TABLE 33-1 SEDDON’S CLASSIFICATION OF NERVE INJURY | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
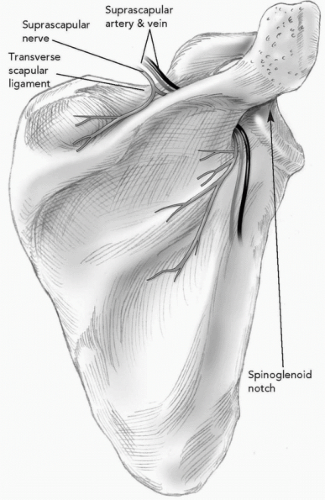 Figure 33-1 Suprascapular nerve passes below the transverse scapular ligament and around lateral margin of the scapular spine (spinoglenoid notch). |
TABLE 33-2 CAUSE OF SUPRASCAPULAR NEUROPATHY | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
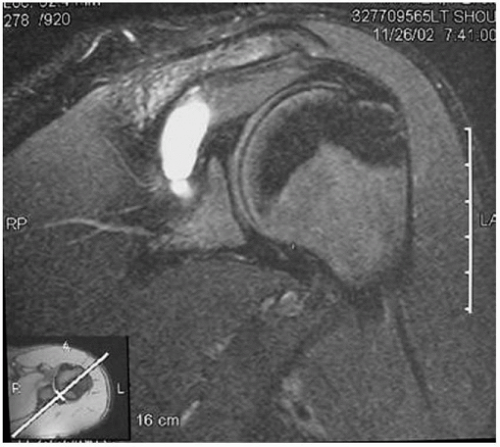
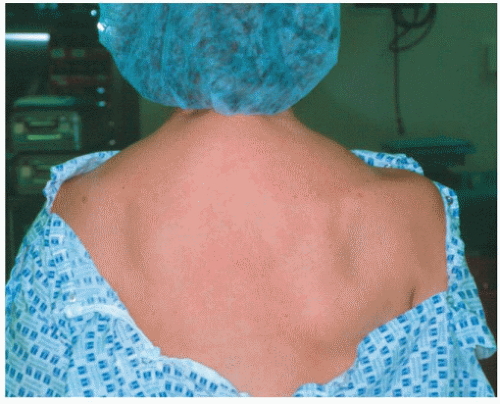 Figure 33-4 A 30-year-old woman with right suprascapular notch neuropathy and diffuse atrophy of both the supraspinatus and infraspinatus muscles. |
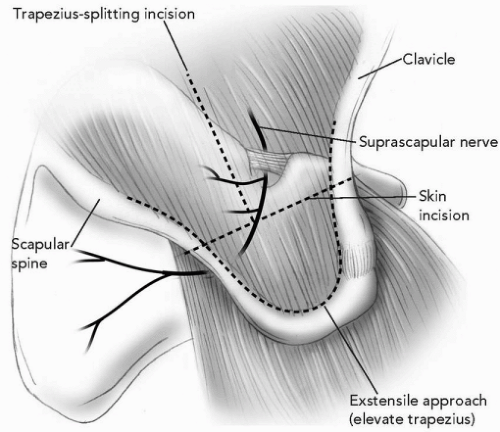 Figure 33-5 Superior trapezius-splitting approach for decompression of suprascapular notch neuropathy. |
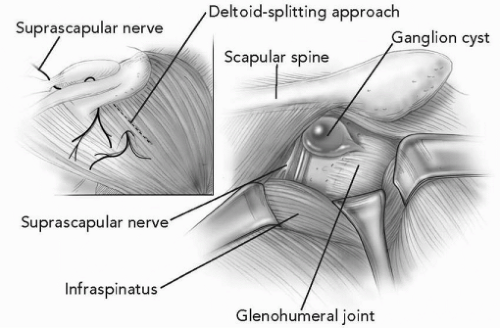 Figure 33-6 Posterior approach to the shoulder for isolation of the suprascapular nerve and excision of glenohumeral cyst. |
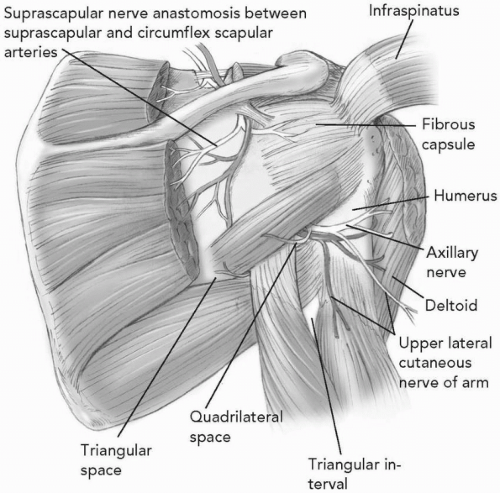 Figure 33-7 Posterior view of quadrilateral space with axillary nerve and posterior humeral circumflex artery. |
TABLE 33-3 CAUSE OF AXILLARY NEUROPATHY | ||||||||
|---|---|---|---|---|---|---|---|---|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree