Tendoscopy of the Ankle
Keywords
• Peroneus longus and brevis tendoscopy • Posterior tibial tendoscopy • Achilles tendoscopy • Flexor hallucis longus tendon endoscopy
Arthroscopy of the foot and ankle is a mainstream technique as a result of refined instrumentation and surgeon familiarity for a variety of pathologic conditions. With the advent of advanced arthroscopic techniques, it is a natural transition that tendoscopic techniques would be incorporated into the experienced arthroscopic surgeon’s armamentarium. Tendoscopy is an endoscopy of the tendon sheath and has been described in various tendons of the foot and ankle, including the posterior tibial, peroneal, long toe flexor, anterior tibial, and Achilles tendons.1–15 Conservative treatment of extra-articular ankle pathology is successful in most cases, but there is a 10% to 25% incidence of failed conservative treatment.2 When conservative treatment fails, most commonly open tendon surgery is advocated. Unlike the elbow or the knee, the tendon structures of the posterior ankle are deep and can be difficult to palpate; also, these structure are in close proximity to each other, which may make diagnostic imaging challenging.7 When treating extra-articular posterior ankle pathology, open treatment can consist of either a posterolateral or a posteromedial approach, which both imply risk of damage to adjacent structures.2,7 Even structures that are not directly encountered during the initial dissection can become entrapped with closure of the soft tissue envelope. Surgical wound problems are of increased concern when incisions are made in the posterior ankle region. Complication rates in open surgical treatments of the Achilles tendon vary between 4.7% and 11.6% and problems are mainly wound infections, skin sloughing, and formation of painful scars.2 With longer incisions, postoperative care may dictate the use of immobilization to promote better wound healing.7 Tendoscopy offers the advantages of less morbidity, early range of motion, and reduction in postoperative pain.5
When performing tendoscopy, the surgeon must be familiar with the anatomy of the foot and ankle. Sammarco10 provides a solid resource of the anatomy of the peroneal tendons. Brandes and Smith14 also provide a zonal anatomic system for the peroneal tendons. Van Dijk and Kort5 performed a cadaveric study where they found in 3 of the 7 explorations that the peroneal tubercle on the calcaneus was between both tendons, 4 to 5 cm distal from the tip of the fibula. The posterior tibial tendon, as mentioned previously, has mesotendinous connections along its course. Van Dijk and Kort5 offer a review of the anatomy of the posterior tibial tendon, whereas Steenstra and Van Dijk16 provide an overview of the Achilles tendon.
Lui and colleagues12 studied the flexor hallucis tendon and its various segments (zones). In their study, it was found that the medial plantar nerve was at the plantar medial side of the proximal tendon sheath in all specimens and its relationship to the more distal sheath was variable. Synovectomy at this location should be performed with caution because of the anatomic proximity of the tarsal tunnel structures. Therefore, any power instrumentation should be kept along the lateral aspect of the flexor hallucis longus tendon.
Tendoscopy developed in other anatomic regions of the body and more recently has been described in the foot and ankle. Kerr and Carpenter17 were the first to describe arthroscopic resection of olecranon and prepatellar bursae in 6 cases. The investigators had 4 good results and 2 failures. Tendoscopy of the posterior tibial, peroneus longus and brevis, and flexor hallucis longus tendons were described by van Dijk and colleagues in 1997, 1998, and 2000 respectively.5–7 Maquirriain18 performed a study on 9 cadavers in which he showed that there could be adequate access to the Achilles tendon via an endoscope.
Indications/contraindications
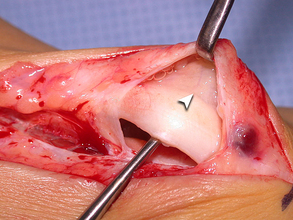
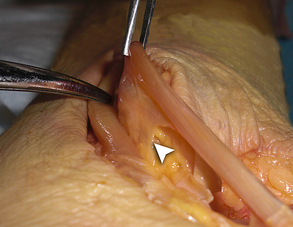
Focal tendonitis and tenosynovitis are pathologic entities that can be treated with tendoscopy. Tenosynovitis, which is associated with chronic mechanical irritation, posttraumatic adhesions, and irregularities of the posterior aspect of the fibula or tibia, can cause significant morbidity in patients. Hypertrophy of the peroneal tubercle can cause direct repetitive injury to the peroneals as well as proximal subluxation, which can be treated with endoscopic groove deepening.5,11 Pathologic thickening of the tissue surrounding the tendon can occur and specifically of the vincula. The vinculum is defined as mesotendinous tissue connecting tendons or tendon sheaths, which is a source of blood supply to the tendon.19 Van Dijk and Kort5 performed a cadaveric study where they found a consistent membranous mesotendineal structure between both peroneal tendons and tendon sheath (Fig. 1). This vinculum runs between the peroneus longus and peroneus brevis tendons and is attached to the posterolateral aspect of the fibula. Seven ankles in cadavers were examined by van Dijk and associates6 where a thin vinculumlike structure was found between the posterior tibial tendon and the tendon sheath of the flexor digitorum longus. This vinculum runs all the way proximal to the end with a free edge 3 to 4 cm above the level of the posteromedial tip of the medial malleolus. Mesotendinous thickening can become a source of morbidity, as it limits or tethers tendon excursion. This thickening can also block backside visualization of the tendon (Fig. 2). Similar thickening can occur along the posterior tibial tendon because of overuse or stage I posterior tibial tendon dysfunction; this thickening is usually seen in the hypovascular zone posterior to the medial malleolus.6
Achilles tendon pathology can be classified as insertional or noninsertional entities. Insertional tendon pathology involvement is a relative contraindication for the use of tendoscopy. Likewise, wide diffuse tendinopathy remains difficult to manage with this technique. Noninsertional pathology can be divided into tendinopathy, paratendinopathy, and a combination of the two.16 As discussed earlier, tendinopathy can be manifested by diffuse thickening of the tendon, local thickening, and partial tears.16 Paratendinopathy is characterized by painful swelling around the paratenon.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree