Current Concepts and Techniques in Foot and Ankle Surgery
Management of Pedal Puncture Wounds
Keywords
• Puncture wound • Foot • Foot infection • Antibiotics
Puncture wounds of the foot are a common injury, and infection associated with these injuries may result in considerable morbidity. These wounds may harm underlying structures, introduce foreign bodies, and deposit inoculum that leads to infections. Schwab and Powers1 reported that patients presenting to the emergency room for puncture wounds showed infection rates of 6% to 11%. The study on wound sites by Patzakis and colleagues2 indicated that 34 of their 36 inpatients had pyarthrosis, osteomyelitis, or both. For these reasons, when treating patients with puncture wounds it is important to have an efficient approach that is well thought out. Accurate diagnosis, assessment, and management are crucial in preventing a poor prognosis.
Clinical presentation
Children will often present to the emergency room with puncture wounds, particularly barefooted children playing outdoors during warmer months.3 Haverstock and Grossman4 also noted that construction workers and laborers are prone to this type of trauma as a result of occupational hazards (Fig. 1). Nails are the most frequently seen object in puncture wounds, but other items such as needles, glass, wood, plastic, metal, and even water have been known to cause this type of injury.
Understanding the timing of the injury to presentation is important for treatment protocol. A wound more than 6 hours old has a higher probability of infectious organisms, and after 48 hours there is a greater risk of complications.5,6 The history should also detail if the patient has made any attempt, successful or not, to debride the wound, to assess the possibility that the foreign body has been broken into pieces or has penetrated deeper.7
High-pressure injection injuries, such as those from paint guns and power washers, can often present as puncture wounds. These unique wounds have an increased incidence of oil, paint, or foreign debris deeply embedded within the puncture site. Patients often present with pain and minimal swelling. Because of the nature of these wounds and the increased likelihood of foreign debris being spread along facial planes, high-pressure injection injuries should be considered for surgical intervention.8
A comprehensive medical and vaccination history in patients presenting with a puncture wound is essential for proper treatment. Risks of complications are greatly increased in patients with peripheral vascular disease or who are immunocompromised.9 Special attention should be also paid to patients with diabetes, because of the unique comorbidities that are often present. Diabetic patients are also at an increased risk of developing an infection secondary to trauma.10 A thorough review of the tetanus immunization history is crucial, as it has been noted that tetanus is 3 times more common and fatalities are 4 times more common among diabetic patients.11 Often diabetics will have abnormal immune responses to infection. Compromised vascular status and ischemia can decrease the erythema associated with a local infection while simultaneously contributing to the increased degree of infection. Peripheral neuropathy also complicates the risk factors in the diabetic patient. Lavery and colleagues10 demonstrated that the loss of protective sensation in the lower extremities prolonged the time from injury to treatment because of the “delayed recognition of a limb-threatening problem.”
Physical examination
Location of the puncture wound is important for assessing the possible risks and complications. Patzakis and colleagues2 developed a schematic that can be used to quickly assess the likelihood of infection (Fig. 2).
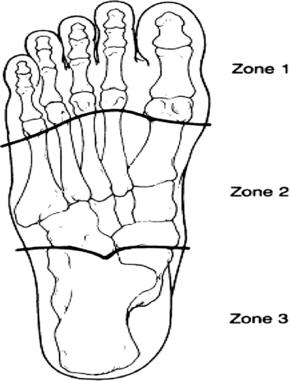
Fig. 2 Patzakis and colleagues’2 classification for the plantar surface of the foot.
(From Patzakis M, Wilkens J, Brien W, et al. Wound site as a predictor of complications following deep nail punctures to the foot. West J Med 1989;150:545–7; with permission.)
The plantar aspect of the foot was divided into 3 zones. Zone 1 extends from the metatarsal necks to the distal phalanges, zone 2 extends from the distal aspect of the calcaneus to the metatarsal necks, and zone 3 comprises the plantar aspect of the calcaneus. Patzakis and colleagues found that puncture wounds in zone 1 had the highest risk for development of osteomyelitis, followed by zone 3. Zones 1 and 3 are of significance because of the limited soft tissue and underlying osseous structures in these areas. It has also been reported that the most common occurrence of osteomyelitis in children is seen in the calcaneus.3 Patients with puncture wounds in these locations should be thoroughly evaluated, because of the minimal amount of soft tissue protecting the underlying bony structures.
Conditions of the surrounding tissues should be inspected for foreign matter, debris, and devitalized tissue. It is critical to assess for vascular compromise, and a comprehensive neurologic assessment of the limb should be performed. Range-of-motion testing and function of the surrounding tendons can be helpful in assessing the extent and depth of the wound. Depth of the injury is an important aspect of assessment because more complications are associated with an increased depth of penetration.2 If examination reveals pain, swelling, erythema, warmth fluctuation, decreased range of motion, and evidence of drainage then infection is indicated, and the wound should be aggressively treated.
Local anatomy of the puncture wound is also important for evaluating the extent of the injury, the likelihood of infection, and potential for the foreign body to migrate. Firth and colleagues12 published a case study in which a 45-mm toothpick fragment went undetected and migrated 10 cm along the flexor hallucis longus tendon sheath. Knowing the anatomy will assist in determining potential routes of migration when a foreign body is suspected, but fails to be detected through either debridement or visualization techniques.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









