CHAPTER 8 Nonarthroplasty Treatment Options for Unicompartmental Degenerative Joint Disease
 Arthroscopy is successful at treating mechanical complaints but not the generalized pain of arthritis.
Arthroscopy is successful at treating mechanical complaints but not the generalized pain of arthritis.Arthroscopic Débridement
Mechanical symptoms associated with meniscal or chondral lesions are the clearest indication for arthroscopic débridement. However, patient expectations need to be clearly defined, and patients should be cautioned that a significant portion of their knee pain might be attributed to the existing arthritis. Multiple authors have shown improvement in knee rating score, improved knee function, decreased anti-inflammatory use, and high patient satisfaction in osteoarthritic knees treated with arthroscopic lavage and débridement.1–4 Steadman et al.’s systematic arthroscopic approach to the degenerative knee included the expansion of joint space through the release of joint contractures, removal of loose bodies, limited chondroplasty, meniscectomy of unstable tears, thermal ablation of synovitis, and excision of osteophytes blocking full extension.4 Their published results on a consecutive series of patients with severe arthritis who underwent the procedure showed that greater than 70% of them had significant gains in knee function scores, satisfaction, and delay of arthroplasty at a minimum of 3 years postoperatively.4
The most cited predictors of failure of arthroscopic intervention include malalignment greater than 5°, age greater than 60, persistent symptoms greater than 1 year, history of prior surgery, and joint space less than 2 mm.5–9 Steadman et al. added the presence of “kissing” grade 4 lesions and severity of joint contracture as additional independent predictors of failure. The preoperative presence of a symptomatic mechanical lesion seems to be the most reproducible predictor of success from arthroscopic débridement. Multiple authors have shown persistent symptomatic benefit in patients with combined meniscal pathology and degenerative changes treated with partial meniscectomy, but better results are seen if the meniscal component is acute rather than degenerative.9–13
In contrast to the multiple reports of success with arthroscopic débridement in osteoarthritis, Moseley et al. and Kirkley et al. demonstrated equal efficacy between a focused physical therapy program and arthroscopic débridement.14,15 Moseley et al. also reported similar outcomes with a “sham-operation” highlighting the power of the placebo effect.14 Their interpretation of these results has caused many clinicians to question the utility of arthroscopy in the setting of osteoarthritis.14,15 However, some surgeons criticize these studies for lacking a specific patient cohort with arthritis but predominating mechanical symptoms. The randomized nature of these two studies does demonstrate that the blind application of arthroscopic débridement to osteoarthritis is unlikely to produce successful outcomes greater than nonsurgical treatments and highlights the importance of critically analyzing the patient’s symptomatology and applying strict patient selection criteria.
Cartilage Restoration
There are multiple, well-studied restorative options for the treatment of acute full-thickness articular cartilage defects. The most common options include microfracture, osteochondral transfer, and autologous chondrocyte transplantation. Despite the continued debate surrounding the appropriate indications and expected longevity for these procedures, one can expect good to excellent results when these restorative options are applied appropriately to the acute full-thickness lesion. On the contrary, most attempts at cartilage restoration will fail in the setting of significant degenerative disease. It is thought that the osteoarthritic environment is not conducive to these techniques and that either the cartilage at the periphery of the degenerative lesion is too thin to contain the repair or the surrounding cartilage will continue to degenerate. In a review of microfracture in the degenerative knee, there were significant gains in Lysholm scores but the improvement in function was less when compared to their “traumatic” counterpart (Fig. 8–1).16 Larger lesions, older patients, those lesions defined as “degenerative” rather than “traumatic,” and bipolar lesions all were associated with less improvement in knee function scores.16 Andres et al.’s review of osteochondral autograft transplantation demonstrated significantly greater improvements in the pain relief and function of the “isolated lesion” group compared to the “degenerative lesion” group.17 In a diverse group of patients treated with autologous chondrocyte implantation, McNickle et al. found that age was an independent predictor of postoperative Lysholm score, with less improvement in older patients.18
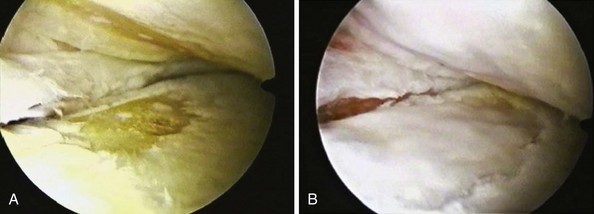
Figure 8–1 Degenerative chondral defects before microfracture (A) and after microfracture (B).
(Photos courtesy of Dr. William Sterett, Steadman-Hawkins Clinic, Vail, CO.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









