3 Myofascial trigger points and other reflex phenomena
Pain patterns
The radiating and/or referred symptoms deriving from myofascial trigger points are a major cause of sustained pain and dysfunction, according to Wall & Melzack (1989), the leading researchers into pain. Trigger points are indeed stated by them to be a part of all chronic pain conditions, often the major part. To be sure there are many other descriptions and classifications of reflex pain patterns – many of which are outlined in the following chapters – and these demand a brief review of the possible mechanisms involved.
Difference between referred phenomena and radicular pain
The key characteristics of radicular dysfunction from, for example, a herniated disc, will include (Lavelle et al 2008, Fairbank 2008, Dvorak & Dvorak 1984):
• pain located in the regions supplied by the nerve roots from the segment(s) involved
• a loss of sensitivity in the appropriate dermatomes related to the segment(s) involved
• a loss of motor power – possibly to the point of paralysis – of the muscle innervated by the nerve roots involved, and possible atrophy
• disturbances of the deep tendon reflexes in the related areas. Diagnosis of the presence of such dysfunction requires expert neurological assessment; however, practitioners and therapists should be aware of these key signs, which alert them to the possibility that nerve root syndromes may be a feature of the patient’s problem.
Historical perspectives on non-radicular patterns of referred pain
Five variations
Dvorak & Dvorak (1984) have described five variations on the theme of referred symptomatology, different ways of seeing the same phenomena, aside from nerve root syndromes. These are:
1. Referred pain – which includes the findings described by researchers such as Lewis (1938), Kellgren (1938), Hockaday & Whitty (1967), who demonstrated that mechanical and chemical stimulation to various spinal structures produces referred pain. This is discussed further in this chapter.
2. Myofascial trigger points, which are discussed extensively in this chapter, and which form the major focus of neuromuscular technique application in North America.
3. Pseudoradicular syndromes, which Brugger (1962) describes as being quite distinct from root syndromes and which derive from a ‘nociceptive somatomotoric blocking effect’ occurring in tissues such as joint capsules, tendon origins and other local (to joint) tissues. These painful reflex effects are noted in muscles and their tendinous junctions as well as the skin – which Brugger calls ‘tendomyosis’ – defined as, ‘the reflexogenic functional change in the muscle in the presence of concurrent functionally dependent muscle pain’. Dvorak & Dvorak (1984) include in this category of referred pain and symptoms the phenomena of viscerosomatic and somatovisceral influences, in which, for example, organ dysfunction is said to produce tendomyotic changes (Korr 1975). Some aspects of these phenomena form part of the discussion of facilitation in this chapter.
4. Tender points, as described by Jones (1981), which Dvorak & Dvorak equate with the tender points described by Kellgren (1938) (see Ch. 4 for more on Jones’ work), are seen to be spontaneously arising areas of tenderness related to acute or chronic strains, usually located in those soft tissues shortened at the time of the strain. These seem to equate with so-called ‘Ah shi’ points in traditional Chinese acupuncture methodology (i.e. points not necessarily present on acupuncture meridian maps, but occurring spontaneously in association with strain in the region).
5. Spondylogenic reflexes, knowledge of which Dvorak & Dvorak describe as being based on empirical clinical observation that demonstrates relationships between the axial skeleton and the peripheral soft tissues which ‘are not easily explained on the basis of radicular, vascular or humoral reasoning’. The effects of these reflexes include ‘demonstrable zones of irritation … which are painful swellings, tender upon pressure, located in the musculofascial tissue in topographically well-defined sites’ (Sutter 1975).
Dvorak & Dvorak (1984) suggest that these different classifications and descriptions are focusing on the same phenomena, with terminology and interpretations being the variables, rather than there being a host of different physiological patterns of response to stress and trauma.
Speransky
Speransky, in his classic book A Basis for the Theory of Medicine (Speransky 1943), demonstrated clearly that ‘From any nerve point it is easy to bring into action nerve mechanisms, the functioning of which terminates at the periphery, in changes of a bio-physico-chemical character.’ And further: ‘Justification exists for the thesis that any nerve point, not excluding peripheral nerve structures, can become the originator of neurodystrophic processes, serving as the temporary nerve centre of these processes.’
 Kellgren
Kellgren
Following on from the pioneering work of Sir Thomas Lewis, the researcher J. H. Kellgren performed a series of studies in the late 1930s which deserve our attention since he clearly identified the character and nature of what became known as ‘myofascial trigger points’ (Kellgren 1938, 1939, Lewis 1938).
Kellgren (1938) effectively showed (using himself and volunteers) that by irritating fascia and muscle he could produce referred sensations in other structures. For example, among his early findings was evidence that a saline injection into the occipital muscles would produce a headache, while similar irritation to the masseter muscle produced a toothache.
Kellgren (1939) concluded that such distribution of pain usually followed segmental pathways, although he modified this position when he applied his studies to clinical work, at which time he not only identified localized, exquisitely painful spots that referred painful symptoms to distant areas, but also noted that the distribution of pain from such spots did not in fact always follow peripheral neural pathways. He also showed that a local anaesthetic injection into such spots could obliterate the referred pain sensations.
Kellgren (1939) stated:
Additional research at that time (1940s) indicated that there was not always a predictable pattern of pain distribution from such experiments (Feinstein et al 1954) (Fig. 3.1).
Dittrich
Dittrich (1954) has shown a constant pattern of fibrosis of subfascial tissue, with adhesions between this and the overlying muscle fascia, in a number of distinctive and common pain patterns. For example, in what he calls the ‘mid-sacral syndrome’ which develops from sacral lesions, referred pain is almost always present in the buttock and sometimes in the thigh, leg or foot. Referred tenderness is elicited in the lower part of the buttock. The fibrous adhesions (trigger area) are found at the level of the 3rd sacral vertebra, near the spine.
The presence of ‘fibrosed subfascial tissue’ supports the theories of Stanley Lief and Boris Chaitow, and their use of NMT in treating such problems (see Ch. 2). The locale of these, close to bony insertions, further supports the rationale behind neuromuscular technique application.
It seems that soft tissue lesions, characterized by fibrosis of subfascial tissue (fat, etc.) with fibrous connections between the structure and the overlying fascia, can initiate sensory irritation that produces referred pain and tenderness. In addition, autonomic nervous involvement may be activated to produce vasomotor, trophic, visceral or metabolic changes. Symptoms will disappear when the offending lesion is normalized, by whatever method. However, a system that both corrects the offending trigger and attempts to prevent its recurrence would seem to offer greater clinical benefits. Before surveying some of the other reflex patterns that are pertinent to this text, a brief summary of current thinking on the aetiology of muscle pain, as described by Mense & Simons (2001) is provided in Box 3.1.
Box 3.1 Mense & Simons perspective on muscle pain
In Chapter 1 a brief overview (see ‘Modern pain concepts’) was provided of how muscle pain evolves, as described by Mense & Simons (2001). In this section some of the major causes of muscle pain are outlined, based on the same researchers’ descriptions and discussions.
Local muscular pain
Metabolic causes of local muscle pain include enzyme deficiencies and hypothyroid status that ‘compromise oxidative metabolism in the muscle mitochondria’ (Mense & Simons 2001). Inflammatory process may result from injury or infection (e.g. Staphylococcus aureus) or infestation (e.g. trichinosis caused by Trichinella spiralis deriving from undercooked meat such as pork).
Local muscle pain resulting from compartment syndrome may result from development of a haematoma, oedema or infection in a muscle surrounded by a fascial envelope (such as flexor digitorum longus muscle in the deep posterior compartment). Surgical intervention may be called for to relieve the pressure before irreparable tissue damage occurs. A similar scenario may result from a plaster cast applied too tightly. Rarely toxicity-induced myalgic pain may derive from contaminated tryptophan, a sleep-inducing and pain-relieving amino acid, useful in the treatment of fibromyalgia. As pure tryptophan is no longer available because of contamination in the manufacturing process following a Japanese attempt to modify genetically the bacteria used in its production, tryptophan is now available in a plant-derived form, free of contaminants, as 5-hydroxytryptophan (Chaitow 2000).
Nerve lesion or dysfunction
Neuropathic muscle pain derived from a nerve lesion or dysfunction in the cranial (spinal) or dorsal root nerves. Causes may be mechanical (trauma) or entrapment (see notes on Maitland, Butler and Gifford in Ch. 1), or as a result of the development of a neuroma, which can lead to phantom pain. Pain from a herniated disc is an example of radicular pain. Peripheral neuropathies may occur in conditions such as diabetes. The causes of widespread pain conditions, which also involve autonomic symptoms, such as complex regional pain syndrome (previously called reflex sympathetic dystrophy), are thought to involve the sympathetic nervous system in an as-yet unknown way.
Referred pain
Pain that is referred to and from muscles can be confusing. Mense & Simons (2001) use the term ‘mislocalization of pain’, in which ‘the muscle in which the pain is felt serves only as a starting point for finding the source of pain, which is really what requires treatment’. The mechanisms are not clear, although the phenomenon is at the very heart of the pain often found to derive from distant trigger point activity. Mense & Simons indicate that there are confusing influences from trigger points when they reflexly influence other structures: ‘Why trigger points cause reflex spasm in one situation and reflex inhibition in another is not at all clear. One possibility is that the distinction between muscles prone to tightness (postural – see Ch. 1) and muscles prone to weakness (phasic – see Ch. 1) may be of fundamental physiologic significance.’ What is known is that specific dermatome and myotome distribution of sensations is not constant in relation to the symptoms produced by an active trigger point. Discussion in this chapter on the phenomena of local and segmental facilitation, and also of viscerosomatic reflex activity, covers aspects of this form of reflexogenic and referred pain.
Muscular tension
Pain deriving from muscular tension may involve biomechanical rather than neural influences. Factors such as the viscoelastic tone and the colloidal nature of soft tissues involving thixotropic qualities, as well as non-neurologically mediated contractures, may be present (see notes on fascia in Ch. 1).
This topic is complex and the reader is referred to Mense & Simons (2001, Ch. 5) for greater detail.
Other reflexogenic models
Gutstein
Gutstein (1956) showed that conditions such as ametropia may result from changes in the neuromuscular component of the craniocervical area, as well as from more distant conditions involving the pelvis or shoulder girdle. He states:
Normalization of these muscles by manipulation relieves eye symptoms as well as fascial, dorsolumbar and abdominal tenderness. Gutstein terms these reflexes ‘myodysneuria’ and suggests that the reference phenomena of such spots or triggers would include pain, modifications of pain, itching, hypersensitivity to physiological stimuli, spasm, twitching, weakness and trembling of striated muscles; hypertonus or hypotonus of smooth muscle of blood vessels, and of internal organs; hypersecretion or hyposecretion of visceral, sebaceous and sudatory glands. Somatic manifestations may also occur in response to visceral stimuli of corresponding spinal levels (Gutstein 1944).
Many such trigger areas are dormant and asymptomatic. Gutstein’s method of treatment was the injection of an anaesthetic solution into the trigger area. He indicated, however, that, where accessible (e.g. muscular insertions in the cervical area), the chilling of these areas combined with pressure yielded good results. This is in line with Mennell’s work (1975), and fits into the field of NMT.
Amongst the patterns of vasomotor sebaceous, sudatory and gastrointestinal dysfunction mentioned by Gutstein (1944a) are the following, all of which relate to reflex trigger points or ‘myodysneuria’ (fibrositis/fibromyalgia):
1. Various patterns of vasomotor abnormality such as coldness, pallor, redness, cyanosis, etc. These variations in response to stimulation relate to the fact that most organs respond to weak stimuli by an increase in activity and to very strong stimuli by inhibiting activity. Menopausal hot flushes are one example, and these seem often to be linked to musculoskeletal pain. Gutstein found that obliteration of overt and silent triggers in the occipital, cervical, interscapular, sternal and epigastric regions was accompanied by years of alleviation of premenopausal, menopausal and late menopausal symptoms. Proponents of NMT have long emphasized the importance of normalizing these very structures.
2. Gutstein maintains that normalization of skin secretion, and therefore of hair and skin texture and appearance, may be altered for the better by the removal of active trigger areas in the cervical and interscapular areas.
3. The conditions of hyperhidrosis, hypohidrosis and anhidrosis may accompany vasomotor and sebaceous dysfunction. Gutstein noted that abolition of excessive perspiration as well as anhidrosis followed adequate treatment.
4. Gutstein quoted a number of practitioners who have achieved success in treating gastrointestinal dysfunctions by treating trigger areas. Some of these were treated by procaine injection, others by pressure techniques and massage. The abdominal wall lends itself to the latter procedure, as evidenced by the work of Cornelius (1909), whose treatment was not dissimilar to Lief’s NMT.
Among the conditions that have responded to such treatment are pylorospasm, bad breath, heartburn, regurgitation, nausea, abdominal distension, constipation and nervous diarrhoea. Gutstein (1944b) called localized functional sensory and/or motor abnormalities of musculoskeletal tissue (comprising muscle, fascia, tendon, bone and joint) myodysneuria (now known as fibromyalgia; formerly known as ‘fibrositis’ and ‘muscular rheumatism’).
He viewed the causes of such changes as multiple; among them are:
1. Acute and chronic infections which, it is postulated, stimulate sympathetic nerve activity via their toxins.
2. Excessive heat or cold, changes in atmospheric pressure, and draughts.
3. Mechanical injuries, both major and repeated minor microtraumas. Postural strain, unaccustomed exercises, etc., which may predispose towards future changes by lowering the threshold for future stimuli (facilitation).
4. Allergic and endocrine factors, which can cause imbalance in the autonomic nervous system.
5. Inherited factors that make adjustment to environmental factors difficult.
6. Arthritic changes – because muscles are the active components of the musculoskeletal system it is logical to assume that their circulatory state has influence over bones and joints. Spasm in muscle may contribute towards osteoarthritic changes, and such changes may produce further neuromuscular changes, which themselves produce new symptoms.
7. Visceral diseases may intensify and precipitate somatic symptoms in the distribution of their spinal and adjacent segments.
Diagnosis of myodysneuria was made according to some of the following criteria:
• A varying degree of muscular tension and contraction is usually present, although sometimes adjacent, apparently unaffected, tissue is more painful.
• Sensitivity to pressure or palpation of affected muscles and their adjuncts.
• Marked hypertonicity may require the application of deep pressure to demonstrate tenderness.
Travell and Bigelow
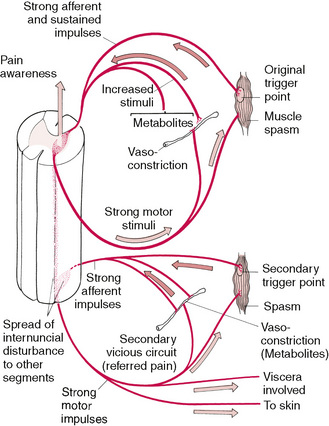
Travell & Bigelow (1947) produced evidence to support much of what Gutstein had reported. They indicated that high-intensity stimuli from active trigger areas produced, by reflex, prolonged vasoconstriction with partial ischaemia in localized areas of the brain, spinal cord or peripheral nerve structures (Fig. 3.2). A wide pattern of dysfunction might result, affecting almost any organ of the body. The phenomenon of hysteria, with symptoms as varied as disordered vision, respiration, motor power and cutaneous sensation, was often mediated by afferent neural impulses from trigger areas in skeletal muscle. These triggers, when similarly located, produced the same pattern of clinical effects, whether activated in one patient by psychogenic factors or in another by different factors (e.g. mechanical or traumatic).
It is worth noting that Travell (1981) has shown that the effect of a trigger point on the muscle housing it is to produce weakness of contraction without atrophy, and that this is often accompanied by a decreased range of movement in associated joints.
Dowling
Dowling (2000) has described a variation on the use of inhibitory pressure (see Box 3.5), which allies itself closely with the methods of NMT and other soft tissue approaches utilizing the effects of compression in a physiologically useful manner. Using two points of contact, progressive, sequential pressure applications are used to inhibit pain and modify function. Dowling’s work fits well with other approaches (acupressure, strain/counterstrain, use of neurolymphatic reflexes, etc.) that depend on the underlying mechanisms that allow manual input to modify neuromuscular function and pain. See Chapter 11 for a full explanation of progressive neuromuscular inhibition technique (PINS).
Central sensitization (see Fig. 3.3)
All these historical perspectives are describing, in one way or another, what is now known as peripheral and central sensitization. In osteopathic medicine the evolution over time of hypersensitivity and reactivity in neural structures, is known as facilitation, and this is described later in this chapter (Korr 1970).
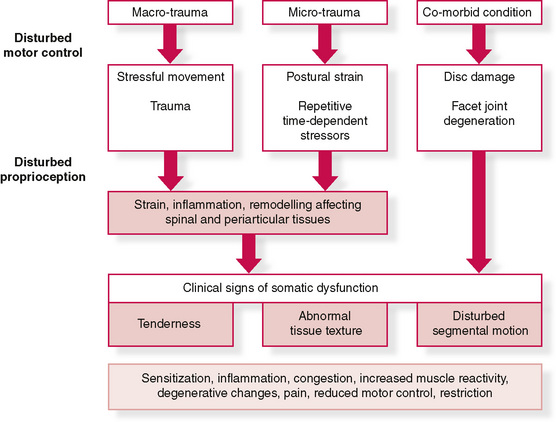
Figure 3.3 Diagram showing possible aetiological pathways to somatic dysfunction and sensitization
Modified from Fryer G, Fossum C. Possible etiology of somatic dysfunction. In: Physical Therapy for tension type and cerviocogenic headache. Fernández de las Peñas C., Arendt-Nielsen L., Gerwin R. (Eds): Jones & Bartlett, Boston, 2009.
Sensitization may underlie both adaptive as well as maladaptive learning processes for the organism. This process is also known as long-term potentiation, and involves complex biochemical changes in the tissues involved (Ji et al 2003, McEachern et al 1999).
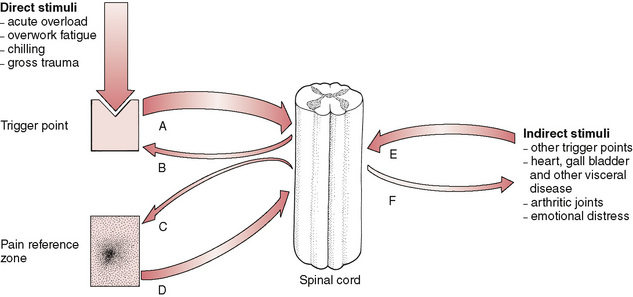
Understanding facilitation
To understand trigger points, we need to understand spinal facilitation first. Facilitation occurs in both spinal and paraspinal tissues (segmental facilitation) as well as in discrete local areas of muscles, mainly near their origins and insertions but also close to their bellies and in areas where fascial stress occurs due to external influences and forces (myofascial trigger points). Understanding facilitation helps us to see how the different classification systems, all describing variations on the same phenomenon of referred pain – listed by Dvorak & Dvorak (1984) and described earlier in this chapter – are held together aetiologically.
Patterson (1976) explains segmental (spinal) facilitation as follows:
A facilitated segment therefore emerges from a prolonged period during which abnormal or altered inputs from a single source (or more than one source) of irritation, impinging on the spinal cord, keep the interneurons or motor neurons of that spinal segment in a constant state of excitement, thus allowing normally ineffectual inputs to produce outputs to all organs receiving innervation from the excited area. This concept implies that the spinal cord is a relatively passive mediator of the influences imposed on it and that the neural paths act as communicators of that activity (Denslow et al 1949).
Research on spinal functions seems to indicate, however, that the spinal cord, besides being the determiner of where abnormal activity is sent, by virtue of predetermined pathways, may participate actively in either controlling abnormal or unusually intense inputs, or amplifying and retaining such inputs in certain circumstances (Korr 1986).
Initially, only intensities of afferent input above a certain level would result in increased sensitivity of the spinal pathway. Inputs of lower intensity would either produce no alterations, or would cause an actual decrease in sensitivity as a protective mechanism against undue changes in homeostatic processes. It is apparent that the potential for sensitization by different types of afferent inputs may differ widely. Thus, inputs from pain receptors may sensitize the pathway at low levels because of the properties of the initial synapses between pain afferent fibres and interneurons. In this event an initially protective increase in response might occur, followed eventually by detrimental facilitation of a segment. On the other hand, inputs from joint receptors seem to have a less dramatic effect at similar input levels (Dowling 1991).
It is now known that emotional arousal would also affect the susceptibility of the pathways to sensitization (Baldry 1993). The increase in descending influences from the emotionally aroused subject would result in an increase in toxic excitement in the pathways and allow all additional inputs to produce sensitization at low intensities. Thus, highly emotional people, or those in a highly emotional situation, would be expected to show a higher incidence of facilitation of spinal pathways.
A further corollary of the hypothesis is that slowly developing conditions, or slowly increasing inputs, would result in less sensitization at high levels than sudden inputs. A process known as ‘wind-up’ can be part of sensitization, with the rate of stimulus, as well as the size of stimuli, determining how rapidly the process evolves. If noxious stimuli occur rapidly, the degree of stimulus required to produce symptoms (pain mainly) decreases (Codere et al 1993, Li 1999).
Windup is just such a mechanism that is thought to operate in fibromyalgia where relatively minor stimuli can produce symptoms that appear to be proportionately excessive (Staud 2006).
Korr
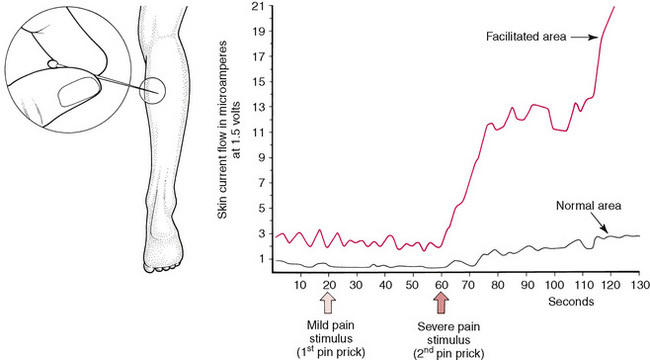
The premier researcher into facilitation over the past half-century has been Irwin Korr (Korr 1970, 1976). In early studies he demonstrated, for example, that if readings were taken of resistance to electricity in the paraspinal skin of an individual there were often marked differences, with one side showing normal resistance and the other showing reduced resistance (facilitated area).
When ‘stress’ was applied elsewhere in the body and the two areas of the spine were monitored, it was the area of facilitation, where electrical resistance was reduced, that showed a dramatic rise in electrical (i.e. neurological) activity. In one experiment, volunteers had pins inserted into one calf muscle in order to gauge the effect in the paraspinal areas under investigation – with the spinal areas being monitored for electrical activity. Almost no increase occurred in the normal region, but the facilitated area showed enormously enhanced neurological activity after 60 seconds (Korr 1977) (Fig. 3.4).
In many instances involving spinal segmental facilitation there is a chronic degree of neurological bombardment resulting from internal organ dysfunction. For example, it is almost always possible to predict that cardiovascular disease is present (or will soon be present) when two or more segments of the spine in the region of T2, T3 and T4 display tense, rigid, ‘board-like’ characteristics on palpation, especially if these tissues do not respond to normal efforts to reduce their hypertonicity (Beal 1983).
Tension headache as an example of facilitation
Danish research (Bendtsen 2000) suggests that there exists:
Viscerosomatic reflexes
Beal
Myron Beal (1985) has described this phenomenon as resulting from afferent stimuli, arising from dysfunction of a visceral nature. The reflex is initiated by afferent impulses arising from visceral receptors, which are transmitted to the dorsal horn of the spinal cord, where they synapse with interconnecting neurons. The stimuli are then conveyed to sympathetic and motor efferents, resulting in changes in the somatic tissues, such as skeletal muscle, skin and blood vessels.
The first signs of viscerosomatic reflexive influences are vasomotor reactions (increased skin temperature), sudomotor (increased moisture of the skin), skin textural changes (e.g. thickening), increased subcutaneous fluid and increased contraction of muscle. The value of light skin palpation in identifying areas of facilitation cannot be too strongly emphasized (Lewit 1992).
Patterns of somatic response will be found to differ from person to person, and to be unique, in terms of location, the number of segments involved, and whether or not the pattern is unilateral or bilateral. The degree of intensity will also differ, and is related to the degree of acuteness of the visceral condition (Hix 1976). Research involving animals, as well as observations in humans, using regional nerve blocks, has helped to define site locations of response, in various forms of visceral dysfunction. Beal (1985) notes that, when the voluminous research into segmental associations with organ dysfunction is compounded, three distinct groups of visceral involvement are found in respect of particular sites:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree