Multiple Percutaneous Osteotomies and Fassier-Duval Telescoping Nailing of Long Bones in Osteogenesis Imperfecta
Paul W. Esposito
François Fassier
DEFINITION
Children with osteogenesis imperfecta (OI) and syndromes with congenital brittle bones sustain recurrent fractures and deformity, which cause chronic pain and limit their function.24, 25
Multiple percutaneous osteotomies and percutaneous telescoping intramedullary nailing can improve comfort and function with lower morbidity than previously was possible.
The severity of bone disease, fracture incidence, degree of deformity, and functional level of the patient, as well as the patient’s response to medical treatment, are more important in surgical decision making than the specific diagnostic type of OI or brittle bone disease.
ANATOMY
There is broad variation in anatomic findings in the different types of OI and other brittle bone diseases that resemble it.
Some children have blue sclera, obvious dentinogenesis imperfecta, triangular faces, and ligamentous laxity, but this varies greatly, even within the same family, and many affected children have none of these findings.
The defining characteristics of children with OI are a varying degree of bone fragility and recurrent fractures.
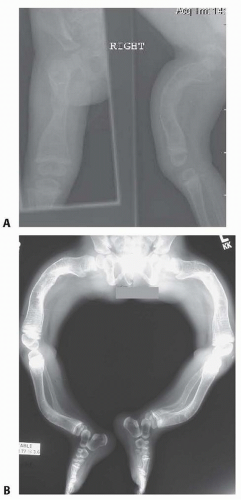
Progressive anterior bowing of the long bones is quite common, especially in children with moderate to severe involvement, even with early treatment with bisphosphonates (FIG 1).
PATHOGENESIS
OI is caused, in the great majority of cases, by dominant mutations in type I procollagen genes.
In the remaining cases, children may have brittle bone disease with a similar presentation and problems that are not caused by mutations in the type I procollagen genes.24, 25
The flexors, such as the gastrocnemius muscles and hamstrings, contribute to the progressive bowing.
Secondary joint contractures may be seen as a result of the long-standing deformities.
Juxta-articular bone deformities can mimic joint contractures, and extra-articular osteotomies frequently will allow full joint motion.
NATURAL HISTORY
Historically, children with very severe OI, especially Sillence type II, rarely survived infancy, and children with types III and IV had severe disability secondary to recurrent fractures, bone pain, and deformities.30, 31
Before bisphosphonate therapy was available, ambulation and even functional, comfortable sitting were difficult if not impossible for many children with severe forms of OI.
Even children with less severe forms of OI may have many significant fractures, which inhibit comfort, function, and quality of life.
Scoliosis and vertebral flexion fractures with secondary kyphosis are common.
Spondylolysis and spondylolisthesis are very common, especially in ambulatory children.11
Progressive craniocervical abnormalities such as basilar invagination, cranial settling, as well as C2 fractures can occur and are not necessarily related to the overall severity of the OI.
PATIENT HISTORY AND PHYSICAL FINDINGS
Findings vary greatly depending on the type and severity of OI. In addition, findings on physical examination may change dramatically as children respond to treatment with bisphosphonates.
Possible physical findings include blue sclera, triangular face, dentinogenesis imperfecta, joint laxity, bowing of the arms and legs, and flattening of the skull, especially in infants with severe involvement, but these findings vary greatly even within the same family, and many of the children have none of these classic physical findings.
Flexible flat feet, lax joints, and externally rotated lower extremities are quite common.
A variety of presentations are possible, and children with subtle forms of OI may appear totally normal on physical examination but present with multiple and recurrent fractures.
The classic triad of bone fragility, blue sclera, and deafness is rarely present in infancy.
IMAGING AND OTHER DIAGNOSTIC STUDIES
There is no specific test for OI. The diagnosis is based primarily on clinical and radiologic basis.
Plain radiographs are preferred as the initial study to evaluate children who have or may not have OI.
Full-length radiographs of both legs on the same cassette from the hips to the ankles are ideal to assess areas of fractures and degree of deformity.
Radiographs of the lower extremity should be performed with the patellas directly anterior and also with the legs maximally externally rotated. This helps assess the severity of the disease, can help predict risk of fracture, and is useful in preoperative planning for osteotomies and instrumentation (FIG 2).
Standardized posteroanterior (PA) and lateral spine radiographs demonstrate spinal fractures, scoliosis, spondylolysis, and spondylolisthesis.
Bone density (dual energy x-ray absorptiometry [DEXA]) scans, although not perfect, can be useful in monitoring changes in bone density, using age-matched Z-scores and consistently using the same techniques and machine type. The DEXA scan alone, however, cannot be used for diagnosis, especially in infants, for whom no standardized validated Z-scores have been established.
The child’s clinical course with regard to incidence of fracture and pain is a much more reliable indicator of successful medical treatment than a specific Z-score.
DIFFERENTIAL DIAGNOSIS
Child abuse
Metabolic bone disease (eg, hypophosphatasia, rickets)
Idiopathic juvenile osteoporosis
NONOPERATIVE MANAGEMENT
Early diagnosis and treatment with bisphosphonates has significantly improved the lives of children with OI and potentially other disorders.26 This treatment positively alters the mechanical properties of their bones, decreases their fracture rate and pain, and enhances their psychomotor development.16, 27
This improvement in bone density and strength often allows them to function at levels that previously were not possible by decreasing their bone fragility and pain.2, 6, 13, 16
Surgical treatment for these children is now possible, whereas previously in many cases, no surgical options existed because of the severity of their bone disease.
It has, however, been suggested that treatment with pamidronate may be related to delayed healing of osteotomies— but not fractures—in children with OI.20
It remains unclear whether the incidence of delayed healing will decrease with lower doses of bisphosphonates or discontinuing their use for a period of time postoperatively.20, 23
Casting, splinting, and bracing for many children with OI should be short-term temporizing measures only because residual deformities will not remodel, and osteoporosis is worsened by prolonged immobilization.
SURGICAL MANAGEMENT
Intramedullary fixation of long bones in children with OI required extensive soft tissue disruption with traditional techniques.32
Insertion of many telescoping and nontelescoping rods requires extensive exposure and arthrotomies for insertion, and the reoperation rate is high.3, 4, 6, 10, 34, 35
Principles of Surgical Treatment
Primary indications for surgical treatment include recurrent fractures, pain, and deformity.
These approaches should be considered, as children begin attempting to stand or crawl. There is no documented benefit to surgery performed before walking age.
There is no advantage to waiting until the child is older.
Surgical treatment should be considered in acute fracture with deformity, even with less severe OI.
Correct deformity and axial alignment.
Residual bowing does not correct with growth and predictably leads to further fracture.
As many involved, symptomatic bones should be corrected at one setting as can be safely accomplished.
Minimize soft tissue dissection and trauma.
Percutaneous technique provides more stability, less scarring, and earlier healing.
Minimize immobilization.
Light splints only
Early weight bearing and motion as symptoms allow
The role of bracing for long bones is not proven, and bracing may inhibit function.
Use telescoping intramedullary devices whenever possible.
Plating predictably leads to stress reaction, progressive deformity, and fracture (FIG 3A,B).
Use relatively small, flexible nails to share stress.
Excessively rigid nails may lead to disappearing bone (FIG 3C,D).
Do not remove nails electively.
Indications in forearm are more limited.
Fixation in the forearm is less predictable and has higher risks and rate of complications.
Instrumentation and bone quality are not optimal.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree