
Increasing anteroinferior glenoid bone loss has been associated also with increased contact pressures. Greis and colleagues showed in a cadaveric study that a 30% glenoid bone defect led to a 41% decreased articular contact area of the entire glenoid and a 100% increase in mean contact pressures. These findings may have implications in the development of postoperative arthritis, and potentially support the findings of Buscayret and colleagues that the presence of osseous glenoid rim lesions is a risk factor in the development of arthritis, and that the development of postoperative arthritis correlates with an increased number of preoperative dislocations.
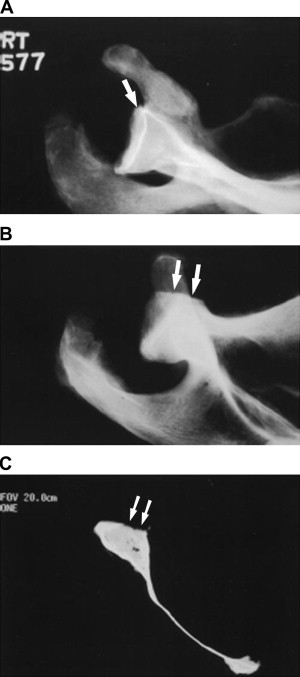
In patients with anterior shoulder instability, bony lesions are not limited to the glenoid but frequently also affect the humeral head. The classic Hill-Sachs lesion, in which the posterolateral aspect of the anteriorly dislocated head impacts the anterior glenoid rim, occurs in up to 90% of primary dislocators, 100% of patients with recurrent instability, and 40% of patients with recurrent anterior shoulder subluxations ( Fig. 2 ). Although lesions involve less than 20% of the articular surface and are considered clinically insignificant, those larger than 20% to 30% may be relevant contributors to recurrent instability.

From a pathoanatomic standpoint, when caring for patients for whom treatment of instability failed, both soft tissue and bony issues must be addressed. The surgeon should identify and be prepared to address not only the Bankart lesion but also any excess capsular tissue and relevant bony lesions.
Clinical evaluation
In patients for whom treatment of instability failed, a careful clinical workup is essential to diagnose and appropriately address the underlying problem. The essential question remains: “Why do we have a ‘failed’ instability patient?” Is the patient complaining of recurrent instability or a different complication, such as pain, loss of motion, or decreased strength? A proper diagnosis is the foundation on which to direct treatment. A thorough history and physical examination, and judicious use of imaging studies, will help separate patients with posterior instability, multidirectional instability, and other labral disorders (such as a humeral avulsion of the glenohumeral ligament [HAGL] lesion) from those with traumatic anterior instability.
History and Physical Examination
Details of the patient’s history are focused on assessing the severity of the instability, confirming the diagnosis, and identifying any associated lesions (eg, bone loss, capsular tears). Up to 89% of failed prior stabilization procedures have been shown to have some degree of glenoid bone loss. Arm position during the injury should be determined, in addition to avoidance of positions that make the patient apprehensive about possible instability. These facts provide significant clues as to the type of instability the patient is experiencing.
The nature of the recurrence episode is also important to determine. A trivial event, such as one occurring during simple activities of daily living or sleeping, suggests the presence of persistent capsular laxity or an osseous defect. However, a major event, especially one requiring a reduction, suggests a disruption of the prior Bankart repair and should raise suspicion of the presence of an engaging Hill-Sachs lesion.
The physical examination should involve comparison with the contralateral shoulder and begins with observation of the shoulder’s resting position. Range of motion and strength testing are important to assess. Loss of motion may be caused by chondrolysis, hardware impingement, or overtightening of the capsulolabral complex. Strength deficits may be caused by a concomitant rotator cuff deficiency or neurapraxia; in particular, the axillary and musculocutaneous nerve functions must be examined. A thorough examination of rotator cuff function should be documented in any patient older than 40 years, because this age group has a higher incidence of rotator cuff tearing with traumatic anterior shoulder dislocations, and this may contribute to their sense of “failure.” Subscapularis function should be assessed by using the belly press or lift-off tests. This is especially important in patients with a previous open Bankart repair, because studies have shown that 23% of these patients will have an incompetent subscapularis with a positive lift-off test and only 27% the strength of their contralateral side. In a study of patients with clinical subscapularis deficiencies, Sachs and colleagues showed that only 57% reported good to excellent results and would have the surgery again.
Generalized ligamentous laxity should be tested for, because its presence may suggest increased baseline capsular redundancy. The Beighton score, which quantifies joint laxity and hypermobility, may be useful. It includes assessment of elbow and knee hyperextension, metacarpophalangeal joint hyperextension, the ability to approximate the thumbs to forearm, and the ability to rest the palms resting on the floor with the knees extended.
The sulcus test should be performed to identify and quantify inferior capsular laxity. Provocative examination maneuvers, such as apprehension testing at varying degrees of abduction and external rotation followed by relocation testing, are vital to characterize the nature of the instability. These tests are greater than 72% sensitive and greater than 92% specific when apprehension is used as the end point (and not pain). Patients with instability at early and midranges of motion are more likely to have a complicating bony lesion. A load-and-shift maneuver may be helpful to quantify any instability, and the examiner should pay careful attention to any crepitus at the edges, which may also suggest a bony defect.
Imaging
Adequate imaging studies are essential in the workup of a patient who underwent failed instability surgery, because they facilitate identification and quantification of bony defects. Standard radiographs, which include an anteroposterior (AP), a true AP, and an axillary view, may suggest subtle bone loss. Modified axillary views, such as the West Point view, are often helpful in visualizing anteroinferior glenoid bone defieciencies. In cadaveric models, this view has been shown to accurately estimate the size of the rim defect, whereas it is significantly underestimated on the standard axillary view ( Fig. 3 ). Additional radiographs, such as the Stryker notch view and the AP view with the humerus in internal rotation, are often useful in defining Hill-Sachs lesions of the humerus.
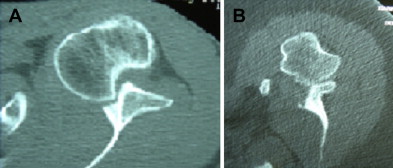
Further imaging studies should be performed in patients whose clinical history and examination are suspicious for glenoid bone loss or whose radiographs show any bony defect. A history of multiple dislocations, the progressive ease of dislocation and reduction, prior failed instability surgery, and marked apprehension and guarding at lower abduction angles on examination are all indications to obtain a CT scan. The CT scan allows definition of both lesions of the humeral head and the glenoid fossa ( Fig. 4 ). Axial and sagittal views permit precise measurement of any glenoid defects. In a review of 123 computed tomography (CT) scans in patients with anterior shoulder instability, Saito and colleagues defined the common location of the glenoid defect to be centered around the 3-o’clock position, extending inferiorly. In their cadaveric study, Itoi and colleagues showed that the critical 21% defect appears as a 50% glenoid bone loss on a single axial slice across the lower one fourth of the glenoid.
The use of three-dimensionally reconstructed CT images with the humeral head subtracted has been recommended to facilitate quantification of glenoid bone loss. Because the inferior two thirds of the glenoid has been shown to consistently be a “circle,” one can use the en face three-dimensional image and calculate the area of bone loss as a percentage of the circle ( Fig. 5 ). Three-dimensional CT imaging can also be used to measure the length of the glenoid lesion. Gerber and Nyffeler found that if the length of the lesion was equal to half the widest diameter in the anteroposterior plane, then the resistance to dislocation was decreased by more than 30%.

MR arthrography can also be helpful in evaluating patients for whom instability surgery failed because it permits better delineation of associated soft-tissue pathology and may detect rotator cuff tears, HAGL, capsular tears or laxity, and posterior extension of Bankart lesions. A recent study of patients with recurrent instability showed MR arthrography to be 91.9% accurate in assessing pathologic labral conditions and other internal derangements compared with arthroscopic findings. Recognition of this concomitant pathology allows for appropriate surgical planning to address these lesions and can lead to improved outcomes.
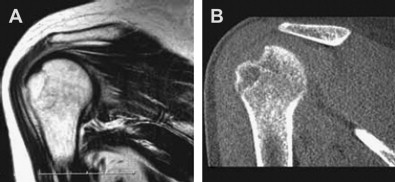
All of these imaging modalities play a role in the workup of patients for whom instability repair failed. Plain radiographs remain the baseline screening tool. Although MR arthrography excels at detecting soft-tissue injuries, it often underestimates the extent of bony lesions ( Fig. 6 ). It should not substitute for CT with three-dimensional imaging, which persists as the gold standard for quantification of bony defects of the glenoid fossa and humeral head.
Clinical evaluation
In patients for whom treatment of instability failed, a careful clinical workup is essential to diagnose and appropriately address the underlying problem. The essential question remains: “Why do we have a ‘failed’ instability patient?” Is the patient complaining of recurrent instability or a different complication, such as pain, loss of motion, or decreased strength? A proper diagnosis is the foundation on which to direct treatment. A thorough history and physical examination, and judicious use of imaging studies, will help separate patients with posterior instability, multidirectional instability, and other labral disorders (such as a humeral avulsion of the glenohumeral ligament [HAGL] lesion) from those with traumatic anterior instability.
History and Physical Examination
Details of the patient’s history are focused on assessing the severity of the instability, confirming the diagnosis, and identifying any associated lesions (eg, bone loss, capsular tears). Up to 89% of failed prior stabilization procedures have been shown to have some degree of glenoid bone loss. Arm position during the injury should be determined, in addition to avoidance of positions that make the patient apprehensive about possible instability. These facts provide significant clues as to the type of instability the patient is experiencing.
The nature of the recurrence episode is also important to determine. A trivial event, such as one occurring during simple activities of daily living or sleeping, suggests the presence of persistent capsular laxity or an osseous defect. However, a major event, especially one requiring a reduction, suggests a disruption of the prior Bankart repair and should raise suspicion of the presence of an engaging Hill-Sachs lesion.
The physical examination should involve comparison with the contralateral shoulder and begins with observation of the shoulder’s resting position. Range of motion and strength testing are important to assess. Loss of motion may be caused by chondrolysis, hardware impingement, or overtightening of the capsulolabral complex. Strength deficits may be caused by a concomitant rotator cuff deficiency or neurapraxia; in particular, the axillary and musculocutaneous nerve functions must be examined. A thorough examination of rotator cuff function should be documented in any patient older than 40 years, because this age group has a higher incidence of rotator cuff tearing with traumatic anterior shoulder dislocations, and this may contribute to their sense of “failure.” Subscapularis function should be assessed by using the belly press or lift-off tests. This is especially important in patients with a previous open Bankart repair, because studies have shown that 23% of these patients will have an incompetent subscapularis with a positive lift-off test and only 27% the strength of their contralateral side. In a study of patients with clinical subscapularis deficiencies, Sachs and colleagues showed that only 57% reported good to excellent results and would have the surgery again.
Generalized ligamentous laxity should be tested for, because its presence may suggest increased baseline capsular redundancy. The Beighton score, which quantifies joint laxity and hypermobility, may be useful. It includes assessment of elbow and knee hyperextension, metacarpophalangeal joint hyperextension, the ability to approximate the thumbs to forearm, and the ability to rest the palms resting on the floor with the knees extended.
The sulcus test should be performed to identify and quantify inferior capsular laxity. Provocative examination maneuvers, such as apprehension testing at varying degrees of abduction and external rotation followed by relocation testing, are vital to characterize the nature of the instability. These tests are greater than 72% sensitive and greater than 92% specific when apprehension is used as the end point (and not pain). Patients with instability at early and midranges of motion are more likely to have a complicating bony lesion. A load-and-shift maneuver may be helpful to quantify any instability, and the examiner should pay careful attention to any crepitus at the edges, which may also suggest a bony defect.
Imaging
Adequate imaging studies are essential in the workup of a patient who underwent failed instability surgery, because they facilitate identification and quantification of bony defects. Standard radiographs, which include an anteroposterior (AP), a true AP, and an axillary view, may suggest subtle bone loss. Modified axillary views, such as the West Point view, are often helpful in visualizing anteroinferior glenoid bone defieciencies. In cadaveric models, this view has been shown to accurately estimate the size of the rim defect, whereas it is significantly underestimated on the standard axillary view ( Fig. 3 ). Additional radiographs, such as the Stryker notch view and the AP view with the humerus in internal rotation, are often useful in defining Hill-Sachs lesions of the humerus.
Further imaging studies should be performed in patients whose clinical history and examination are suspicious for glenoid bone loss or whose radiographs show any bony defect. A history of multiple dislocations, the progressive ease of dislocation and reduction, prior failed instability surgery, and marked apprehension and guarding at lower abduction angles on examination are all indications to obtain a CT scan. The CT scan allows definition of both lesions of the humeral head and the glenoid fossa ( Fig. 4 ). Axial and sagittal views permit precise measurement of any glenoid defects. In a review of 123 computed tomography (CT) scans in patients with anterior shoulder instability, Saito and colleagues defined the common location of the glenoid defect to be centered around the 3-o’clock position, extending inferiorly. In their cadaveric study, Itoi and colleagues showed that the critical 21% defect appears as a 50% glenoid bone loss on a single axial slice across the lower one fourth of the glenoid.
The use of three-dimensionally reconstructed CT images with the humeral head subtracted has been recommended to facilitate quantification of glenoid bone loss. Because the inferior two thirds of the glenoid has been shown to consistently be a “circle,” one can use the en face three-dimensional image and calculate the area of bone loss as a percentage of the circle ( Fig. 5 ). Three-dimensional CT imaging can also be used to measure the length of the glenoid lesion. Gerber and Nyffeler found that if the length of the lesion was equal to half the widest diameter in the anteroposterior plane, then the resistance to dislocation was decreased by more than 30%.
MR arthrography can also be helpful in evaluating patients for whom instability surgery failed because it permits better delineation of associated soft-tissue pathology and may detect rotator cuff tears, HAGL, capsular tears or laxity, and posterior extension of Bankart lesions. A recent study of patients with recurrent instability showed MR arthrography to be 91.9% accurate in assessing pathologic labral conditions and other internal derangements compared with arthroscopic findings. Recognition of this concomitant pathology allows for appropriate surgical planning to address these lesions and can lead to improved outcomes.
All of these imaging modalities play a role in the workup of patients for whom instability repair failed. Plain radiographs remain the baseline screening tool. Although MR arthrography excels at detecting soft-tissue injuries, it often underestimates the extent of bony lesions ( Fig. 6 ). It should not substitute for CT with three-dimensional imaging, which persists as the gold standard for quantification of bony defects of the glenoid fossa and humeral head.









