Muscle weakness and therapeutic exercise
Timothy L. Kauffman and Karen Kemmis
Introduction
Muscle weakness has long been associated with aging and is a significant factor in morbidity and loss of function. However, skeletal muscle may be considered the largest organ in the body and has new-found hormonal actions (Doria et al., 2012; Ertek & Cicero, 2012), thus the role of muscle involves more than just providing strength. Muscle is involved with movement, which is crucial for joint nutrition as well as for cardiopulmonary health. Also, muscle is related to the circulatory system, as smooth muscle supports the walls of arteries and skeletal muscle is involved in the return of venous blood. Muscle is also involved in bone health and density. It provides impetus to the nervous system, as primary sensory fibers of the muscle spindle respond to muscle length changes. A principal source of body heat comes from muscle and, additionally, it provides a cushion of compressible tissue that helps to absorb impact in the event of trauma.
Definitions
Muscle is principally noted for its roles in strength and movement. Sarcopenia is the loss of skeletal muscle mass, strength and function, and is a component of the frailty syndrome (Frontera et al., 2012) and sarcopenia may be associated with a higher risk of death (Landi et al., 2013). Strength may be defined as the tension that is generated by contracting muscle and is best expressed as a force. Torque, a result of angular displacement, is the product of force and the perpendicular distance from the line of the force’s action to the axis of rotation. Time is also a consideration for the tension that is generated and thus should be considered muscle power.
The generation of muscle tension is determined largely by the cross-sectional area of the muscle and the recruitment of motor units. Other biomechanical factors, such as muscle length and angle of displacement, and physiological factors, such as metabolism and muscle fiber type, also influence strength. Insufficient strength to perform a functional motor task should be considered weakness.
There are various types of muscle contractions. When there is no change in muscle length, a static contraction occurs, which is also referred to as isometric (same length). Dynamic contractions are a lengthening or shortening of a muscle, also called eccentric and concentric contractions respectively. Isotonic (same tone) contractions involve movement of a constant weight through a motion. Normally, raising a weight is a concentric contraction and lowering it is an eccentric contraction. When a mechanical device resists the tension generated by the contracting muscle, thereby controlling the speed of the limb’s movement, an isokinetic (same speed) contraction occurs. Isokinetic devices are essential for assessing torque at various speeds, which is clinically important because of the age-related loss of fast-twitch type II muscle fibers (see Chapter 2). This loss is one of several factors that probably contribute to the increasing inability to recover from a stumble, which results in an increased risk of injury.
Assessment
Assessment of muscle strength can be performed using a manual muscle test (MMT). Although the MMT is an ordinal scale measurement, it is invaluable because it can be performed in every treatment setting. When using the MMT, it is crucial to specify the type of contraction being performed. The original MMT was designed to be an assessment of strength throughout the available range of motion (ROM), but it has been modified in many circumstances to a ‘make’ test, in which the patient performs an isometric contraction at a specific joint position. Modification of the MMT may be especially necessary for aging patients and others who have painful arcs or restrictions in motion (Kauffman, 1982). When measuring plantar flexor strength in the weight-bearing position on one leg, Jan et al. (2005) found that men and women between 61 and 80 years of age were able to heel raise a mean of 4.1 and 2.7 times respectively. Men and women aged between 21 and 40 years were able to perform 22.1 and 16.1 repetitions respectively. Clarity in documentation is enhanced when these specifics (type of test and position) are recorded.
In contrast, a ‘break test’ is used when the patient is asked to hold the joint in a specific position and the evaluator attempts to break the tension that is generated. This changes an isometric to an eccentric contraction and is likely to generate a greater force. It should be noted that in healthy muscle, the highest tension is generated with an eccentric contraction followed by an isometric contraction, and the least tension is generated with an isotonic contraction. This is an important consideration when measuring strength with a hand-held dynamometer because a ‘make test’ is different than a ‘break test’. Caution should be used when measuring strength with the MMT in aging individuals because of the frequent necessity of modifying the test positions. In the aging patient, the test positions as enumerated in the standard manuals may have to be modified because of injury or disease. Also, a more functional position may be necessary because areas of weakness may be found only in certain positions of the joint’s ROM. These areas of weakness may be the result of joint-surface irregularities or changes in periarticular connective tissue and muscle length.
Hand-held and isokinetic dynamometers are very useful for assessing strength. Caution must be used to avoid pain in and injury to swollen areas and ulcerated or atrophied skin; the verbal extolling that frequently accompanies this testing may have to be restrained. Also, a greater risk of injury because of age-related changes in periarticular connective tissue (see Chapters 4 and 61) should be considered when dynamometers are being used.
Another strength-assessment technique described in research but almost never in the clinic is the 1RM or 10RM technique. The ‘RM’ stands for repetition maximum: a 1RM test measures the maximal weight (dynamic and isotonic) that can be moved through the ROM once, and 10RM is the maximal weight that can be moved 10 times. Some guessing is involved in determining the starting test weight, which may be too heavy or too light, and weight adjustments must be made accordingly. These techniques are safe for older patients but caution must be used during testing to avoid injury. Manor et al. (2006) reported another method of assessing strength (and really power and endurance) by using elastic bands and recording the number of complete repetitions of the joint motion that can be achieved in 30 seconds. They found that the elastic band technique was significantly correlated with a 30-second test using dumb-bells and with maximal isokinetic torque.
Perhaps more important than a frank measurement of the force of a muscle contraction is a functional assessment of motor performance, such as the ability to ascend and descend a flight of steps or to raise a 1 kg (2 lb 3 oz) can of food onto the second shelf of a cupboard. Noting that a patient was able to ascend six steps before catching a toe or failing to elevate the lower extremity would be a functional parameter of muscle performance. Endurance is an important consideration, too, especially as it relates to functional outcomes. It is one factor in the 10 RM test and is frequently measured with isokinetic devices. In activities of daily living, endurance is always a consideration; for example, carrying a full 1-gallon jug (3.6 kg [8 lb]) of water from the refrigerator to the kitchen table requires muscular strength and endurance.
Strength training
Strength training research since the 1980s has shown that the potential to increase strength is maintained in older people (Kauffman, 1985). A task force from the Section on Geriatrics of the American Physical Therapy Association has developed ‘Principles of Exercise Training in Aging Persons’, as shown in Table 16.1. The benefits of strength training with isometric, isotonic and isokinetic routines have been shown. Simple calisthenics without the use of machines are efficacious. Hypertrophy occurs even in individuals aged 90 years and above, although hypertrophy itself is not necessarily a primary objective of care; however, as noted above, muscle mass does act as a shock absorber. Functional outcomes are related to strength and motor performance and should be the objective of rehabilitation.
Table 16.1
Principles of exercise training in aging persons*
| Definition | |
| Principle | |
| Overloada | Tissue must be exposed to increased load or strain to improve function. |
| Overload applies to all aspects of the exercises prescription, including Frequency, Intensity, Time and Type (FITT principles). | |
| Overload should be applied during all forms of exercise, including aerobic capacity/endurance conditioning; or reconditioning balance, coordination and agility training; body mechanics and postural stabilization; flexibility exercises; gait and locomotion training; relaxation; and strength, power, and endurance training | |
| Specificity | The beneficial effects of exercise are primarily specific to the body part involved in the exercise, the type of exercise and/or the skill or activity performed |
| Progression | An optimal level of exercise will provide the most favorable results. As the patient/client improves, intensity of a particular exercise should be reassessed and advanced to overload the stimuli and optimize results |
| Recuperation/recovery | Training should not be rushed. The body needs recovery time to avoid undue fatigue and/or injury |
| Use/disuse | Tissue will maintain or increase function with use and lose function with disuse |
| Components of the exercise prescription | |
| Frequency | How often an exercise is performed, typically stated in times per day or days per week |
| Intensity | How hard an exercise is performed, based on the individual’s capacity |
| Time/Duration | How long an exercise is performed, typically in minutes or repetitions |
| Type/Mode | The particular exercise performed |
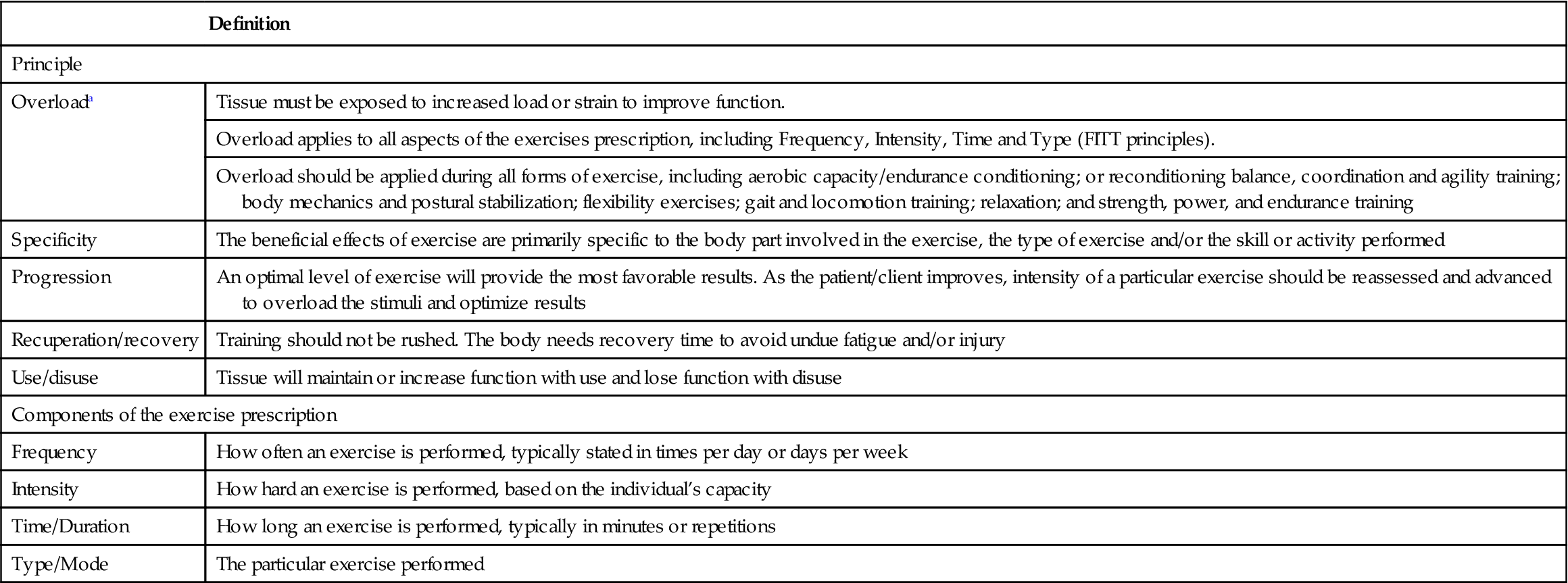
aDefinition from: American Physical Therapy Association. Guide to Physical Therapist Practice, 2nd edn. Phys Ther 2001;81:9–746.
*Adapted from Certified Exercise Experts for Aging Adults Educational Program of the Section on Geriatrics, American Physical Therapy Association, 2013.
Newman and associates (2006) reported that grip strength and isokinetic quadriceps strength were strongly related to mortality but that muscle size was not. Stenholm et al. (2012) reported similar findings. Exactly how strength and mortality are associated is unclear but these researchers suggested that the assessment of strength may measure other important aspects of the aging process. It is possible that sarcopenia and frailty, nutrition, disuse, inflammatory factors and hormonal factors related to strength, such as testosterone and insulin-like growth factor (IGF), may contribute to the strength–mortality association. For excellent reviews of the benefits of exercise on diseases, disability, performance and longevity see Warburton et al. (2006) and Kokkinos (2012).
Modifying strength training
When planning a strength training routine for geriatric patients, it is crucial to consider the need to modify the training regimen in order to accommodate pathology in the cardiopulmonary and cardiovascular systems as well as in the neuromusculoskeletal system. Guidelines for exercise in patients with heart disease are presented in Chapter 39. The aging individual is more susceptible to skin tears as well as injuries to muscles, joints and ligaments; however, injuries can be minimized with the use of individualized and sound exercise techniques (Dodd et al., 2004). Fatigue, poor physical work capacity and deconditioning are important considerations, especially in the frail elderly who have multiple diagnoses. The Valsalva maneuver must be avoided. Isometric exercises are safe, provided that the hold time is no more than 5–10 seconds, the standard isometric contraction. Blood pressure has been shown to be adversely affected by isometric contractions longer than 30 seconds in duration.
Aging patients who need an exercise program benefit from individualized instruction that is tailored to meet functional goals. Some individuals are fully cognitive and capable of engaging in standard strengthening and fitness exercises. Others do not have the same physical, cognitive or communicative abilities and, to be effective, the exercise program must be modified.
Monitoring response to exercise is requisite. This is achieved by observing and recording pulse rate, respiratory rate, perceived exertion and quality of movement. For example, asynchronous muscle contractions or obtaining full ROM for only the first 6 repetitions and not all 10 would be indicative of low quality of movement.
Blood pressure should be taken before, during and after exercise, especially in patients with known or suspected cardiovascular, cardiopulmonary or cerebrovascular disease. However, the repeated measurements with the use of a sphygmomanometer can become cumbersome in busy outpatient clinics and in home healthcare. A pulse oximeter is used to measure oxygen levels and may be helpful for establishing safe exercise parameters. Clinically, the talk test is beneficial. This is a simple safeguard that avoids overloading patients beyond capability by talking with them during the exercise routine. When overexercised, the patient will become dyspneic and be unable to talk in two- to three-word sentences.
Postexercise hypotension is a concern in patients who experience light-headedness or near-syncope, especially after endurance training. In these cases, further workup is necessary to rule out cardiac, cardiopulmonary or other potential causes of the problem. These symptoms may result from carotid sinus hypersensitivity when the pulse is taken at the carotid artery. Compression at the carotid sinus may send impulses to the vasomotor and cardioinhibitory centers in the medulla, resulting in hypotension (Ziegelstein, 2004).
Training considerations
To obtain optimal results, an exercise program for an aging adult should be prescribed based on the individual’s abilities and goals. When prescribing each exercise, the therapist should consider each exercise principle and include all components of an exercise prescription. These principles and components apply to all types of exercises, including those to improve aerobic capacity/endurance, muscle performance or balance. Exercises should be monitored and adjusted as the individual progresses to achieve the most favorable outcome.
Exercise can be performed with weights, bands, balls and with body weight alone using isometric, isotonic and isokinetic contractions. The overload principle is necessary but care must be taken to avoid excessive overload. Some patients with cognitive or communicative difficulties may benefit from gestures or ROM exercises, including passive, active assistive, active and resistive exercises, as well as proprioceptive neuromuscular facilitation. Physical contact may assist not only in attaining a desired movement but also in establishing a trusting rapport between patient and care provider. Also, the benefit of sensory stimulation to muscle activation has been recognized, especially in work with individuals with neurological conditions.
Functional activities done repeatedly, such as sit-to-stand 10 times, will not only strengthen muscles but also enhance coordination, endurance and motor learning. Neural adaptations will occur in the motor cortex and in the spinal level that facilitates activation of individual muscles and coordinates groups of muscles. Practice is important for skill acquisition (see Chapter 5).
Some patients have pathologies, for example chronic obstructive pulmonary disease, or are too deconditioned to effectively undergo typical exercise routines such as closed chain activities, progressive resistive exercise and standard aerobic programs; however, they may benefit from a graded circuit routine using a combination of chair exercises and, if possible, ambulatory activities. Sample circuit exercises are provided in Box 16.1. The speed and number of repetitions of these simple exercises can be increased or decreased according to the patient’s response to exercise. Walking exercises can also be added. Some individuals may only be able to exercise for 1 minute with this type of circuit routine, whereas others may be able to advance to 3–4 minutes. The talk test or perceived exertion are helpful for monitoring response to the activity. A rest of 1–5 minutes should be taken before repeating the routine. It is safe to start the routine again when the pulse rate has returned to the pre-exercise level. Exercise machines clearly have benefits for some patients. Weight-training units, bicycles, stair-steppers and rowing machines are all beneficial. As mentioned above, simple calisthenics and walking are mainstays in the exercise armamentarium for aging patients. Use of low weights at the ankles and wrists can increase the physical work carried out during simple walking exercises. Aquatic exercise is excellent for strengthening, conditioning and balance retraining, especially after joint replacement, back surgery or in those with painful arthritic joints (see Chapter 73).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







