Normal Gastrointestinal Function
Mark A. Gilger
The gastrointestinal (GI) tract has many functions—digestion, absorption, and secretion, as well as endocrine and immunologic functions. This system can be thought of as a tube that extends from the mouth to the anus and is divided into three parts: the foregut (mouth to proximal duodenum), midgut (distal duodenum to colon), and hindgut (distal colon and rectum). Each part has a separate blood supply. The salivary glands, pancreas, liver, and gallbladder are outgrowths of the foregut and
midgut. The in utero development of the human gut results in a digestive system that is nearly fully capable at birth.
midgut. The in utero development of the human gut results in a digestive system that is nearly fully capable at birth.
DEGLUTITION
Swallowing, or deglutition, can be seen in the fetus by approximately 16 weeks of gestation. After birth, the normal swallow develops into three phases: oral, pharyngeal, and esophageal. The oral and pharyngeal phases are voluntary; the esophageal phase is reflexive. In feeding infants, sucking is accomplished by a rhythmic lowering of the tongue and compression of the nipple or areola. The bolus of milk is propelled backward by a rolling action of the tongue posteriorly. The nasopharynx then is sealed off by the soft palate, and the larynx is brought upward and forward as the epiglottis covers the trachea. The esophageal phase begins with a relaxation of the upper esophageal sphincter, allowing the bolus to enter the esophagus. A primary peristaltic wave is initiated, which then transports the bolus to the stomach. A secondary peristaltic wave within the body of the esophagus may be initiated by distention and frequently occurs as a result of esophageal reflux.
Peristalsis also is initiated in the esophagus by migrating motor complexes. These rhythmic involuntary complexes originate independently of swallow or distention and sweep through the entire GI tract, terminating in the rectum.
The ability to swallow solid foods, although partially present at birth, is completely functional by the time the child is age 4 to 6 months. Children who have not been fed solid foods by age 15 months have difficulty swallowing them. This fact suggests that infancy is a critical time in the development of the ability to handle solid foods.
ESOPHAGUS
The esophagus develops from the embryonic foregut. During elongation, the luminal surface differentiates into stratified squamous epithelium. The esophagus and respiratory tract begin as a single tube, which divides by 2 months’ gestation. Incomplete division of the tube into two separate organs results in a variety of anomalies, such as a tracheoesophageal fistula.
The esophagus is a collapsed hollow tube lying posterior to the trachea. The esophageal mucosa is oriented into longitudinal folds that disappear when the esophagus is distended. Unlike the rest of the GI tract, the esophagus has no serosal surface. The upper third of the esophagus is striated or skeletal muscle, whereas the lower esophagus is smooth muscle. The luminal surface is covered with stratified squamous epithelium. Blood is supplied to the upper third of the esophagus by the inferior thyroid artery, whereas branches of the descending thoracic aorta supply the body. The left gastric artery supplies blood to the lower third of the esophagus. Venous drainage is to the superior vena cava superiorly, the azygos vein from the body, and the gastric veins from the lower esophagus. The gastric veins drain to the portal venous system. In cases of portal hypertension, venous flow can reverse, resulting in esophageal varices. The esophagus is innervated by the spinal accessory nerve and the vagus nerve.
Functionally, the esophagus is divided into three zones: the upper esophageal sphincter, the body, and the lower esophageal sphincter. The upper esophageal sphincter has a resting pressure of approximately 30 mm Hg and normally is closed. Swallowing results in relaxation and dilation of the upper esophageal sphincter and initiates a primary peristaltic wave that passes through the body of the esophagus. The lower esophageal sphincter has a resting manometric pressure of approximately 20 mm Hg and also normally is contracted. The primary peristaltic wave opens the lower esophageal sphincter for approximately 7 seconds to allow passage of material into the stomach. The lower sphincter then returns to its resting state, which prevents reflux of acidic gastric contents into the esophagus.
STOMACH
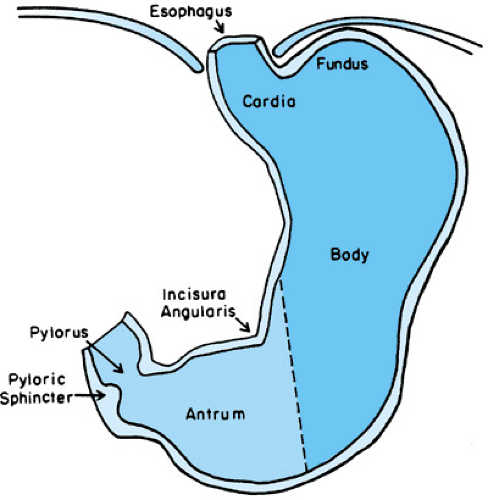
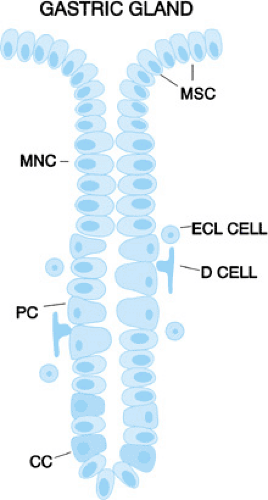
The stomach develops from the primitive foregut and is evident by 4 weeks’ gestation. Gastric glands appear by approximately 11 weeks’ gestation. Structurally, the stomach is divided into four parts—the cardia, fundus, body, and antrum—terminating with the pyloric sphincter (Fig. 342.1). Gastric glands present in the lining of the stomach are composed of four cell types: chief cells (zymogen cells), which contain zymogen granules and secrete pepsinogen; parietal cells (oxyntic cells), which secrete hydrochloric acid and intrinsic factor; mucous neck cells; and endocrine-like cells (Fig. 342.2). Production of hydrochloric acid is measurable at 15 weeks’ gestation and increases in amount until normal adult levels are reached at approximately 1 month after birth. Production of pepsin is evident at 16 weeks’ gestation and reaches adult levels by the time the child is 2 years of age.
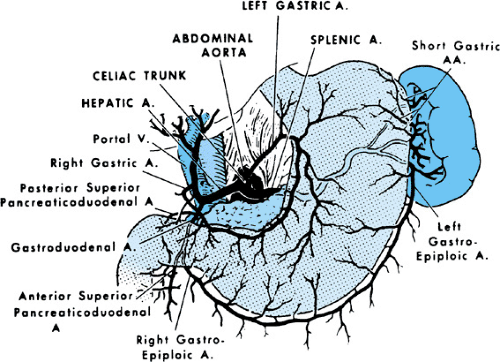
Blood supply is provided by the left and right gastric branches of the celiac artery (Fig. 342.3). Venous drainage is through the left and right gastric veins into the portal vein. The stomach is innervated by the vagus nerve and is completely autonomic.
The stomach has at least four major functions: storing meals, mixing and grinding foods, controlling the emptying of food into the duodenum, and acting as the initial barrier to pathogens and allergens entering the GI tract. At birth, the stomach has a capacity of approximately 30 mL (approximately 1 oz), but capacity increases to approximately 1,500 mL by adulthood. The fundus provides most of the storage capacity and responds to the ingestion of food by relaxing and increasing gastric volume. Mixing and grinding food are accomplished by the phasic gastric contractions and the cone shape of the
antrum. The gastric pacemaker, located in the body, generates three-per-second depolarization waves, which initiate contractions that push food toward the antrum. These contractions increase in strength at the antrum, forcing the smaller food particles, usually approximately 1 mm in size, into the duodenum. The emptying of food is controlled by the pylorus, which allows a relatively constant flow of nutrients into the duodenum. Liquids tend to empty more quickly (cool liquids faster than warm), and factors such as high fat content and high osmolarity of the meal tend to delay gastric emptying.
antrum. The gastric pacemaker, located in the body, generates three-per-second depolarization waves, which initiate contractions that push food toward the antrum. These contractions increase in strength at the antrum, forcing the smaller food particles, usually approximately 1 mm in size, into the duodenum. The emptying of food is controlled by the pylorus, which allows a relatively constant flow of nutrients into the duodenum. Liquids tend to empty more quickly (cool liquids faster than warm), and factors such as high fat content and high osmolarity of the meal tend to delay gastric emptying.
Gastric acid plays an important role in destroying or damaging intestinal pathogens. This acid barrier is the first of a series of nonimmunologic mechanisms that eradicate pathogens and other noxious agents.
SMALL INTESTINE
The small intestine develops from the midgut portion of the fetal archenteron or primitive gut. Initial growth occurs out of the abdominal cavity, within the vitelline stalk of the umbilicus. It returns into the abdominal cavity by 10 weeks’ gestation due to the fixation of the cecum to the right lower quadrant of the abdomen. Failure of this fixation rotation results in the common malrotation syndromes. Villous formation is apparent first at 8 weeks’ gestation and proceeds in a proximal to distal fashion. The entire small bowel has both villi and crypts by 12 weeks, and the enzymatic activities of pepsin, trypsin, and lipase have been documented by 18 weeks’ gestation. The small intestine immune apparatus, M cells (membranous cells), and Peyer patches appear at 2 weeks’ gestation. The number of Peyer patches increases until puberty, then decreases throughout adult life. The mucosa of the small intestine contains more immunocytes (plasma cells, lymphocytes, and so forth) than does any other organ in the body: 1 cm of small intestine contains approximately ten immunocytes (Box 342.1).
The small intestine is approximately 250 cm long in full-term infants and grows to between 2 and 3 m in the adult. The first 25 cm of small bowel or duodenum is fixed to the peritoneum. Beyond the ligament of Treitz, the intestine is freely mobile, supported only by the mesentery. The small intestine is covered by serosa (mesentery) beginning at the ligament of Treitz (Fig. 342.4). Beneath the serosa lie two muscular layers: an outer longitudinal and an inner circular layer, which act in concert to provide peristalsis. Within the submucosa, the next layer, lie numerous cellular elements, including lymphocytes, plasma cells, mast cells, eosinophils, and macrophages. Brunner glands are present in the submucosa of the duodenum (Fig. 342.4).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree