Monoblock Tapered Titanium Stems for Femoral Revision
Brett R. Levine
Case Study
A 65-year-old female presents to the emergency room with left hip pain after a slip and fall while climbing the stairs. The patient was unable to bear weight on the left lower extremity after the fall and was brought into the emergency room for assessment. She was 2 years status post a primary total hip arthroplasty (THA) on the left side. Prior to the fall she maintained an active lifestyle including biking, swimming, and hiking on a regular basis. On physical examination the patient was neurovascularly intact, with a shortened and externally rotated left lower extremity. Radiographs revealed a displaced Vancouver B2 fracture of the proximal femur (Fig. 121.1). The patient elected to proceed with revision surgery and concomitant open reduction and internal fixation of the left femur fracture.
Key Points, Pearls, and Pitfalls
Preoperatively template to determine anchor point of the stem and appropriate length needed for the revision procedure at hand (1).
In early experience take intraoperative radiograph of trial components to assure correct sizing, adequate implant alignment, and relationship of limb lengths.
Mark depth of penetration on the trial stem and translate to the final implant to assure that the component settles to a similar level (final component has eight splines vs. trials with four splines).
Use tapered reamers by hand to start. May complete reaming under power, but beware to not stop reamer and get incarcerated distally as this can lead to spiral fractures of the femur.
Introduction
The number of revision THAs being performed annually continues to increase as the population with prior hip replacements ages and younger patients with more demanding lifestyles are undergoing primary surgeries (2,3,4). Femoral component failure may occur in association with several possible etiologies, including sepsis, aseptic loosening, periprosthetic fracture, recurrent instability, trunnion corrosion, and component breakage. In the United States a review of revision THAs in 2005–2006 found instability (22.5%), mechanical loosening (19.7%), and infection (14.8%) to be the most common causes necessitating repeat surgery (1). More recently, although not quantified as of yet, a rise in revision surgery secondary to corrosion, articular surface debris, and adverse local tissue reactions has occurred. Regardless of the etiology of failure, femoral bone loss is a difficult problem to solve during revision THA surgery and if not respected may be a detriment to long-term survivorship.
Specific factors that may compromise the femoral bone stock include particulate-induced osteolysis, stress-shielding, femoral remodeling around the implants, adverse local tissue reactions, and damage to the remaining bone during component/cement extraction (5).
Specific factors that may compromise the femoral bone stock include particulate-induced osteolysis, stress-shielding, femoral remodeling around the implants, adverse local tissue reactions, and damage to the remaining bone during component/cement extraction (5).
There are many options to manage femoral bone loss in revision THA with no one modality representing an absolute gold standard. Component choices are often based upon the quantity and location of the bone loss as well as the patients’ bony anatomy and bone quality (6,7,8). Overall goals include achieving a stable prosthesis with fixation as proximal as possible in the femur to prevent greater areas of stress shielding and preserve future bone stock. However, in extreme cases fixation will need to occur distal to weakened areas to assure long-term success. Furthermore, while distal fixation is important a greater emphasis for proximal support of the femoral stem is coming to light in the face of component fretting-corrosion and implant fractures. In such cases greater stress is being borne by the proximal unsupported portion of the stem above a well-fixed distal segment, setting up the possibility of fatigue fracture.
Design Rationale
In revision THA it is often necessary to bypass the proximal femur and secure fixation into the distal extent of the bone at the level of the isthmus or beyond. This concept of distal stem fixation was developed and popularized by Wagner (9,10). The Wagner SL revision femoral component (Zimmber GmbH, Winterthur, Switzerland) maintains a tapered design with longitudinal flutes and is available in multiple stem lengths (Fig. 121.2A,B). The implant is fabricated from a titanium alloy, Ti6-Al7-Nb, and is extensively grit-blasted over the entire surface of the component. Standard (34 mm) and high offset (44 mm) options are available in varying lengths and diameters, from 185 to 385 mm (although the 225, 265, and 305 mm are more commonly used) and from 14 to 25 mm, respectively. The implant has a two-degree taper with a circular cross section with eight longitudinal ridges evenly distributed around the circumference of the component. Proximally the component incorporates two holes to aid in reattachment of the greater trochanter as needed.
The circular nature of the implant allows for the simple adjustment of component version to help optimize stability and decrease the risk of dislocation. However, surgeons should keep in mind that a recent finite element analysis found an increase in prosthetic stress from 5% to 15% with the standard and high offset stems when anteversion was increased from 4 to 14 degrees (11). This may be an important consideration when utilizing a high offset modular stem with significant anteversion dialed into the component. The tapered nature of the stem affords axial stability, while the longitudinal ridges provide rotational fixation. The conical shape of the stem and reamer preparation yields a large contact area between the host bone and the implant. This intimate contact translates into an even transmission of load and uniform stress distribution from the prosthesis to the surrounding bone. The ultimate goal for these long, tapered stems is to achieve as proximal fixation as possible and as distal as deemed necessary.
Indications
With modern trends toward utilizing tapered stems for primary THA, it is not irrationale to move toward similar style stems for revision procedures as well. Therefore, despite the
original indications being reserved for severe proximal bone loss (9,10,12,13), the Wagner technique has expanded to treat lower grade proximal femoral defects purely due to the familiarity of inserting a tapered style stem. Routinely as part of the preoperative planning for revision THA the femoral bone defects are classified using the Paprosky classification system (14). While better suited to treat more severe femoral defects the Wagner SL stem can be used in Paprosky type 1 and 2 femoral defects. More commonly this conical revision stem is utilized in type 3A and 3B femoral defects or in cases with canal diameters greater than 18 mm (Fig. 121.3A–C). As long as there remains sufficient cortical bone within the femoral isthmus the Wagner SL revision stem is a viable option in treating these difficult femoral defects. While cylindrical distal fixation stems typically require 4 cm of isthmus to be successful, the author suggests using the Wagner SL stem with a minimum of 2 cm of isthmus to achieve optimal results. Furthermore this stem is an excellent reconstruction option for the management of severe proximal femoral defects with favorable load transmission and version adjustment options (15).
original indications being reserved for severe proximal bone loss (9,10,12,13), the Wagner technique has expanded to treat lower grade proximal femoral defects purely due to the familiarity of inserting a tapered style stem. Routinely as part of the preoperative planning for revision THA the femoral bone defects are classified using the Paprosky classification system (14). While better suited to treat more severe femoral defects the Wagner SL stem can be used in Paprosky type 1 and 2 femoral defects. More commonly this conical revision stem is utilized in type 3A and 3B femoral defects or in cases with canal diameters greater than 18 mm (Fig. 121.3A–C). As long as there remains sufficient cortical bone within the femoral isthmus the Wagner SL revision stem is a viable option in treating these difficult femoral defects. While cylindrical distal fixation stems typically require 4 cm of isthmus to be successful, the author suggests using the Wagner SL stem with a minimum of 2 cm of isthmus to achieve optimal results. Furthermore this stem is an excellent reconstruction option for the management of severe proximal femoral defects with favorable load transmission and version adjustment options (15).
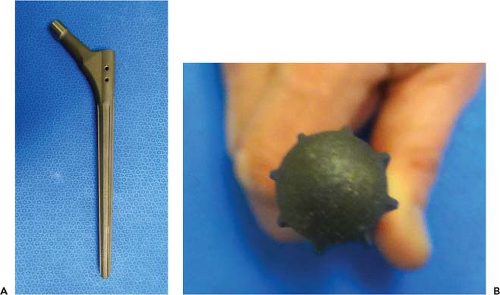 Figure 121.2. View of the Wagner SL revision stem in its entirety (A) with a close-up view (B), depicting the conical shape of the implant as well as the extent of the eight longitudinal ridges. |
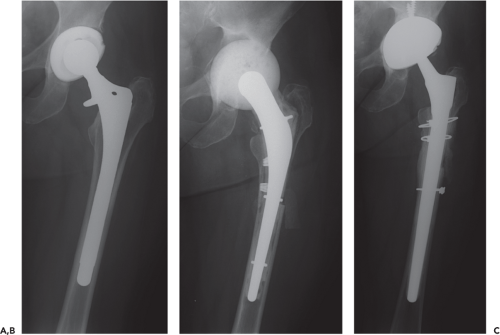 Figure 121.3. Case example (A) of an infected THA treated with a two-stage exchange. After component and spacer removal (B)
Get Clinical Tree app for offline access
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree


|






