Open and Arthroscopic Excision of Ganglion Cysts and Related Tumors
Mitchell E. Nahra
John S. Bucchieri
DEFINITION
Ganglion Cysts
Ganglion cysts, although not true cysts, are the most common tumors of the hand and wrist.
These fluid-filled cysts are a frequent cause of hand and wrist pain.
Ganglion cysts typically arise from either a joint or tendon sheath.
Most ganglion cysts occur in the wrist. Dorsal wrist ganglion cysts account for 60% to 70% of all ganglion cysts, with volar wrist ganglion cysts accounting for about 18% to 20%.1
Ganglion cysts may also arise from a tendon sheath (volar retinacular cyst) or occur in association with arthritis (degenerative mucous cyst).
Giant Cell Tumors
ANATOMY
Ganglion Cysts
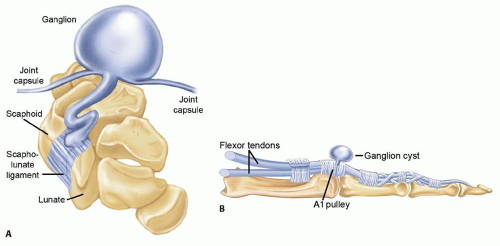
Ganglion cysts typically consist of a cyst sac that communicates through a stalk to an underlying joint or tendon sheath (FIG 1).
The cyst sac may have a single cavity or be multilobulated.
Although not a true cyst, lacking an epithelial lining, ganglion cysts are typically filled with a clear, viscous, jelly-like mucinous fluid made up of glucosamine, albumin, globulin, and a high concentration of hyaluronic acid.17
Giant Cell Tumors
The tumor is usually a multilobular, well-circumscribed mass, ranging in size from 0.5 to 7 cm.6
The color ranges from yellow to deep brown depending on the amount of hemosiderin, histiocytes, and collagen present in the lesion.
These lesions have a thin pseudocapsule. Aggressive lesions may invade adjacent soft tissue, tendon, and capsular structures and can envelop neurovascular bundles. A large study showed joint involvement in one-fifth of all cases.7 Long-standing lesions may erode into cortical bone but will not involve cartilage or the medullary canal of bone. Satellite lesions may occur.
Histologically, giant cell tumors contain collagen-producing polyhedral-shaped histiocytes, scattered multinucleated giant cells, and hemosiderin deposits.6
Epidermal Inclusion Cysts
Epidermal inclusion cysts are well-circumscribed, firm, and slightly mobile lesions.
They are often superficial and adherent to overlying skin.
They may be flesh-colored, yellow, or white.
They contain a thick, white, keratinous material.
Cysts in the fingertip may erode into the distal phalanx, causing a lytic lesion.
Histologically, they are cysts filled with keratin and lined with epithelial cells.
PATHOGENESIS
Ganglion Cysts
The true causes of ganglion cysts remain unclear, although multiple theories have been proposed.
Some early investigators theorized that ganglion cysts occurred as the result of synovial herniation and others felt that ganglion cysts resulted from mucoid degeneration.
A more recent theory proposes that ganglion cysts arise from stress at the synovial capsular interface. This stress, such as stretching of the capsular and ligamentous structures, stimulates the production of mucin from modified synovial, mesenchymal, and fibroblast cells, all of which have been shown to produce hyaluronic acid. The mucin then dissects through the capsular and ligamentous tissues, forming the main cyst. The fluid may enter the cyst from the capsular ligamentous interface via a one-way valve type of mechanism and then decrease as the water component is resorbed, accounting for the often-fluctuating cyst size.1
Giant Cell Tumors
The cause of giant cell tumors is not known. There is a strong association of giant cell tumors with rheumatoid arthritis. There are no clinical studies associating these tumors with trauma.6
Although these tumors are histologically similar to the pigmented villonodular synovitis seen in large joints in the lower extremity, they are thought to be clinically distinct lesions.
Epidermal Inclusion Cysts
Epidermal inclusion cysts occur as a result of trauma when epithelial cells are introduced into the underlying subcutaneous tissues or bone. These cells slowly grow to produce a cyst lined with epithelial cells and filled with keratin.
NATURAL HISTORY
Ganglion Cysts
Ganglion cysts typically arise spontaneously and are most common in the second through the fourth decade but may arise in the pediatric population19 as well as the aged.
Once present, ganglion cysts tend to fluctuate in size depending on the amount of fluid present in the cyst at any given time. Patients often note that the cyst becomes larger after increased periods of activity and decreases in size with inactivity.
Ganglion cysts tend to be self-limiting and do not typically continue to expand in size.
If left untreated, ganglion cysts can persist for years. They may resolve or rupture spontaneously. One cannot predict how long that they will persist or if and when they will resolve.
Resolution is far more common in the pediatric population.
Giant Cell Tumors
The lesion begins as a single nodule, becoming multinodular as it enlarges.
Malignant transformation of giant cell tumor of the tendon sheath in the hand has not been reported.6
Epidermal Inclusion Cysts
These lesions occur months to years after a traumatic event. They grow slowly to produce a painless mass, most commonly seen in the fingertip.
Malignant transformation of these lesions in the hand has not been reported.12
PATIENT HISTORY AND PHYSICAL FINDINGS
Ganglion Cysts
Patients often present with an asymptomatic mass that has been present for weeks to years.
A history of trauma is often absent.
Pain if present is often described as a dull ache. Nocturnal pain is uncommon and pain is more common with active hand use.
Paresthesias are rare but can occur if the ganglion cyst compresses any local nerves.
Patients often report that the mass tends to fluctuate in size, a characteristic typical of ganglion cysts and not typical of other types of soft tissue tumors.
Patients with wrist ganglion cysts—particularly dorsal wrist cysts—will often complain of weakness of grip.
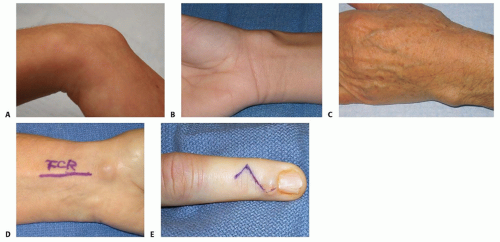
Patients with dorsal wrist ganglion cysts most commonly note a mass over the dorsum of the wrist, typically over the dorsal scapholunate region. In contrast, patients with volar wrist ganglion cysts typically note a mass over the volar aspect of the wrist in the interval between the flexor carpi radialis (FCR) and first extensor compartment tendons.
Volar retinacular cysts or ganglion cysts of tendon sheath usually present as a mass in the palm in the region of the first and second annular pulleys. The cyst is typically fluctuant but may feel like a firm nodule. The cyst is usually slightly mobile but does not often glide with flexor tendon movement.
These types of cysts are often painless at rest but become painful when patients perform activities that involve forceful grip.
Degenerative mucous cysts are ganglion cysts that arise from the distal interphalangeal joint, usually in association with underlying osteoarthritis.4 Patients often note a painless soft tissue mass that arises from the dorsal surface of the joint, radially or ulnarly (less commonly in the midline), often extending into the eponychial fold region.
Commonly, the cyst will thin the overlying dermis, resulting in rupture of the skin, and the patient often reports drainage.
Physical examination begins with inspection (FIG 2).
Being fluid-filled, ganglion cysts will often transilluminate, whereas other more solid soft tissue lesions will not.
Ganglion cysts usually occur in specific locations in the hand and wrist. Swelling or masses in these locations are diagnostic clues that a ganglion cyst may be present.
The examiner should palpate the mass for fluctuance and mobility and assess tenderness.
Ganglion cysts are generally fluctuant and slightly mobile. When they become more distended with fluid, they may feel more firm and less fluctuant. Firm, less mobile masses suggest the possibility of other soft tissue lesions.
Ganglion cysts of tendon sheath do not usually glide with tendon motion, but less common ganglion cysts, such as those that arise in the fourth extensor compartment, are often adherent and do glide with tendon motion.
The examiner should assess joint mobility through the range of motion. With the exception of dorsal wrist ganglion cysts, which may cause some loss of wrist dorsiflexion secondary to impingement, loss of joint range of motion suggests the possibility of an underlying joint abnormality.
Giant Cell Tumors
Giant cell tumors are most common in the fourth to sixth decade, with a slight predominance in women.
Patients typically present with a slow-growing, multilobulated, firm, painless mass present for several months to years.
Lesions usually occur in the radial three digits of the hand on the volar surface. Dorsal involvement, particularly around the distal interphalangeal joint, is not uncommon.7
These lesions are typically firmer than ganglion cysts and do not transilluminate.
Large lesions may limit range of motion or result in neuropathic symptoms as a result of compression of digital nerves.
Direct palpation typically reveals a firm, multinodular, nontender lesion.
Loss of range of motion may occur when large lesions occur near the interphalangeal joints.
Patients may have sensory deficits secondary to digital nerve compression. These can be revealed by testing two-point discrimination.
Epidermal Inclusion Cysts
Epidermal inclusion cysts are more common in men than in women and occur in the third to fourth decade.2
Patients commonly present with a painless, slow-growing mass after a laceration, puncture wound, or traumatic amputation of the finger.2
These lesions should be suspected in laborers who have a painless mass in the palm.12
Erythematous and painful lesions have been reported. One study reported two cases mimicking a collar-button abscess resulting from rupture of the cyst in the palmar soft tissues.20
These lesions are typically firmer than ganglion cysts and do not transilluminate.
Direct palpation will reveal a lesion that is firm, nontender, superficial, and mobile.
Loss of range of motion may occur when large lesions occur near the interphalangeal joints.
Two-point discrimination testing may reveal sensory deficits secondary to digital nerve compression.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Ganglion Cysts
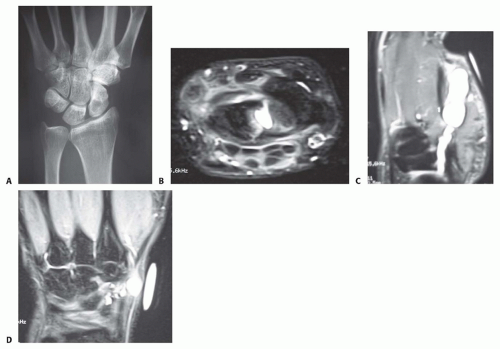
Radiographs are obtained if there is clinical suspicion of an underlying bony abnormality noted on physical examination, such as joint crepitation, swelling, carpal instability, or a history of trauma.
Radiographs are also useful in identifying an intraosseous ganglion cyst in patients with wrist pain of uncertain cause (FIG 3A).
Radiographs are also often obtained in patients with a degenerative mucous cyst of the digit because the cysts typically arise as the result of degenerative arthritis of the distal interphalangeal joint.
If the clinical findings suggest the possibility of an occult ganglion cyst, or if there is suspicion that the patient may
have a symptomatic intraosseous ganglion cyst, magnetic resonance imaging (MRI) can be a useful tool to confirm the diagnosis (FIG 3B).
MRI can also be used to better localize the site of origin as part of preoperative planning in ganglion cysts that occur in atypical locations (FIG 3C,D).
Ultrasound can also be used to diagnose ganglion cysts, but this test is examiner dependent and less sensitive and specific than MRI.
Computed tomography (CT) scans are generally obtained only for preoperative planning to better localize and evaluate the bony architecture of intraosseous ganglion cysts.
Giant Cell Tumors
Plain radiographs show a soft tissue mass. Juxtacortical lesions may show bony erosion.
MRI demonstrates a benign-appearing encapsulated mass, with decreased signal on T1- and T2-weighted images.
Epidermal Inclusion Cysts
Plain radiographs show a soft tissue mass.
A lytic lesion may be seen in the distal phalanx if it erodes into bone.
DIFFERENTIAL DIAGNOSIS
Ganglion Cysts
Epidermoid inclusion cyst
Giant cell tumor of tendon sheath
Lipoma
Synovial cyst
Giant Cell Tumors
Fibroma of the tendon sheath, synovial chondromatosis, synovial hemangioma, tophaceous gout, foreign body granuloma, periosteal chondroma
NONOPERATIVE MANAGEMENT
Of the three tumors discussed in this chapter, only ganglion cysts can be managed without surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree