Nausea and Vomiting (Case 20)
Owen Tully MD and Bob Etemad MD
Case: A 65-year-old woman presents with nausea and vomiting. She has a past medical history of hypertension, hyperlipidemia, type 2 diabetes mellitus, mild obesity, and a recent diagnosis of a herniated lumbar disk; her surgical history includes a hysterectomy for fibroid disease. She states the nausea and vomiting has been worsening for 3 days, usually after meals, and is associated with crampy abdominal pain before these episodes. She was recently seen by her primary physician, who added glipizide to her medical regimen because her hemoglobin A1c (HgbA1c) was not well controlled. She has also recently been started on a fentanyl patch for worsening pain in her cervical spine secondary to her herniated disk.
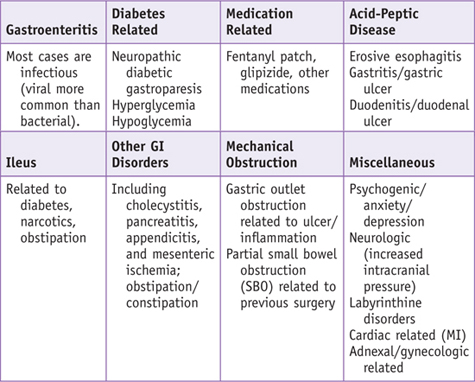
Differential Diagnosis
When a patient presents with symptoms of nausea and vomiting, it is important to consider that some patients may vomit and have minimal nausea, whereas others present with long durations of nausea punctuated with a rare episode of vomiting that does not relieve the nausea. Among the more important factors to consider are the following:
 Are the symptoms acute or chronic? Acute nausea or vomiting usually suggests a more urgent issue.
Are the symptoms acute or chronic? Acute nausea or vomiting usually suggests a more urgent issue.
 Is there any possibility of pregnancy?
Is there any possibility of pregnancy?
 Are there other signs or symptoms that the patient is significantly ill?
Are there other signs or symptoms that the patient is significantly ill?
PATIENT CARE
Clinical Thinking
• In any woman of childbearing age, be sure to exclude pregnancy.
• Determine the time frame of symptoms. If the symptoms are roughly 1 month or less, an acute cause of the symptoms should be considered, as catastrophic and more dangerous etiologies tend to manifest acutely.
History
• Perform a detailed review of systems to consider the multitude of other etiologies.
Physical Examination
• Abnormal vital signs suggest a more concerning process needing more urgent attention.
• General appearance: Is the patient “miserable” or comfortable? Is there something obvious that strikes you as concerning (distended abdomen, lying in fetal position, abnormally quiet, not moving a particular extremity)? Does the patient appear ill?
• Check for signs of volume depletion by examining the oral mucous membranes, eyes, and skin.
• Lymphadenopathy could suggest either infectious causes or malignancy.
• Signs of muscle atrophy, cachexia, and temporal wasting could suggest malignancy.
• Peripheral neuropathy can be seen in patients with or without diabetic gastroparesis.
Tests for Consideration
$11 | |
$12 | |
$9 | |
$4 | |
$19 | |
• Esophagogastroduodenoscopy (EGD): Evaluate for gastritis, esophagitis, peptic ulcer disease (PUD). | $600 |
$27 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


 Does the patient have a chronic medical condition in which nausea or vomiting may be a manifestation of a life-threatening complication of that condition (cardiovascular disease, diabetes, neurologic disorder, active malignancy)?
Does the patient have a chronic medical condition in which nausea or vomiting may be a manifestation of a life-threatening complication of that condition (cardiovascular disease, diabetes, neurologic disorder, active malignancy)? What is the relationship between the patient’s nausea and his or her vomiting? Timing, duration, exacerbating factors, associated symptoms, and new medications must be considered.
What is the relationship between the patient’s nausea and his or her vomiting? Timing, duration, exacerbating factors, associated symptoms, and new medications must be considered.
