Fig. 5.1
Main locations of osteochondral ankle defects
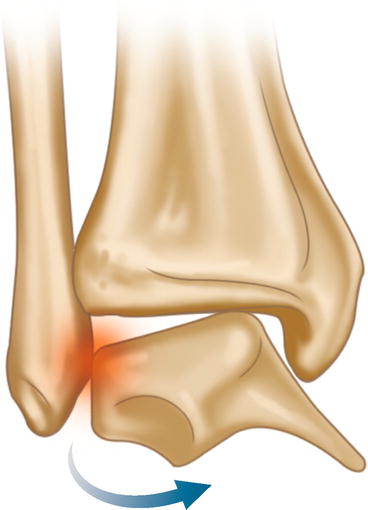
Fig. 5.2
Shear mechanism of injury in lateral osteochondral ankle defects
5.4 Clinical Appearance
A differentiation has to be made between acute and chronic conditions. In acute conditions, symptoms of osteochondral ankle defects are similar to those of acute ankle injuries. They include lateral or medial ankle pain, functio laesa and swelling. In patients with an isolated ligamentous ankle injury, these symptoms usually resolve after functional treatment within 2–3 weeks. If symptoms do not resolve after 3–6 weeks, an osteochondral defect of the talus should be suspected. These patients typically present with persisting symptoms and limited range of motion.
Locking and catching are symptoms of a displaced fragment. In most patients with a non-displaced lesion after supination trauma, acute symptoms cannot be distinguished from soft tissue damage.
Chronic lesions classically present as deep lateral or medial ankle pain associated with weight-bearing. Reactive swelling and stiffness can be present, but absence of swelling, locking or catching does not rule out an osteochondral defect. Recognisable pain on palpation is typically not present in these patients. Some patients have a diminished range of motion. See Table 5.1. Differential diagnoses are listed in Table 5.2.
Table 5.1
Possible symptoms
Lateral or medial ankle pain |
Functio laesa |
Swelling |
Locking |
Catching |
Deep pain on weight-bearing |
Stiffness |
Diminished range of motion |
Typical: no recognisable pain on palpation |
Table 5.2
Differential diagnoses
Posttraumatic synovitis |
Osteochondral defect of the tibial plafond |
Sinus tarsi syndrome |
Os trigonum |
Ligament laxity |
Peritendinitis |
Osteoarthritis |
Osteoid osteoma |
Avascular necrosis of the talus |
Damaged talar cartilage is responsible for pain during weight-bearing. It is probably the result of edge-loading by the tibia on the cartilage rim of the defect and the subchondral bone underneath. Due to the convex nature of the talus, the edges of the mainly circular defect are more heavily loaded than usual. Part of the healthy cartilage is gone, and the remaining cartilage has to carry the weight transmitted by the tibia. Nerve endings in the subchondral bone in the rim of the defect or underneath the defect are excitated by the increased loading. Purpose of the treatment is to diminish edge-loading, destroying the mechanism that is responsible for increased local hydraulic pressure onto the subchondral area below the defect.
5.5 Diagnosis
After thorough history taking and physical examination, routine radiographs of the ankle are made consisting of weight-bearing anteroposterior, mortise and lateral views of both ankles.
The radiographs may show an area of detached bone, surrounded by radiolucency (Fig. 5.3). Initially, the damage might be too small to be visualised on routine X-ray. By repeating the images in a later stage, the abnormality sometimes becomes apparent.


Fig. 5.3
Radiograph: radiolucency of medial talar dome indicating an osteochondral defect
A heel-rise view with the ankle in a plantarflexed position may reveal a posteromedial or a posterolateral defect [21]. A bone scan can differentiate between a symptomatic lesion and an asymptomatic lesion. MRI is often used for detection of these lesions. Computed tomography is useful for defining the exact size and location of the lesion and is therefore valuable for preoperative planning (Figs. 5.4 and 5.5).

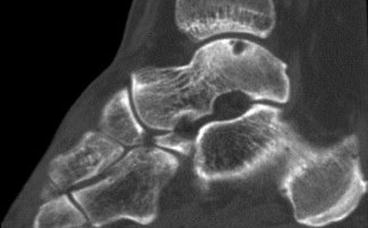

Fig. 5.4
CT scan of a lateral osteochondral defect, coronal reconstruction
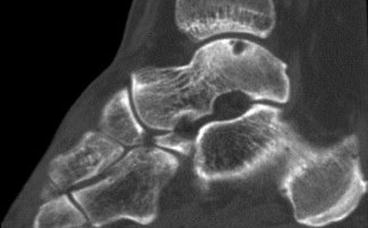
Fig. 5.5
CT scan of a medial osteochondral defect, sagittal reconstruction
5.6 Classification and Staging
In 1959, Berndt and Harty suggested a classification system for staging the lesions at the time of surgery based on plain radiographs of the ankle. In grade I, there is local compression of the cartilage and subchondral bone, and usually, there are no radiographic findings. In grade II, there is an avulsion or partial detachment of the osteochondral fragment, but the main part is still attached to the talus. In grade III, there is complete avulsion of an osteochondral fragment, without any displacement. In grade IV, the osteochondral fragment is completely detached and displaced inside the ankle joint (Table 5.3 and Fig. 5.6). Later, classification systems [22] based on CT [23] (Table 5.4), MRI [24] (Table 5.5) and arthroscopic findings were made [25] (Table 5.6). The use of these classification systems is questionable since none of the systems are duly related to the current treatment options [26].
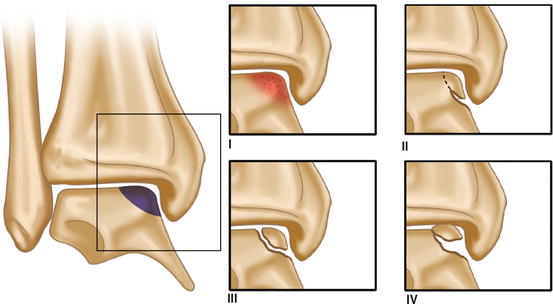
Table 5.3
Berndt and Harty (1959)
Stage I | A small compression fracture |
Stage II | Incomplete avulsion of a fragment |
Stage III | Complete avulsion of a fragment without displacement |
Stage IV | Displaced fragment |
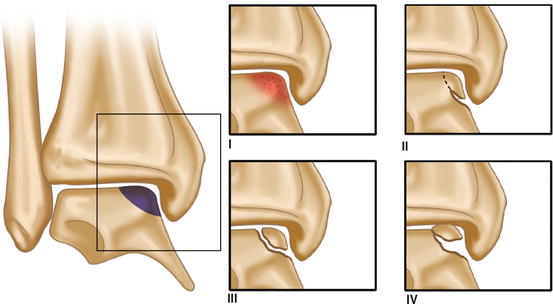
Fig. 5.6
Berndt and Harty classification of osteochondral ankle defects
Table 5.4
Talus OCD CT classification of Ferkel and Sgaglione
Stage I | Intact roof/cartilage with cyst lesion beneath |
Stage II/A | Cyst lesion with communication to the surface |
Stage II/B | Open surface lesion with overlying fragment |
Stage III | Non-displaced fragment with lucency underneath |
Stage IV | Displaced fragment |
Table 5.5
Talus OCD MRI classification of Hepple et al.
Stage I | Articular cartilage injury only |
Stage II/A | Cartilage injury with bony fracture and oedema (flap, acute) |
Stage II/B | Cartilage injury with bony fracture and without oedema (chronic) |
Stage III | Detached, non-displaced bony fragment (fluid rim beneath fragment) |
Stage IV | Displaced fragment, uncovered subchondral bone |
Stage V | Subchondral cyst present |
Table 5.6
Ferkel/Cheng rating: arthroscopic surgical grade based on status of articular cartilage
Grade A | Smooth, intact, but soft cartilage |
Grade B | Rough surface |
Grade C | Fibrillations/fissures |
Grade D | Flap present or bone exposed |
Grade E | Loose, undisplaced fragment |
Grade F
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|




