Olecranon Fractures
Julie E. Adams
INTRODUCTION AND CLASSIFICATION
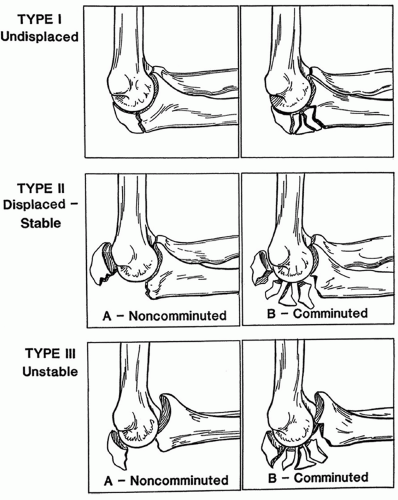
Olecranon fractures typically result from trauma to the flexed elbow (1). Lack of abundant subcutaneous tissue makes the olecranon especially vulnerable to trauma, and olecranon fractures have an estimated incidence of 1.08 per 10,000 person-years (2). The Mayo classification of olecranon fractures divides fractures into three types with subcategories related to comminution (3,4) (Fig. 3-1).
Type I fractures are nondisplaced and noncomminuted (IA) or comminuted (IB) fractures.
Type II fractures are stable, displaced fractures and may be noncomminuted (IIA) or comminuted (IIB).
Type III fractures are unstable, displaced fractures and may be noncomminuted (IIIA) or comminuted (IIIB).
In addition to these basic fracture patterns, complex fracture dislocations in which the coronoid and/or radial head are involved may exist; in addition, pure avulsion fractures of the olecranon tip are not included in this classification system.
TREATMENT OPTIONS
Broadly speaking, treatment options include immobilization, which may be appropriate for elderly low-demand patients or patients with type I fractures; excision of fracture fragments, which again may be appropriate for low-demand patients and those with small avulsion fractures; and open reduction and internal fixation (ORIF) with a variety of fixation constructs.
Type I nondisplaced fractures may be treated with immobilization in midflexion and neutral rotation for 7 to 10 days.
Close radiographic follow-up is necessary to ensure that further displacement does not occur and that the fracture heals.
Active-resisted elbow extension and weightbearing should be avoided for 6 to 8 weeks if these fractures are treated nonoperatively.
Displaced type II and III fractures typically require surgery.
Surgical goals include restoration of a congruent and stable elbow joint and of extensor strength; ideally, fixation is sufficiently stable to permit early active motion in rehabilitation in the postoperative period.
EVALUATION OF THE PATIENT
Patients generally present following acute trauma to the flexed elbow. Concomitant injuries should be excluded by careful history, physical examination above and below the elbow, and radiographs as appropriate. Three-view plain film radiographs of the elbow are obtained and inspected to determine the fracture pattern, to plan appropriate treatment, and to exclude concomitant injuries to the coronoid, the distal humerus, or the radial head. In some cases, particularly in the setting of transolecranon fractures or complex fracture dislocations, a computed tomography scan may be helpful. Two- and three-dimensional reconstructions can delineate fracture patterns more clearly and help with preoperative planning.
Although nerve palsy is rare following olecranon fractures (5,6,7,8,9,10,11 and 12), careful attention to the neurovascular status is paid and the function of the major peripheral nerves of the limb is documented, with particular attention to the ulnar nerve. Two-point discrimination is measured distally, and motor function is assessed and documented.
PROCEDURE
Supine positioning with the arm over the chest and the bed “airplaned” gives ready access to the arm but may require an additional assistant to hold the arm in place. An alternative is lateral positioning with the patient secured on a beanbag and the arm draped over an arm holder. The author employs both positions in her practice, depending on the patient’s habitus and the amount of assistance available. Others may perform the procedure in a prone position. A nonsterile tourniquet is applied proximal to the sterile field and inflated to 200 mm Hg following administration of antibiotics to improve visualization. It is helpful to have a mini C-arm unit available for intraoperative imaging and to limit radiation exposure to the patient and surgical team, and it should be confirmed that good images of the elbow can easily be obtained prior to prepping and draping the arm.
Although either general or regional anesthesia may be used, the author prefers general anesthesia as it improves patient comfort during the procedure since positioning can be awkward.
A straight posterior incision is made at the medial side of the olecranon tip, raising large fullthickness flaps. If the patient has ulnar nerve symptoms preoperatively, the nerve may be decompressed in situ; however, in the absence of symptoms preoperatively, postoperative ulnar neuritis is unlikely. The fracture is exposed, hematoma and debris removed, and the fracture inspected to make a final determination of treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree