Fig. 5.1
Irreducible posterior dislocation of the left knee in an elderly male: AP and lateral X-rays from emergency presentation (a, b) and 8 weeks after open reduction and conservative management (orthosis immobilization and physical therapy) (c, d)
5.1.1 Clinical Signs and Emergency Procedures
The initial clinical evaluation of the patient is of utmost importance and must be carried out as soon as possible, depending on the overall status of the patient. The patient is usually in great pain, the knee is swollen (hemarthrosis) and very often deformed (if the dislocation has not been reduced prior to his arrival). The pulse must be checked distal to the knee, and the reduction procedures must be carried out immediately after observing the x-rays. It is important to mention that normal pulses, capillary refill or Doppler signal does not rule out eventual vascular injury [7].
The reduction is obtained by applying an axial (traction) force on the ankle while another doctor manipulates the proximal tibia in the appropriate direction. X-ray confirmation is mandatory, and immobilization in a long leg splint or trans-calcaneal extension is strongly advised.
Irreducible dislocations, open dislocations and prolonged ischemia are strong indicators for an emergency surgical procedure. Otherwise, MRI and clinical evaluation after 3–6 weeks from the trauma are needed in order to establish the surgical treatment. After the patient has overcome the acute phase, a proper clinical examination can be done which includes the Lachmann, anterior and posterior drawer and dial tests. These tests are specific to ligament injuries and can clearly demonstrate the grade of laxity and instability the knee has.
5.1.2 Patient Management
Multiple associated soft tissue injuries of the knee following dislocations are very hard to manage surgically and require a great deal of surgical skill and clinical experience. Depending on the structures that are affected, multiligamentary knee lesions can be resolved in different ways.
The ACL rupture is a definite indication for reconstruction, especially when associated with other instability issues of the knee. The reconstruction of the ACL was thoroughly discussed earlier on. The PCL is known to have intrinsic healing capabilities if properly managed. Thus, the bracing must include a method of pushing the tibia slightly anterior in order to allow for optimal healing parameters. If conservative PCL management is what we desire, an MRI investigation must be performed 4–6 weeks after immobilization in order to evaluate its condition.
The MCL ligament usually heals by itself after 4–6 weeks of stiff bracing. In certain ACL/PCL/MCL injuries, it is recommended to delay the surgical procedure of ACL and/or PCL reconstruction until after the eventual healing of the MCL. In unfortunate cases, the MCL must require reconstruction procedures to be carried out alongside with the other injured ligaments. Injuries that associate ACL and PCL with posterolateral corner tears must be surgically addressed and repaired between the 2nd and 3rd week after the trauma. This allows for optimal capsular closure and arthroscopic repair for the other affected structures as well as the posterolateral corner (Fig. 5.2).
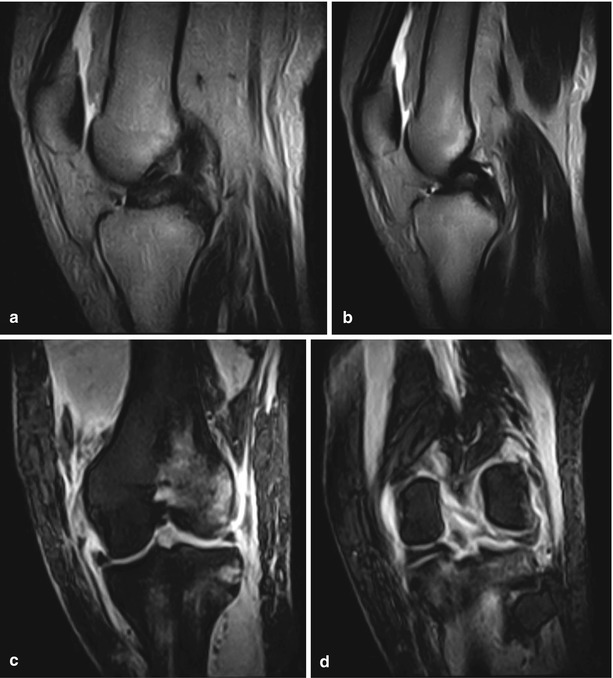
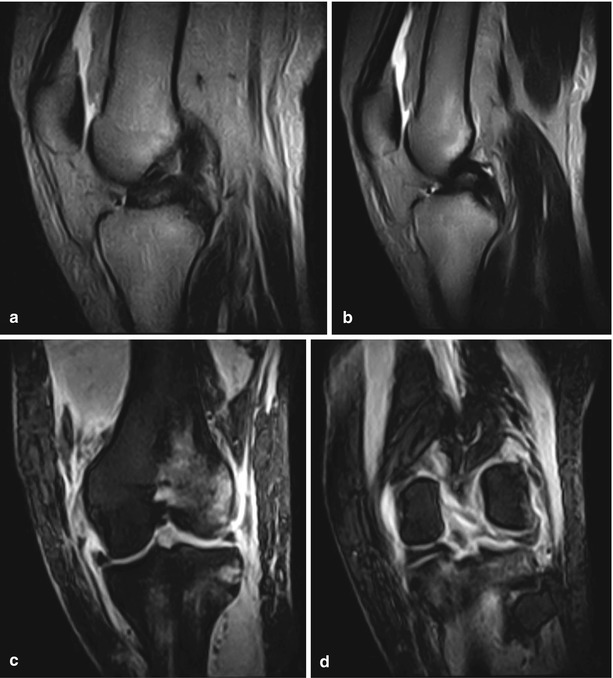
Fig. 5.2
Left knee MRI of a young male patient with multiligamentary injury: sagittal T2 with torn ACL at the femoral insertion (a) and PCL at the tibial insertion (b); coronal views showing complete (grade III) MCL rupture from the femoral insertion, bone edema on the lateral femoral condyle (c) and tibial plateau and ruptured PCL (d)
5.2 Posterior Cruciate Ligament (PCL) Tears
PCL tears represent 5–37 % of all ligament injuries, being less frequent than ACL tears but more difficult to handle with. The incidence in a general population was measured at 3 % [8]. They can occur in multiligamentary knee trauma [9, 10] or in athletes frequently in a hyperflexion movement [11, 12]. There has been great controversy regarding the treatment of PCL tears. Some author suggest that in case of multiligamentary association, the PCL should be treated surgically [13–17] and others believe that conservative treatment leads to acceptable results [14].
5.2.1 Examination
PCL tears lead to posterior knee laxity, sensation of uncontrolled hyperflexion and sometimes anterior knee pain. This type of injury translates into a highly positive posterior drawer test in knee flexion [3, 5, 7, 33]. According to the posterior laxity the knee has during the posterior drawer test, Harner and Hoher have established a classification for PCL tears. Grade I tears correspond to 0–5 mm of laxity, grade II tears present 5–10 mm of posterior tibial translation and grade III have more than 10 mm of posterior stress laxity [18]. Of course MRI and bilateral knee stress x-rays still carry a very important role in the imaging diagnosis of PCL rupture. For a good treatment to be offered, all of the other possibly associated ligament tears should be identified.
5.2.2 Treatment
Conservative treatment is considered a good option for PCL tears if they are not associated with other ruptured ligaments, whether the rupture is acute or chronic, exception being only grade III isolated ruptures in young athletes. Surgical treatment is an indication for combined ligamentary lesions that include PCL tears.
The PCL can be reconstructed using either a single bundle (SB) or double bundle (DB) technique. There have been many studies that compared the outcomes of both procedures, but there has been insufficient strong proof to confirm that DB technique is a clear advantage regarding rehabilitation and knee kinematics over the SB technique [19–23].
Most of the authors that use the SB technique use the footprint of the antero-lateral bundle to place the femoral insertion of the reconstructed PCL [24]. This footprint is located between the 9 and 12 o’clock positions looking at the notch [25]. Fifty articles on PCL reconstruction were reviewed and the reported positions for femoral insertion were between 10:00 and 11:00 o’clock, and from 2.5 to 13 mm depth regarding the edge of the articular cartilage [24].
The main advantage of the DB technique is that it decreases posterior tibial translation and laxity, unlike the SB that has had somewhat low results regarding this issue [20, 26–28]. The femoral footprint is usually left in place in order to allow for a proper fixation of the neoligament. A posteromedial portal is usually established under arthroscopic guidance and the PCL guide is placed on the tibial footprint of the PCL. With the aid of the guide, the two tunnels (AL and PM) are drilled, paying absolute caution to the neurovascular structures. The proper position of the tunnels is confirmed with an AP fluoroscopic view. The AL (1 o’clock) and PM (4 o’clock) femoral tunnels are drilled with the knee in 130° and 110° flexion. Graft positioning is done for the AL bundle first and then for the PM bundle taking note that proper tension should be performed before fixation.
5.2.3 Conclusion
Although the results of PCL reconstruction using the SB and DB techniques are still very controversial, it is safe to say that both can be used and give good results, given that the patient is chosen carefully and the procedure is performed with no complications. Another influencing factor is the postoperative rehabilitation which must be carried out by a specialized physiotherapist while taking into account for the case particularities and eventual other morbidities.
Even if PCL reconstruction is achieved, the patient must be aware that it cannot eliminate the posterior laxity that was once offered by the original ligament. Associated instabilities must be addressed before the PCL reconstruction in order to ensure good functional outcomes (Figs. 5.3 and 5.4).
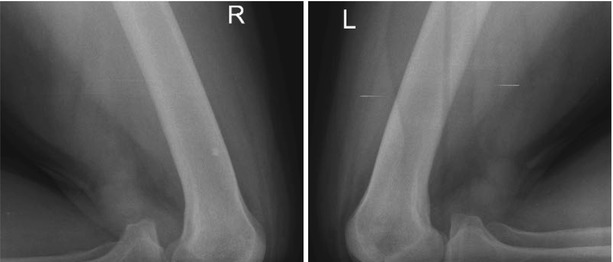

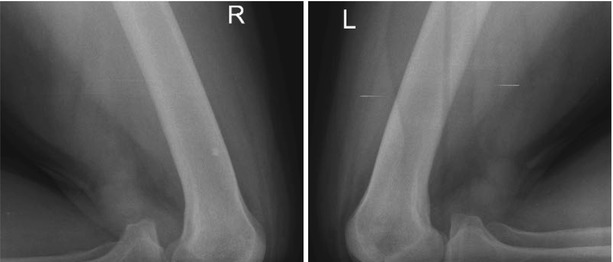
Fig. 5.3
An adult male patient with positive posterior drawer – stress X-ray of the right knee, suggestive of PCL injury

Fig. 5.4
A middle aged male patient with residual laxity and a history of distal femoral fracture. Positive posterior drawer – stress X-ray of the right knee suggestive of PCL insufficiency. KT-1,000 examination
5.3 Multiligamentary Surgical Repair
5.3.1 Posteromedial Corner
The posteromedial corner is made up of three ligaments that provide this portion of the knee with static and dynamic stability. These three ligaments are: the superficial medial collateral ligament, the posterior oblique ligament and the deep medial collateral ligament.
LaPrade et al. described an anatomic reconstruction technique of the proximal and distal avulsions of the superficial medial collateral ligament and the posterior oblique ligament using two separate grafts. Their approach was through an incision that expands from the medial side of the patella and continues 7–8 cm distal to the joint line, down the tibia. Once they found the attachment and insertion points of these two structures tunnel were drilled with the aid of guiding pins. Graft sizes should be 16 cm for the superficial MCL and 12 cm for the posterior oblique ligament. Femoral fixation was obtained through bioabsorbable screws. Then the posterior oblique ligament is fixed on the tibia with the knee in full extension and the superficial MCL with the knee in 20° of flexion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








