Fig. 10.1
This lateral radiograph demonstrastes anterior and posterior spinal instrumentation after excision of giant cell tumor of T1
Fig. 10.2
This axial CT demonstrates lytic changes in the posterior elements of T1 (arrows)
After positioning the patient in the operating room an intra-operative CT was obtained and the patient’s tumor was mapped prior to making the skin incision. The navigation helped to determine the optimal position for the incision (Figs. 10.2 and 10.3). In this case the smaller incision was ideal for a tubular retractor system (Fig. 10.4). Again, the navigation allowed for the use of a smaller incision by helping to determine the best trajectory needed to access the tumor while avoiding the hardware already in place. Once the incision was made the navigation helped to guide the burr used to remove the tumor. The navigation probes were used frequently during the surgery to determine exactly how much bone/tumor to remove (Figs. 10.5, 10.6, and 10.7). A post-operative CT demonstrates the extent of resection most clearly (Fig. 10.8).
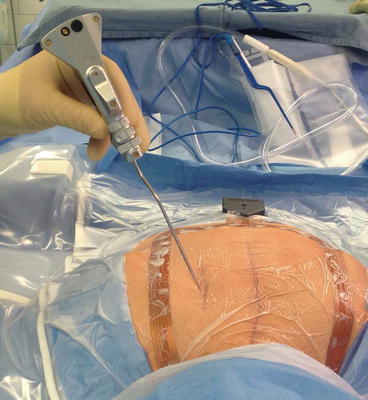
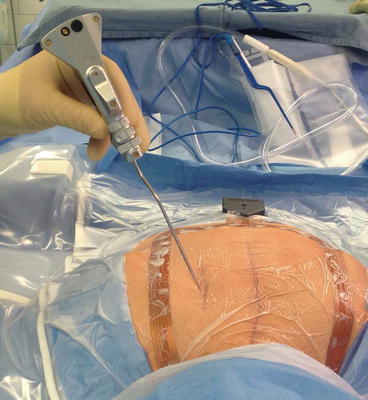
Fig. 10.3
This intra-operative photograph shows the navigation probe being used to help localize the lytic disease so that the incision can be made precisely at the level of the tumor
Fig. 10.4
This intra-operative navigation image shows the head of the probe over the lytic area in the bone. The probe appears to be in the subcutaneous tissues however, the probe is actually on the skin rather in the tissue
Fig. 10.5
This intra-operative photograph shows the placement of a tubular retractor system through a small incision centered over the T1
Fig. 10.6
This intra-operative navigation image shows the probe in the area of the lytic disease. In this case the area proximal to the tip of the probe has been removed with the drill. The navigation probe provides information regarding how much more bone should be removed as well as how close one is to the spinal canal. It also allows one to avoid the posterior instrumentation
Fig. 10.7
This intra-operative photograph shows the drill being used to remove bone through the tubular retractor system
Fig. 10.8
This intra-operative photograph shows the navigation probe within the tubular retractor system. It also shows the navigation image in the same field allowing the reader to appreciate where the probe is relative to the lytic disease in the spine
Another situation where navigation can be useful is where percutaneous implants are utilized. Fluoroscopic images are the standard method by which to insert these screws and it is a reliable method. However, CT based navigation is also quite useful and can decrease operative time and radiation exposure to the surgeon.23883830 Fluoroscopy guided percutaneous screw placement requires the insertion of a guide wire over which the screw is inserted (Figs. 10.9, 10.11, 10.12, 10.13, and 10.14). Screws can be placed reliably using this method. One or dual C-arms can be used to obtain biplaner fluoroscopic images. Alternatively, three dimensional fluoroscopic images can be obtained with more specialized equipment.
Fig. 10.9
This is a post-operative axial CT which shows complete removal of the lytic area (arrow) and surrounding bone in T1
Fig. 10.10
This intra-operative navigation image reveals the navigation probe with a phantom screw attached to it’s tip so that it can be used as a template
Fig. 10.11
This anterior/posterior fluoroscopic image reveals a Jamshidi needle in a thoracic pedicle
Fig. 10.12
This lateral fluroscopic image shows a guide wire in the pedicle and vertebral body of a thoracic vertebrae