Olecranon Fractures: Open Reduction Internal Fixation
Gregory J. Schmeling
Lawrence J. Maciolek
Indications/Contraindications
Olecranon fractures are a result of direct or indirect forces, or a combination of both (1). Direct forces drive the olecranon into the distal humerus, often producing comminuted fractures with depressed joint fragments, similar to a tibial plateau fracture. Olecranon fractures, which occur indirectly through the contraction of the triceps muscle, generally produce transverse or short oblique fracture patterns.
Minimally displaced olecranon fractures are defined as less than 2 mm of joint gap or step-off, intact, active-elbow extension, and no significant fragment motion with elbow flexion. Fractures are displaced if they do not meet these criteria (1).
The treatment objectives for olecranon fractures are reconstruction of the articular surface, restoration of the elbow extensor mechanism, preservation of elbow motion and function, and prevention or avoidance of complications (2). The indications for operative treatment include displaced fractures, injuries with elbow extensor-mechanism disruption, and open fractures. Indications for conservative treatment include nondisplaced fractures, injuries where the elbow extensor mechanism is intact, and poor overall medical condition of the patient.
Operative treatment options include open reduction and internal fixation (ORIF) and fragment excision with elbow extensor-mechanism reconstruction (2,3,4). For displaced fractures, the treatment goals are met most often with internal fixation techniques. These techniques consist primarily of tension band wiring or plate osteosynthesis.
Olecranon fractures usually occur as isolated injuries, but they are occasionally found in the polytrauma patient. With isolated fractures, a history of a fall with elbow pain is the most common presenting complaint. Physical examination reveals a painful, swollen elbow, and in displaced fractures, a palpable defect is often identified. Crepitus with elbow motion may also be present. The inability to extend the elbow against gravity suggests loss of the integrity of the elbow extensor mechanism. Neurovascular evaluation should include particular attention to the ulnar nerve. The proximity of the ulnar nerve places it at risk for injury, especially when direct forces are involved in the accident.
Essential radiographs include an anteroposterior (AP) view and a true lateral view. When the olecranon fracture is part of an elbow fracture dislocation, traction radiographs are used to evaluate the injury as well. The lateral radiograph reveals the extent of the fracture and the presence of comminution or joint depression. The integrity of the radial head–capitulum articulation is examined, and subluxation or dislocation of the semilunar notch from the trochlea is noted. The AP radiograph is examined for sagittal fracture lines that are not well visualized on the lateral view. Comparison radiographs can be helpful in complex fracture patterns.
Preoperative Planning
To optimize outcomes, a preoperative plan is drawn and a surgical tactic developed. The preoperative plan begins with a tracing of the fracture fragments. The fragments are then reduced on paper. The need for bone graft to support depressed intra-articular fragments is determined. The proposed fixation is added. The method of fixation chosen is dependent on the fracture geometry and the experience of the surgeon. The surgical tactic is a sequential outline of the planned procedure and is added to the drawing (Fig. 8.1).
Although there are many classification schemes for olecranon fractures, we prefer that of the Orthopaedic Trauma Association (5). The location of the fracture is in the proximal segment of the radius and ulna (6). The fractures are divided into three types: extra-articular (21-A), articular and involving the surface of one bone (21-B), and articular and involving the surface of both bones (21-C). Extra-articular avulsion fractures are type 21-A
while intra-articular fractures are type 21-B. A more detailed description of this classification is found in the Orthopaedic Trauma Association’s Fractures and Dislocation Compendium (5).
while intra-articular fractures are type 21-B. A more detailed description of this classification is found in the Orthopaedic Trauma Association’s Fractures and Dislocation Compendium (5).
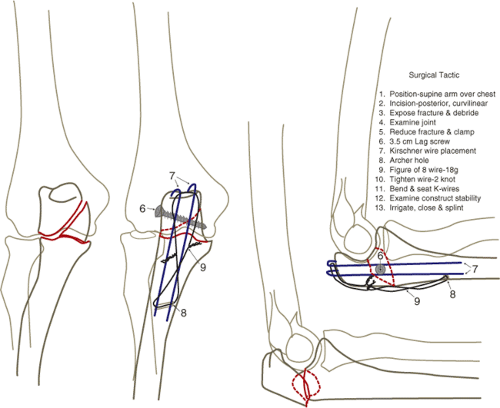 Figure 8.1. Preoperative plan. This is a tracing from the radiographs: ulna (blue); fixation (red); and humerus/radius (black). |
It is easier to conceptualize olecranon fractures as transverse, oblique, comminuted, or elbow fracture dislocations (Fig. 8.2). Transverse and oblique fractures may have a depressed joint segment similar to that seen in tibial plateau fractures. Depressed segments are elevated and may require bone graft or other support to maintain elevation. Oblique fractures can be oriented proximally or distally. Lag screws are frequently used with oblique fractures. Comminuted fracture patterns usually occur in isolation, but the radiographs must be scrutinized to rule out a fracture dislocation of the elbow.
The two most common methods of fixation are either tension band wiring or plate osteosynthesis with or without a lag screw (3,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24,25,26). A tension band construct may consist of two Kirschner (K) wires with a figure-of-eight wire or cable, or it may be made of an intramedullary screw with a figure-of-eight wire. Alternatively, a lag screw and dorsal plate (3.5-mm semitubular or reconstruction) can be used (Fig. 8.3A–C). The cable is easier to place and has a low-profile crimp rather than two prominent wire knots. A figure-of-eight wire alone does not provide sufficient stability to resist physiologic loading (21). Advocates of the lag screw–dorsal plate technique cite less operative time, better reductions, fewer
hardware symptoms, less postoperative loss of reduction, and lower incidence of infection (7,10,20,26). The lag screw–neutralization plate construct consists of a lag screw across the fracture and a radial, ulnar, or dorsal neutralization plate. Two K wires with a figure-of-eight wire will also neutralize the lag screw (Fig. 8.3D).
hardware symptoms, less postoperative loss of reduction, and lower incidence of infection (7,10,20,26). The lag screw–neutralization plate construct consists of a lag screw across the fracture and a radial, ulnar, or dorsal neutralization plate. Two K wires with a figure-of-eight wire will also neutralize the lag screw (Fig. 8.3D).
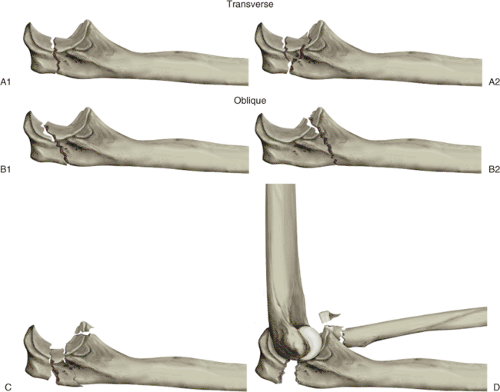 Figure 8.2. Olecranon fractures: (A1) transverse, (A2) transverse with joint depression, (B1) proximal oblique, (B2) distal oblique, (C) comminuted, (D) fracture-dislocation. (From McKee MD, Jupiter JB. Trauma to the adult elbow and fractures of the distal humerus. In: Browner BD, Jupiter JB, Levine AM, et al, eds. Skeletal trauma. Philadelphia: W.B. Saunders; 1992:1455–1522 ; Fig. 41-16.) |
Based on the injury pattern, patient profile, and clinical experience, the surgeon must determine which fixation technique to employ for a given fracture. In the absence of complications, outcomes for each of the fixation techniques are comparable (12,21). However, biomechanical and clinical evidence suggests that certain techniques may be advantageous when applied to specific fracture patterns.
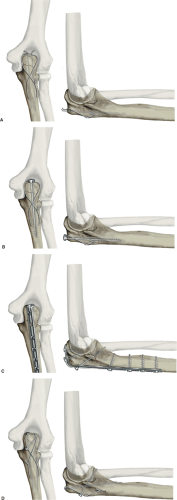 Figure 8.3. Tension-band constructs. A. Two K wires with a figure-of-eight wire (33). B. Medullary screw with a figure-of-eight wire (33). C. Dorsal plate with lag screw. D. Two K wires that engage the anterior cortex plus lag screw. (A and B from Macko D, Szabo RM. Complications of tension-band wiring of olecranon fractures. J Bone Joint Surg 1985;67A:1396–1401 ; C and D fromHelm U. Forearm and hand/mini-implants. In: Muller ME, Allgower M, Schneider R, et al, eds. Manual of internal fixation. Berlin: Springer-Verlag; 1991:453–484 , Fig. 8.6.) |
Tension band wiring techniques are the mainstay of treatment for transverse, noncomminuted, olecranon fractures, but they may also be used in some comminuted fracture patterns. In commonly used constructs, intramedullary K wires or an intramedullary screw, combined with either braided cable or monofilament wire, are used. In terms of biomechanics, tension band techniques are thought to convert the force generated by the elbow extensor mechanism into a dynamic compressive force along the articular surface of the
semilunar notch during active elbow motion (7). Although the validity of this biomechanical principle has been recently challenged, the clinical efficacy of tension band techniques is well documented (15



semilunar notch during active elbow motion (7). Although the validity of this biomechanical principle has been recently challenged, the clinical efficacy of tension band techniques is well documented (15
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








