18 Myofascial Trigger Point Treatment Relevant physiologic and treatment principles for manual trigger point techniques have been described in Chapter 2. • Pain referral pattern: Occiput; temporal and parietal region on the same side asthe incriminated trigger point (a). I Motion restriction: Maximal flexion (inclination) at C0–C1 with the cervical spine extended is usually restricted. • Palpatory localization: The rectus capitis major and minor can be palpated through the thin layers of the trapezius and splenius muscles. The muscle bellies are large and prominent. The trigger points (TPs) can only be assumed (b). • The patient is sitting. • The physician stands behind the patient and introduces appropriate motion of the head and cervical spine. Technique I: Active, repetitive muscle contraction and relaxation. Compression of the trigger point (TP), while small flexion–extension motions are repetitively performed (b, c), specifically addressing the C0–C1flexion (inclination) and extension (reclination) motions. Technique II: Stroking massage of connective tissue. Localized stretching of the muscle portion containing the trigger point (at its painful location) following along the direction of the muscle fibers. The preparation/set-up stretch should not be excessive because otherwise one is unable to advance to the deeper trigger points. Technique III: “Fascial release.” Introduction of lateral stretch applied to muscle belly below the inferior nuchal line. Technique IV: Myofascial release (“fascial separation”). Release (“separation”) of the fascia between the following muscles: the suboccipital muscles and the area medial to the semispinalis capitis muscle and lateral to the border to the longissimus cervicis muscle. In the presence of somatic dysfunctions with motion restriction at the C0–C1 and C1–C2 levels, address the sub-occipital muscles before applying other maneuvers. • Pain referral pattern: Pain may be localized to the sub-occipital region; pain may also be referred to the temporal region (a). • Motion restriction: Cervical rotation to the opposite side is restricted. The transverse process of the atlas (insertion) moves away from the spinous process of the axis (origin). • Palpatory localization: The muscle can only be palpated when it is tight (e. g., “spasm”) (b). • The patient is seated upright with the head being rotated slightly to the opposite side. I The physician stands behind the patient and monitors the patient’s motion with one hand. Technique I: Active, repetitive muscle contraction and relaxation. The trigger point is compressed by the physician’s finger, which pushes “through” the trapezius and splenius capitis muscles. The patient is instructed to repetitively rotate his head and neck to either side (b, c). Technique II: Stroking massage of connective tissue. Localized stretching of the muscle portion containing the trigger point (at its painful location) following along the direction of the muscle fibers. The preparatory stretch should not be excessive because otherwise one is unable to advance to the deeper trigger points. Skin and underlying tissues should be treated simultaneously, that is, the skin should not be displaced with respect to the muscle. Technique III: “Fascial release.” Usually this technique cannot be applied to the obliquus capitis inferior muscle. Technique IV: Myofascial release (“fascial separation”). Usually this technique cannot be applied to the obliquus capitis inferior muscle. Notes: • The trigger point treatment of the obliquus capitis inferior muscle is well suited as preparation for mobilization-with-or -without-impulse techniques directed to the C1–C2 articulation. • The muscle can also be stretched utilizing the NMT 2 technique by introducing rotation at the C1–C2 level. • Pain referral pattern: To the occipital region and referred pain to the vertex and the temporal region. The patient often does not complain of pain in the neck region but describes a “constant pressure.” External pressure, such as when lying on a pillow, is often not tolerated by the patient (a). • Motion restriction: Flexion of the cervical spine and inclination at the C0–C1 junction may be diminished. • Palpatory localization: The trigger point can be palpated under the descending portion of the trapezius muscle. The trigger points are usually located lateral to the spinous processes of C2–C6. • The patient is seated. • The physician is standing behind the patient guiding the head. • As an alternative, this maneuver can be performed with the patient in the prone position. However, in the prone position one should assure careful and gentle positioning, especially at the level of the throat. Technique I: Active, repetitive muscle contraction and relaxation. Compression of the trigger point through the trapezius muscle with the instruction given to the patient to actively nod his head up and down (b, c). Technique II: Stroking massage of connective tissue. Stroking-type of massage applied to the area harboring the trigger point while using slight traction. Technique III: “Fascial release.” Treat the trigger point with pressure exerted through the nuchals while maintaining slight traction to the entire cervical spine. The physician stabilizes the patient’s head with one hand. Technique IV: Myofascial release (“fascial separation”). The trigger point is treated by applying pressure between the semispinalis capitis and cervicis muscles as well as between the semispinalis cervicis muscle and the fourth-layer rotator muscles. • The semispinalis muscles are frequently involved in a flexion–extension type of injury as they are often excessively stretched when the head and neck are suddenly and forcefully displaced anteriorly. • The multifidi and cervical rotator muscles are located deep in the groove between the semispinalis capitis and the longissimus cervicis muscles. They can be treated in a way similar to that described for the semispinalis capitis and cervicis muscle. • Pain referral pattern/symptoms: Anteriorly, the pain may project to the entire shoulder region and the chest. Posteriorly it may project between the shoulder blades, the lateral portion of the arm and as far distal as the hand (a). • Motion restriction: Cervical side-bending to the side opposite of the incriminated muscle is typically restricted. Specific range of motion restrictions due to involvement of the anterior or posterior scalene muscles are as follows: • Anterior scalene muscle: extension and rotation to the ipsilateral side is restricted. • Posterior scalene muscle: flexion and rotation to the opposite side is restricted. Palpatory localization: The anterior scalene muscle is palpated in the front part of the neck by going deep either anterior or lateral to the sternocleidomastoid muscle. The medial and posterior scalene muscles are best approached posteriorly from a lateral direction. • The patient is seated. • The physician stands behind the patient. With one hand placed on top of the patient’s head, he guides the patient’s head and neck into the appropriate positions. Technique I: Active, repetitive muscle contraction and relaxation. While applying slight pressure (e. g., appropriately dosed compressive force) to the localized trigger point, the physician carefully side-bends the patient’s neck to the side opposite the incriminated muscle. From this position, the patient is requested to repetitively contract and relax the muscle using a side-bending effort toward and away from the incriminated muscle. Depending on which of the three scalene muscles is involved, the technique is “fine-tuned” as specific rotation components are incorporated as well (b, c). Technique II: Stroking massage of connective tissue. After an adequate preparatory stretch has been introduced to the muscle harboring the trigger point—though always staying within the patient’s pain tolerance—adeepstroking type of massage is carefully applied to the connective tissues surrounding the incriminated trigger point. Technique IV: Myofascial release (“fascial separation”). In the lateral neck, this technique can be applied to any of the fascial planes and connections associated with the scalene muscles. A shortened anterior or medical scalene muscle can compress upon the brachial plexus leading to an entrapment situation. If the anterior portion of the scalene triangle is being compressed, the elicited pain pattern can easily be mistaken for that of irritation of the brachial plexus and thus can be misdiagnosed. • Pain referral pattern/symptoms: The pain may be referred to the ipsilateral mastoid region and the ear as well as the ipsilateral temporal region, forehead, and orbit (a). • Motion restriction: The following movements are typically restricted: cervical spine extension, side-bending to the opposite side, and rotation toward the same side as the incriminated muscle. • Palpatory localization: The trigger point in the sternal and/or clavicular portion of the muscle can be palpated with the thumb and index finger by gently squeezing the muscle in a pinch maneuver. An incriminated trigger point in the superior segment of the muscle usually reacts to the palpatory pressure by referring the pain to the occipital region and behind the ear. Palpation of a trigger point in the inferior segment of the muscle is more likely to elicit pain in the forehead and orbit. • The patient is seated. • The physician stands behind the patient and carefully guides his head. Technique I: Active/repetitive muscle contraction and relaxation: • After careful localization, the physician compresses with his index finger and thumb the muscle belly that harbors the incriminated trigger point. • The patient is then instructed to carefully extend the neck and repetitively side-bend away and toward the side of the incriminated trigger point (b). Technique II: Stroking massage of connective tissue. After an adequate preparatory stretch has been introduced to the muscle harboring the trigger point—though always staying within the patient’s pain tolerance—adeepstroking type of massage is carefully applied with the thumb on one side and the fingers on the other to the connective tissues surrounding the incriminated trigger point (c). Technique III: “Fascial release”. With the neck suitably extended, the physician carefully slides his index finger and thumb along the entire muscle from inferior to superior. Technique IV: Myofascial release (“fascial separation”). Similar to technique III. Trigger points in the sternocleidomastoid muscle have typically been associated with trauma to the cervical spine, and in particular when there are strong torsion/rotation forces involved. During the treatment of these trigger points, it is not unusual for the patient to report such symptoms as dizziness or nausea. When present and treated correctly, the patient may report that his “eye problems” (e. g., scotomata) or tinnitus have resolved. • Pain referral pattern/symptoms: The patient usually reports a painful and stiff neck. The pain is often referred to the back of the shoulder, and in particular the superior angle and the medial margin of the scapula (a). • Motion restriction: Typically, there is objective motion restriction for cervical flexion, side-bending, and rotation to the side opposite the incriminated muscle. • Palpatory localization: The muscle is best palpated at or near its inferior attachment at the scapula. After having identified the muscle mass of the trapezius (descending portion), the palpating fingers are advanced further anteriorly (e. g., in front of the trapezius) until they reach the levator scapulae muscle (b). This should be accomplished with relative ease. • The patient is seated. • The physician stands behind the patient and guides the patient’s head. Technique I: Active, repetitive muscle contraction and relaxation: • The trigger point is first localized as described above. • Palpatory pressure is maintained while the patient is instructed to move his neck, under careful guidance by the physician, into flexion, side-bending, and rotation away from the side of the incriminated muscle. Technique II: Stroking massage of connective tissue. After an adequate preparatory stretch has been introduced to the muscle harboring the trigger point—always however staying within the patient’s pain tolerance—adeepstroking type of massage is carefully applied with the thumb on one side and the fingers on the other to the connective tissues surrounding the incriminated trigger point. Technique III: “Fascial release.” After introducing an adequate preparatory stretch, the physician carefully slides his fingers along the fascial planes associated with the muscle from superior to inferior. Technique IV: Myofascial release (“fascial separation”): • With the arm on the incriminated side maximally elevated by the physician, the fingers of the treating hand advance as deep as possible both anterior and posterior to the levator scapulae muscle. • The myofascial release technique with fascial “separation” is then employed while the physician simultaneously “fine tunes” the technique by introducing applicable cervical spine rotation (c). It is the authors’ experience that trigger points in the levator scapulae muscle are quite frequently accompanied by involvement of the splenius capitis and cervicis muscles. It is therefore recommended to examine for trigger points in these muscles as well. Pain referral pattern/symptoms • Upper trapezius muscle (descending fibers): A trigger point in this portion of the trapezius muscle is one of the most commonly diagnosed points in the human body. The pain is typically referred upward and posterolaterally along the neck to the mastoid area and as far superior as the side of the head and the temple. The pain may also be referred to the orbit. The associated myofascial pain has been described as one of the most frequent causes of “tension” headache and “tension” neck-ache (a). • Lower trapezius muscles (ascending fibers): The pain is characteristically referred superiorly as far as the upper cervical spine and the suboccipital region (e. g., origin of the descending fibers of the trapezius muscle) as well as the ipsilateral mastoid region. Frequently there may be associated complaints of pain or discomfort in the ipsi-lateral suprascapular or interscapular region, or at the medial scapular border (where often it is a rather diffuse, poorly localizable pain). Motion restriction • Upper cervical spine muscle (descending fibers): When harboring a myofascial trigger point, cervical side-bending toward the opposite side is the most frequently restricted motion. When the anterior fibers are involved, cervical rotation is restricted in particular to the opposite side. When the posterior fibers are involved, cervical rotation is restricted to the same side (b). Lower trapezius muscle (ascending fibers): Motion restriction is apparent for cervical spine rotation to the opposite side. The motion restriction testing can be facilitated by having the patient cross his arms in front of him and then inducing cervical spine rotation. Palpatory localization
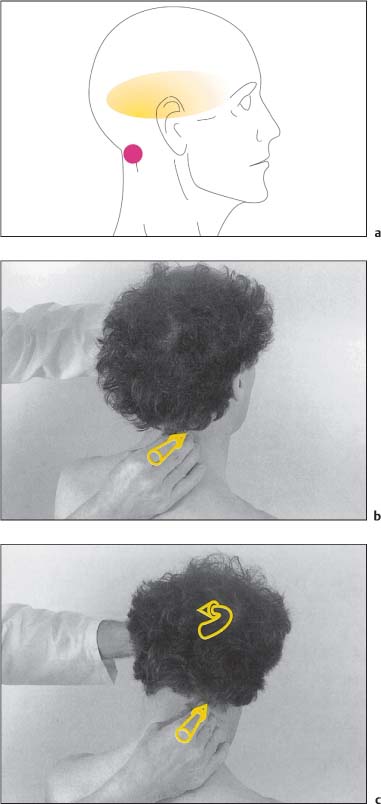
Rectus Capitis Major and Minor Muscles (Figs. I18.1a–c)
Indications
Patient Positioning and Set-up
Treatment Procedure
Comments

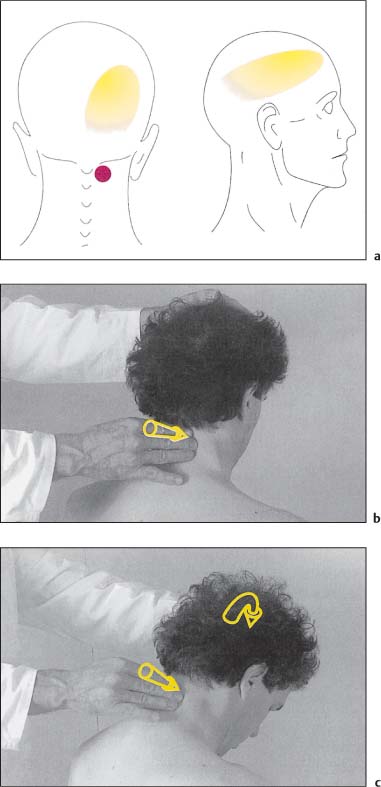
Obliquus Capitis Inferior Muscle (Figs. I18.2a–c)
Indications
Patient Positioning and Set-Up
Treatment Procedure
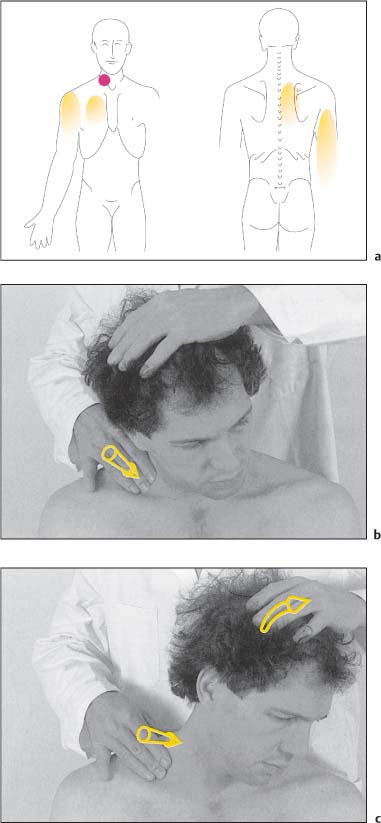
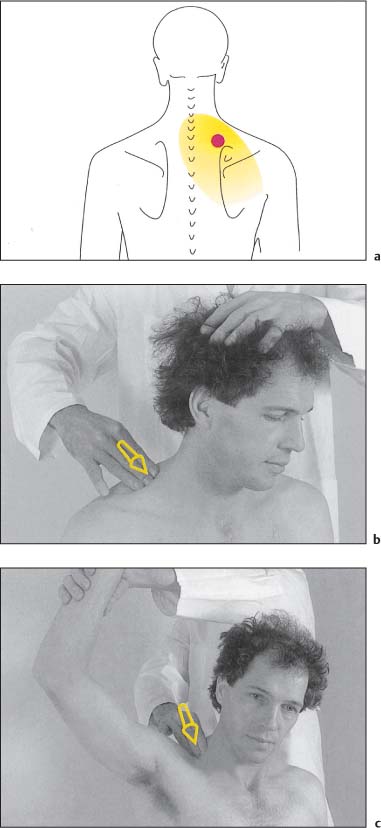
Semispinalis Capitis and Cervicis Muscles (Figs. I18.3a–c)
Indications
Patient Positioning and Set-up
Treatment Procedure
Comments
Scalene Muscles (Figs. I18.4a–c)
Indications
Patient Positioning and Set-Up
Treatment Procedure
Comments
Sternocleidomastoid Muscle (Figs. I18.5a–c)
Indications
Patient Positioning and Set-up
Treatment Procedure
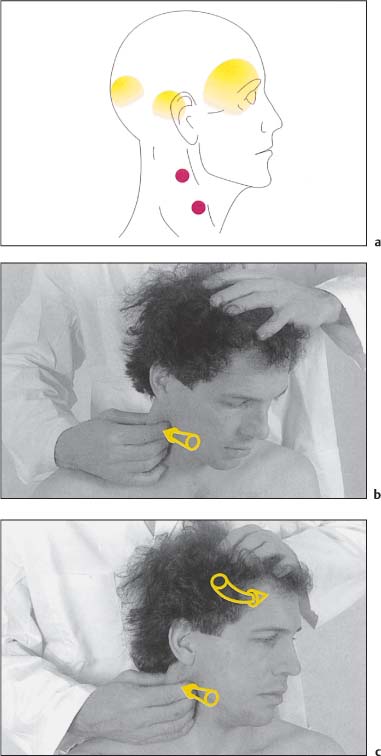
Comments
Levator Scapulae Muscle (Figs. I18.6a–c)
Indications
Patient Positioning and Set-Up
Treatment Procedure
Comments
Trapezius Muscle (Upper and Lower Trapezius) (Figs. I18.7a–d)
Indications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








